Abstract
We studied the relation between adherence to imatinib measured with microelectronic monitoring systems and the probabilities of losing a complete cytogenetic response (CCyR) and of imatinib failure in 87 CCyR chronic myeloid leukemia patients receiving long-term therapy. We included in our analysis the most relevant prognostic factors described to date. On multivariate analysis, the adherence rate and having failed to achieve a major molecular response were the only independent predictors for loss of CCyR and discontinuation of imatinib therapy. The 23 patients with an adherence rate less than or equal to 85% had a higher probability of losing their CCyR at 2 years (26.8% vs 1.5%, P = .0002) and a lower probability of remaining on imatinib (64.5% vs 90.6%, P = .006) than the 64 patients with an adherence rate more than 85%. In summary, we have shown that poor adherence is the principal factor contributing to the loss of cytogenetic responses and treatment failure in patients on long-term therapy.
Introduction
Lack of adherence to oral therapy for chronic diseases is a well-recognized problem.1-4 Several recent studies have shown that lack of adherence to imatinib is frequent and has a significant impact on the degree of response to therapy obtained by the patient.5,6 For example, a Belgian study found that one-third of 169 patients were nonadherent to imatinib and only 14% took all of their prescribed dose.5 In this study, nonadherence was associated with reduced clinical response. We recently reported that 26% of the patients on long-term imatinib therapy had an adherence rate lower than 90% and 14% had a rate lower than 80%.6 In our study, multivariate analysis identified adherence and the level of expression of the molecular transporter hOCT1 as the only independent predictors for achieving major molecular response (MMR)
We now present the follow-up data, where we investigated the relation between adherence to imatinib and the probabilities of losing a complete cytogenetic response (CCyR) and of imatinib failure in patients receiving long-term therapy.
Methods
Patient variables and treatment
Between April 2008 and February 2009, we measured the adherence to imatinib in 87 (Table 1) consecutive chronic-phase chronic myeloid leukemia patients who had received imatinib 400 mg/day as first-line therapy for a median of 59.7 months before enrollment (www.clinicaltrials.gov, #NCT00632255).6 Adherence levels were monitored during a 3-month period using a medication event monitoring system as previously described.6 Briefly, a medication event monitoring system is an electronic device fitted into the cap of a normal looking medication bottle that automatically records each time the bottle is opened. Medication event monitoring systems are considered the “gold standard” for measuring adherence.1,2,9,10 After the 3-month monitoring period, the patients were followed subsequently for a median of 19 months (range, 14-24 months). Data from the patients were censored in March 2010, when our previous work was published, to ensure that the results of this study were not influenced by possible changes in a patient's behavior. The study was approved by the Imperial College London Institutional Review Board and the Medicines and Healthcare Products Regulatory Agency.
Patient characteristics and 24-month probabilities of cytogenetic relapse and EFS
| Variables . | n . | 24-month probability of losing the CCyR, % . | 24-month probability of EFS, % . |
|---|---|---|---|
| Variables at diagnosis | |||
| Sex | P = .41 | P = .12 | |
| Male | 49 | 10.3 | 79.0 |
| Female | 38 | 5.8 | 90.9 |
| Age | P = .55 | P = .20 | |
| ≤ 45 y | 42 | 9.6 | 76.6 |
| > 45 y | 45 | 6.9 | 89.7 |
| Sokal risk group | P = .13 | P = .79 | |
| Low | 33 | 6.6 | 85.8 |
| Intermediate | 32 | 3.4 | 85.3 |
| High | 22 | 17.9 | 79.7 |
| Hemoglobin | P = .82 | P = .77 | |
| ≤ 115 g/L | 40 | 8.1 | 81.9 |
| > 115 g/L | 47 | 7.3 | 83.7 |
| Leukocytes | P = .95 | P = .99 | |
| ≤ 140 × 109/L | 44 | 7.2 | 85.1 |
| > 140 × 109/L | 43 | 7.1 | 82.3 |
| BCR-ABL1 transcript type | P = .72 | P = .43 | |
| e14a2 | 40 | 10.9 | 89.0 |
| e13a2 | 33 | 9.4 | 74.6 |
| e13a2 and e14a2 | 14 | 4.6 | 75.0 |
| hOCT1 transcript level* | P = .30 | P = .51 | |
| ≤ 0.16 | 30 | 11.2 | 81.1 |
| > 0.16 | 30 | 3.4 | 86.7 |
| MDR-1 polymorphism | P = .82 | P = .79 | |
| C/C | 75 | 10.1 | 82.3 |
| T/C | 12 | 7.9 | 80.2 |
| Early molecular response† | 55 | P = .08 | P = .13 |
| Yes | 32 | 4.1 | 92.9 |
| No | 15.0 | 78.0 | |
| Baseline response | P = .0006 | P = .0007 | |
| CCyR and no MMR | 34 | 21.1 | 67.5 |
| MMR | 53 | 0 | 94.4 |
| On study variables | n | ||
| Age | P = .18 | P = .03 | |
| ≤ 50 y | 42 | 12.5 | 74.7 |
| > 50 y | 45 | 4.6 | 91.7 |
| Weight | P = .57 | P = .14 | |
| ≤ 74 kg | 47 | 6.5 | 90.9 |
| > 74 kg | 40 | 10.4 | 75.5 |
| Imatinib plasma level‡ | P = .98 | P = .80 | |
| ≤ 1 μg/mL | 43 | 6.8 | 86.7 |
| > 1 μg/mL | 41 | 7.0 | 83.9 |
| Adherence rate§ | P < .0001 | P = .0002 | |
| > 85% | 69 | 1.4 | 91.4 |
| ≤ 85% | 18 | 36.3 | 54.2 |
| Dose of imatinib | P = .73 | P = .79 | |
| 400 mg/day | 55 | 7.7 | 81.6 |
| > 400 mg/day | 32 | 9.2 | 87.1 |
| Variables . | n . | 24-month probability of losing the CCyR, % . | 24-month probability of EFS, % . |
|---|---|---|---|
| Variables at diagnosis | |||
| Sex | P = .41 | P = .12 | |
| Male | 49 | 10.3 | 79.0 |
| Female | 38 | 5.8 | 90.9 |
| Age | P = .55 | P = .20 | |
| ≤ 45 y | 42 | 9.6 | 76.6 |
| > 45 y | 45 | 6.9 | 89.7 |
| Sokal risk group | P = .13 | P = .79 | |
| Low | 33 | 6.6 | 85.8 |
| Intermediate | 32 | 3.4 | 85.3 |
| High | 22 | 17.9 | 79.7 |
| Hemoglobin | P = .82 | P = .77 | |
| ≤ 115 g/L | 40 | 8.1 | 81.9 |
| > 115 g/L | 47 | 7.3 | 83.7 |
| Leukocytes | P = .95 | P = .99 | |
| ≤ 140 × 109/L | 44 | 7.2 | 85.1 |
| > 140 × 109/L | 43 | 7.1 | 82.3 |
| BCR-ABL1 transcript type | P = .72 | P = .43 | |
| e14a2 | 40 | 10.9 | 89.0 |
| e13a2 | 33 | 9.4 | 74.6 |
| e13a2 and e14a2 | 14 | 4.6 | 75.0 |
| hOCT1 transcript level* | P = .30 | P = .51 | |
| ≤ 0.16 | 30 | 11.2 | 81.1 |
| > 0.16 | 30 | 3.4 | 86.7 |
| MDR-1 polymorphism | P = .82 | P = .79 | |
| C/C | 75 | 10.1 | 82.3 |
| T/C | 12 | 7.9 | 80.2 |
| Early molecular response† | 55 | P = .08 | P = .13 |
| Yes | 32 | 4.1 | 92.9 |
| No | 15.0 | 78.0 | |
| Baseline response | P = .0006 | P = .0007 | |
| CCyR and no MMR | 34 | 21.1 | 67.5 |
| MMR | 53 | 0 | 94.4 |
| On study variables | n | ||
| Age | P = .18 | P = .03 | |
| ≤ 50 y | 42 | 12.5 | 74.7 |
| > 50 y | 45 | 4.6 | 91.7 |
| Weight | P = .57 | P = .14 | |
| ≤ 74 kg | 47 | 6.5 | 90.9 |
| > 74 kg | 40 | 10.4 | 75.5 |
| Imatinib plasma level‡ | P = .98 | P = .80 | |
| ≤ 1 μg/mL | 43 | 6.8 | 86.7 |
| > 1 μg/mL | 41 | 7.0 | 83.9 |
| Adherence rate§ | P < .0001 | P = .0002 | |
| > 85% | 69 | 1.4 | 91.4 |
| ≤ 85% | 18 | 36.3 | 54.2 |
| Dose of imatinib | P = .73 | P = .79 | |
| 400 mg/day | 55 | 7.7 | 81.6 |
| > 400 mg/day | 32 | 9.2 | 87.1 |
Samples were not available in 27 patients.
Early molecular response is defined as having achieved a 1-log reduction (BCR-ABL1/ABL1 ratio ≤ 10%) by 3 months.6-8
In 3 patients, the trough plasma level was not available.
We explored different cutoff levels for the adherence rate. In all cases, the patients in the group with the lower adherence rate were more likely to lose their CCyR during the follow-up, namely, ≤ 80 vs > 80 (54.5 vs 2, P < .0001), ≤ 85 vs > 85 (36.3 vs 1.4, P < .0001), ≤ 90 vs > 90 (26.9 vs 1.6, P = .0002), and ≤ 95 vs > 95 (24.5 vs 0, P = .0001). We use a multivariate Cox model to choose the better cutoff, which was 85. The adherence rate also predicted for loss of CCyR when considered as a continuous variable (RR = 1.05; P = .0001).
Laboratory assessments
BCR-ABL1 transcripts were measured in the blood at 6- to 12-week intervals as previously described.6 Trough imatinib plasma levels, levels of hOCT1, and the polymorphism 1236C → T in ABCB1 were assessed as previously reported.6,11,12 Cytogenetic relapse (loss of CCyR) was defined by the detection of one or more Ph-positive marrow metaphases, confirmed by a second test. Bone marrow examination was triggered by a rise in BCR-ABL1 transcript numbers to a level consistent with cytogenetic relapse.13,14
Statistical methods
The probability of event-free survival (EFS) (the reverse of imatinib failure) was calculated using the Kaplan-Meier method. To define imatinib failure the event was death from any cause, progression from chronic phase, loss of complete hematologic response, loss of CCyR, or imatinib discontinuation on account of unacceptable toxicity or inadequate response.14 The probability of cytogenetic relapse was calculated using the cumulative incidence procedure. Univariate and multivariate analyses were performed as described elsewhere.6
Results and discussion
As previously reported,6 the median adherence rate was 97.6% (range, 24%-103.8%). In 23 (26.4%) patients, adherence was less than or equal to 90% (median, 76%) and in 18 (20.7%) less than or equal to 85% (median, 73.8%). During follow-up, 7 (8%) patients lost their CCyR (6 of whom became > 35% Ph-positive before alternative therapy could be commenced) and 12 (13.8%) discontinued the imatinib therapy (7 resulting from loss of CCyR and 5 resulting from side effects).
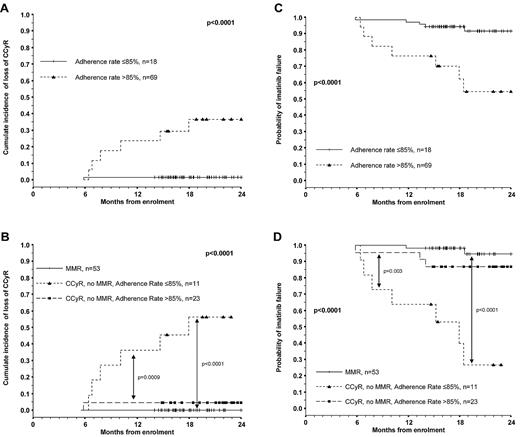
We performed univariate analysis to identify factors associated with loss of CCyR and with EFS (Table 1). The 18 patients with an adherence rate less than or equal to 85% had a higher probability of losing their CCyR than the 69 patients with an adherence rate more than 85%, namely, 36.3% versus 1.4% (P < .0001). None of the 57 patients with an adherence rate more than 95% lost their CCyR (P = .0001). Patients who were in MMR at the beginning of the study had a significantly lower probability of losing their CCyR by the end of follow-up (Table 1; Figure 1). Multivariate analysis identified an adherence rate less than or equal to 85% (relative risk [RR] = 27.8, P = .002) and never having achieved a MMR (RR = 14.9, P = .01) as the only 2 independent predictors for loss of CCyR.
Two-year probability of losing the CCyR and imatinib failure (EFS) according to the adherence rate and to the combination of adherence and the prior achievement of MMR. The 18 patients with an adherence rate ≤85% had higher 2-year probability of both losing their CCyR (A; 36.3% vs 1.4%, P < .0001) and of failing imatinib therapy (C; 54.4% vs 91.4%, P = .0002) than the 69 patients with an adherence rate >85%. The 53 patients who had achieved MMR at the moment of enrollment had a similar 2-year probability of losing their CCyR during follow-up (B) and a 2-year EFS (D) to that of the 23 patients who were not in MMR at enrollment but had an adherence rate >85% (0% vs 4.3%, P = .31; and 94.4% vs 86.1%, P = .14). However, the 11 patients who were not in MMR at the moment of enrollment and had an adherence rate ≤85% had a significantly higher probability of losing their CCyR (54.5%) and lower EFS (28.3%) (B,D).
Two-year probability of losing the CCyR and imatinib failure (EFS) according to the adherence rate and to the combination of adherence and the prior achievement of MMR. The 18 patients with an adherence rate ≤85% had higher 2-year probability of both losing their CCyR (A; 36.3% vs 1.4%, P < .0001) and of failing imatinib therapy (C; 54.4% vs 91.4%, P = .0002) than the 69 patients with an adherence rate >85%. The 53 patients who had achieved MMR at the moment of enrollment had a similar 2-year probability of losing their CCyR during follow-up (B) and a 2-year EFS (D) to that of the 23 patients who were not in MMR at enrollment but had an adherence rate >85% (0% vs 4.3%, P = .31; and 94.4% vs 86.1%, P = .14). However, the 11 patients who were not in MMR at the moment of enrollment and had an adherence rate ≤85% had a significantly higher probability of losing their CCyR (54.5%) and lower EFS (28.3%) (B,D).
The median adherence rate in the 12 patients who eventually failed imatinib therapy was significantly lower than that of the patients who continued on therapy (78.1% vs 97.8%, P = .02). Patients with an adherence rate less than or equal to 85% had a significantly lower EFS than the adherent patients (54.4% vs 91.4%, P = .0002). Again, we performed univariate (Table 1) and multivariate analysis to identify prognostic factors for imatinib failure. An adherence rate less than or equal to 85% (RR = 0.22, P = .01) and having failed to achieve an MMR (RR = 0.14, P = .15) were the only independent predictors for EFS.
The multivariate analysis identified adherence rate and the degree of molecular response as the only independent predictors for loss of CCyR and imatinib failure. Figure 1 shows the 2-year probabilities of loss of CCyR (Figure 1B) and EFS (Figure 1D) according to the combination of both variables. The 53 patients who started the study in MMR fared well, with a 2-year probability of losing the CCyR of 0% and an EFS of 94.4%. We have previously shown that patients who achieve MMR are less likely to lose their CCyR15 and that the achievement of MMR depends on the adherence to imatinib therapy and, to a lesser extent, on ill-defined intrinsic biologic factors, such as higher expression of hOCT1.6 It is impossible to establish the relative contributions of these 2 factors to the sustained responses, both of which may militate in favor of MMR.
The outcome for the 34 patients who were not in MMR at the beginning of the study was less satisfactory (probability of losing their CCyR, 67.5%, P = .0007). Within this second cohort, the impact of adherence on their outcome was dramatic. The 23 patients who had an adherence rate more than 85% had a prognosis similar to that of the MMR patients (probability of losing their CCyR, 4.3%), whereas the 11 patients with a low adherence rate had 54.5% cumulative incidence of loss of CCyR (P < .0001; Figure 1). Thus, good adherence to therapy seemed to be able to overcome any possible biologic difference as patients who had failed to achieve MMR but had a good adherence to therapy had a prognosis similar to that of MMR patients. This must mean that, for patients who have achieved CCyR, good adherence to therapy and not the further achievement of MMR should be the main clinical focus.
In conclusion, we have studied the reasons for cytogenetic relapse and imatinib failure in a cohort of patients on long-term imatinib therapy. We have included in our analysis the more important prognostic factors identified to date. Our data show that poor adherence to imatinib therapy is the most important factor contributing to cytogenetic relapse and imatinib failure. It is therefore of paramount importance that physicians recognize this problem and work toward improving adherence in chronic myeloid leukemia patients treated with tyrosine kinase inhibitors.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 USC section 1734.
Acknowledgments
The authors thank the patients who participated in this study.
This work was supported by the NIHR Biomedical Research Center Funding Scheme.
Authorship
Contribution: A.R.I. and L.E. collected patient data, performed statistical analysis, and wrote the manuscript; G.G., J.S.K., and A.B. performed the molecular studies, assembled the molecular data, and commented on the manuscript; K.K. and C.P. collected patient data and commented on the manuscript; M.B., D. Milojkovic, and J.F.A. provided patient care and commented on the manuscript; R.S. reviewed the statistical analysis and commented on the manuscript; M.M. and F.-X.M. performed the imatinib plasma levels and commented on the manuscript; L.F. supervised the day-to-day running of the Minimal Residual Disease service and commented on the manuscript; A.R. performed the cytogenetics and commented on the manuscript; K.R. reviewed the manuscript; J.G. wrote some of the manuscript; and D. Marin designed the study, performed the statistical analysis, supervised patient care, and wrote the manuscript.
Conflict-of-interest disclosure: D. Marin received research support from Novartis and is a consultant for Novartis and Bristol Myers-Squid. The other authors declare no competing financial interests.
Correspondence: David Marin, Department of Haematology, Imperial College London, Du Cane Road, London W12 0NN, United Kingdom; e-mail: d.marin@imperial.ac.uk.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal