Abstract
Congenital macrothrombocytopenia is a genetically heterogeneous group of rare disorders. αIIbβ3 has not been implicated in these conditions. We identified a novel, conserved heterozygous ITGA2B R995W mutation in 4 unrelated families. The surface expression of platelet αIIbβ3 was decreased to 50% to 70% of control. There was spontaneous PAC-1 and fibrinogen binding to resting platelets without CD62p expression. The activation state of αIIbβ3 in 293T cells was higher for αIIb-W995 than for β3-H723 but was weaker than for β3-N562. FAK was spontaneously phosphorylated in αIIb-W995/β3-transfected 293T cells. These results indicate that αIIb-W995/β3 has a constitutive, activated conformation but does not induce platelet activation. αIIb-W995/β3-transfected CHO cells developed membrane ruffling and abnormal cytoplasmic protrusions. The increased size and decreased number of proplatelet tips in αIIb-W995/β3-transduced mouse fetal liver-derived megakaryocytes indicate defective proplatelet formation. We propose that activating mutations in ITGA2B and ITGB3 represent the etiology of a subset of congenital macrothrombocytopenias.
Introduction
Congenital macrothrombocytopenia is a genetically heterogeneous group of rare disorders.1-4 The most frequent forms include MYH9 disorders and Bernard-Soulier syndrome. In approximately half of cases of congenital macrothrombocytopenia, the pathogenesis remains unknown; thus, a definite diagnosis is unavailable. Glanzmann thrombasthenia is the most common congenital platelet disorder caused by qualitative or quantitative abnormality of the integrin αIIbβ3, in which the platelet counts and morphology are normal.5 However, ITGA2B R995Q mutation has been reported in a patient with Glanzmann thrombasthenia-like phenotype and macrothrombocytopenia.6,7 Recently, heterozygous ITGB3 mutations were found in patients with congenital macrothrombocytopenia.8-10 We report here a novel, conserved heterozygous ITGA2B R995W mutation in 4 unrelated families.
Methods
Patients
Twenty-seven patients with congenital macrothrombocytopenia, in whom MYH9 disorders, heterozygous and homozygous Bernard-Soulier syndrome, type 2B von Willebrand disease, and TUBB1 mutations were excluded, underwent mutational analysis of ITGA2B and ITGB3. Fifty-five consecutive patients were prospectively analyzed for the surface expression of platelet αIIbβ3. Written informed consent was obtained from all patients or their parents in accordance with the Declaration of Helsinki. Institutional review boards of Nagoya Medical Center and each of the participating institutions/hospitals approved this study.
Genetic analysis
The entire coding sequence of exons and exon-intron boundaries of ITGA2B (supplemental Table 1, available on the Blood Web site; see the Supplemental Materials link at the top of the online article) and ITGB3 was amplified by polymerase chain reaction and sequenced. The disease-associated ITGA2B haplotype was determined by cloning and sequencing the polymerase chain reaction products.
Platelet glycoprotein analysis
Cloning, mutagenesis, and retroviral transduction
ITGA2B and ITGB3 sequences were amplified from the patient's platelet cDNA and cloned into pcDNA3.1 (Invitrogen). T562N13 and D723H8 were introduced into ITGB3 cDNA using site-directed mutagenesis. ITGA2B and ITGB3 expression plasmids were cotransfected into 293T and CHO cells. Transfected cells were subjected to flow cytometry, FAK phosphorylation, and spreading assay.13,14
ITGA2B and ITGB3 cDNAs were inserted upstream of internal ribosome entry site (IRES)-enhanced green fluorescent protein (EGFP) and IRES-Kusabira-Orange in the retroviral vector pGCDNsamIRES/EGFP and pGCDNsamIRES/huKO, respectively.15,16 Each plasmid was transfected into 293gp packaging cells with a vesicular stomatitis virus G expression plasmid. Supernatants were used for the transduction of 293gpg producer cells harboring a tetracycline-inducible vesicular stomatitis virus G expression cassette,17 and virus-bearing supernatant was harvested under tetracycline-deficient conditions.
Mouse fetal liver cells were harvested from embryonic day 13.5 embryos and cultured in Dulbecco modified Eagle medium supplemented with 10% fetal calf serum and 50 ng/mL human thrombopoietin. The next day, cells were infected with retroviruses expressing ITGA2B and ITGB3 on recombinant human fibronectin fragment CH-296 (RetroNectin, Takara)-coated plates. After transduction, proplatelet formation was monitored for the next 4 days on EGFP and Kusabira-Orange double-positive megakaryocytes in suspension by inverted fluorescence microscopy. The Experimental Animal Committee of Nagoya Medical Center approved the animal studies.
Results and discussion
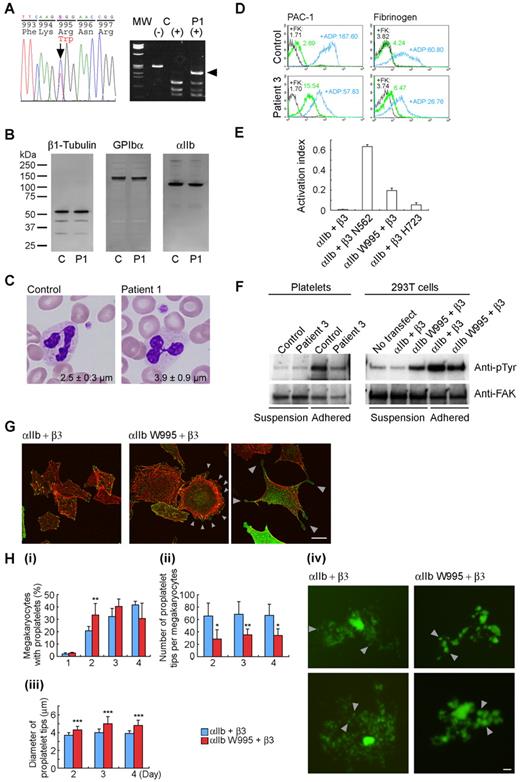
We searched for ITGA2B and ITGB3 mutations in 27 patients with macrothrombocytopenia and identified a novel, conserved heterozygous ITGA2B R995W mutation in one patient (patient 1; Figure 1A). The decreased surface expression of platelet αIIbβ3 prompted us to prospectively screen its expression by flow cytometry. We detected decreased αIIbβ3 expression level (50%-70% of control) in 3 of 55 consecutive patients with macrothrombocytopenia of unknown etiology (patients 2-4 in Table 1). Immunoblotting showed a normal electrophoretic mobility of αIIb, but the total expression level relative to β1-tubulin was decreased to 0.7 (Figure 1B; Table 1). Sequence analysis identified the same heterozygous ITGA2B R995W mutation. In total, we identified 11 patients in 4 unrelated Japanese families. In each family, the disease-associated ITGA2B haplotype was unique, indicating independent occurrence (supplemental Table 2). Patients had larger platelets, approximately 30% increase of control, and moderate thrombocytopenia (Figure 1C; Table 1). These results indicate that macrothrombocytopenia shows a dominant inheritance.
Platelet morphology and biochemical, genetic, and functional analyses of ITGA2B R995W mutation. (A; left) DNA sequence analysis of ITGA2B. The entire coding regions of the patients' ITGA2B were amplified from genomic DNA by the polymerase chain reaction, and amplified DNA fragments were subjected to direct cycle sequence analysis. A C to T transition at nucleotide 3077, changing Arg995 to Trp (R995W), was detected. Nucleotide numbering for ITGA2B cDNA is according to Poncz et al.18 The arrow shows the position of the substitution. (Right) Allele-specific restriction analysis. DNA fragments amplified using primers 2Bg305/303 (supplemental Table 1) were digested with BspACI (SibEnzyme), electrophoresed on 2% agarose gels, and stained with ethidium bromide. The 3077C > T substitution abolishes a recognition site for BspACI, generating a new 231-bp band (arrowhead). The mutation was not found in 108 healthy controls or in the SNP database (www.ncbi.nlm.nih.gov/SNP). MW indicates HaeIII digest of ΦX 174 DNA; C, control; and P1, patient 1. (B) Immunoblot analysis of platelets. Triton X-100-soluble platelet lysates were separated by sodium dodecyl sulfate-polyacrylamide gel electrophoresis on 4% to 12% gradient acrylamide slab gels (Invitrogen) and electroblotted onto polyvinylidine difluoride membranes. The blots were incubated with anti-β1 tubulin antibody NB2301,19 anti-GPIbα antibody PL524 (Takara), and anti-αIIb antibody SZ22 (Beckman-Coulter) and reacted with horseradish peroxidase-conjugated secondary antibody. The bound antibodies were visualized using an enhanced chemiluminescent substrate. C indicates control; and P1, patient 1. (C) Platelet morphology. Peripheral blood smears were stained with May-Grünwald-Giemsa for a normal control and patient 1 (original magnification, × 1000). The patient showed giant platelets with morphologically normal leukocytes. The number in each panel shows the mean platelet size (n = 200). Images were obtained using a BX50 microscope with a 100×/1.35 numeric aperture oil objective (Olympus). Images of the slides were acquired using a DP70 digital camera and DP manager software Version 1.2.1.107 (Olympus). (D) Activation state of platelet αIIbβ3. Washed platelets from patient 3 were resuspended in Tyrode buffer (137mM NaCl, 2.7mM KCl, 1.0mM MgCl2, 3.3mM NaH2PO4, 3.8mM N-2-hydroxyethylpiperazine-N′-2-ethanesulfonic acid, 0.1% glucose, 0.1% bovine serum albumin, pH 7.4) and incubated with fluorescein isothiocyanate-conjugated PAC-1 or 125 μg/mL fluorescein isothiocyanate-labeled fibrinogen in the presence or absence of 10μM FK633 (αIIbβ3-specific peptidomimetic antagonist: black lines) or 10μM adenosine diphosphate (blue lines), and analyzed by flow cytometry. Numbers indicate the mean fluorescence intensity. Results are representative of 2 independent experiments. (E) Quantitation of the αIIbβ3 activation state. The activation state of αIIbβ3 was quantified as an activation index on transiently transfected 293T cells. The activation index was higher for αIIb-W995 than for β3-H723 but was weaker than for an activating mutant β3-N562. Activation index = (a − b)/(c − b), in which a is the mean fluorescence intensity of PAC-1 binding with buffer, b is the mean fluorescence intensity in the presence of FK633, and c is the mean fluorescence intensity in the presence of PT25–2 (anti-αIIbβ3 antibody, which induces the active conformation of αIIbβ3). Data are mean plus or minus SE (n = 3). (F) FAK phosphorylation. Washed platelets from patient 3 (left) or transiently transfected 293T cells (right) were incubated in suspension or seeded onto 100-μg/mL fibrinogen-coated plastic dishes for 1 hour. Cells were washed with phosphate-buffered saline and lysed with 1% Triton X-100 and 1mM sodium vanadate. FAK was immunoprecipitated from the lysates with anti-FAK antibody FAK(C903; Santa Cruz Biotechnology) and protein G-Sepharose, and phosphotyrosine was detected with the antiphosphotyrosine antibody 4G10 (Millipore). Note that 300-μg and 150-μg lysates from suspension and adhered platelets, respectively, and 200-μg lysates from suspension and adhered transfected 293T cells were used for immunoprecipitation analysis. To monitor the loading of gel lanes, the membrane was stripped and reprobed with the anti-FAK antibody FAK(A17; Santa Cruz Biotechnology). Results are representative of 2 and 3 independent experiments for platelets and transfected cells, respectively. (G) Abnormal cytoplasmic protrusions in αIIb-W995/β3-transfected CHO cells. Stably transfected CHO cells were seeded onto 100 μg/mL fibrinogen-coated glass coverslips and incubated for 2 hours at 37°C. Cells were fixed with 3.7% formaldehyde and permeabilized with 0.2% Triton X-100. Coverslips were then stained with anti-CD41a antibody HIP8 (BD Biosciences) followed by Alexa-488-labeled goat antimouse IgG (Invitrogen) and tetramethylrhodamine isothiocyanate-phalloidin (Sigma-Aldrich). Images were obtained using a confocal microscope with a Plan-Apochromat 63×/1.4 oil DIC objective lens LSM5Pascal (Carl Zeiss). Arrowheads indicate membrane ruffling (middle panel) and abnormal cytoplasmic protrusions with the bulbous tips (right panel) in αIIb-W995/β3-transfected CHO cells. Representative images from 3 independent experiments are shown. (H) Abnormal proplatelet formation in αIIb-W995/β3-transfected megakaryocytes. Mouse fetal liver-derived megakaryocytes infected with EGFP-αIIb and Kusabira-Orange-β3 retrovirus were examined in suspension cultures under an IX71 fluorescence microscope with an LCPlanFI 40×/0.60 objective lens (Olympus). (i) The percentage of megakaryocytes extending proplatelets was evaluated manually under a fluorescence microscope 1 to 4 days after infection. For each specimen, at least 100 megakaryocytes were evaluated. The number of proplatelet tips per megakaryocyte (ii) and the size of the proplatelet tips (iii) were measured on acquired images by the ImageScope software Version 10.2.2 (Aperio Technologies). At least 10 megakaryocytes were analyzed for each sample. An unpaired, 2-tailed t test was used to analyze data. A value of P less than .05 was considered statistically significant. Data are mean plus or minus SD. *P < .05. **P < .01. ***P < .0001. (iv) Representative megakaryocytes from 3 independent experiments are shown. Note that the number of proplatelet tips/bulbous structures (arrowheads) is decreased and the size of the tips increased in αIIb-W995/β3-transfected megakaryocytes than in wild-type αIIb/β3-transfected megakaryocytes. Scale bar represents 10 μm.
Platelet morphology and biochemical, genetic, and functional analyses of ITGA2B R995W mutation. (A; left) DNA sequence analysis of ITGA2B. The entire coding regions of the patients' ITGA2B were amplified from genomic DNA by the polymerase chain reaction, and amplified DNA fragments were subjected to direct cycle sequence analysis. A C to T transition at nucleotide 3077, changing Arg995 to Trp (R995W), was detected. Nucleotide numbering for ITGA2B cDNA is according to Poncz et al.18 The arrow shows the position of the substitution. (Right) Allele-specific restriction analysis. DNA fragments amplified using primers 2Bg305/303 (supplemental Table 1) were digested with BspACI (SibEnzyme), electrophoresed on 2% agarose gels, and stained with ethidium bromide. The 3077C > T substitution abolishes a recognition site for BspACI, generating a new 231-bp band (arrowhead). The mutation was not found in 108 healthy controls or in the SNP database (www.ncbi.nlm.nih.gov/SNP). MW indicates HaeIII digest of ΦX 174 DNA; C, control; and P1, patient 1. (B) Immunoblot analysis of platelets. Triton X-100-soluble platelet lysates were separated by sodium dodecyl sulfate-polyacrylamide gel electrophoresis on 4% to 12% gradient acrylamide slab gels (Invitrogen) and electroblotted onto polyvinylidine difluoride membranes. The blots were incubated with anti-β1 tubulin antibody NB2301,19 anti-GPIbα antibody PL524 (Takara), and anti-αIIb antibody SZ22 (Beckman-Coulter) and reacted with horseradish peroxidase-conjugated secondary antibody. The bound antibodies were visualized using an enhanced chemiluminescent substrate. C indicates control; and P1, patient 1. (C) Platelet morphology. Peripheral blood smears were stained with May-Grünwald-Giemsa for a normal control and patient 1 (original magnification, × 1000). The patient showed giant platelets with morphologically normal leukocytes. The number in each panel shows the mean platelet size (n = 200). Images were obtained using a BX50 microscope with a 100×/1.35 numeric aperture oil objective (Olympus). Images of the slides were acquired using a DP70 digital camera and DP manager software Version 1.2.1.107 (Olympus). (D) Activation state of platelet αIIbβ3. Washed platelets from patient 3 were resuspended in Tyrode buffer (137mM NaCl, 2.7mM KCl, 1.0mM MgCl2, 3.3mM NaH2PO4, 3.8mM N-2-hydroxyethylpiperazine-N′-2-ethanesulfonic acid, 0.1% glucose, 0.1% bovine serum albumin, pH 7.4) and incubated with fluorescein isothiocyanate-conjugated PAC-1 or 125 μg/mL fluorescein isothiocyanate-labeled fibrinogen in the presence or absence of 10μM FK633 (αIIbβ3-specific peptidomimetic antagonist: black lines) or 10μM adenosine diphosphate (blue lines), and analyzed by flow cytometry. Numbers indicate the mean fluorescence intensity. Results are representative of 2 independent experiments. (E) Quantitation of the αIIbβ3 activation state. The activation state of αIIbβ3 was quantified as an activation index on transiently transfected 293T cells. The activation index was higher for αIIb-W995 than for β3-H723 but was weaker than for an activating mutant β3-N562. Activation index = (a − b)/(c − b), in which a is the mean fluorescence intensity of PAC-1 binding with buffer, b is the mean fluorescence intensity in the presence of FK633, and c is the mean fluorescence intensity in the presence of PT25–2 (anti-αIIbβ3 antibody, which induces the active conformation of αIIbβ3). Data are mean plus or minus SE (n = 3). (F) FAK phosphorylation. Washed platelets from patient 3 (left) or transiently transfected 293T cells (right) were incubated in suspension or seeded onto 100-μg/mL fibrinogen-coated plastic dishes for 1 hour. Cells were washed with phosphate-buffered saline and lysed with 1% Triton X-100 and 1mM sodium vanadate. FAK was immunoprecipitated from the lysates with anti-FAK antibody FAK(C903; Santa Cruz Biotechnology) and protein G-Sepharose, and phosphotyrosine was detected with the antiphosphotyrosine antibody 4G10 (Millipore). Note that 300-μg and 150-μg lysates from suspension and adhered platelets, respectively, and 200-μg lysates from suspension and adhered transfected 293T cells were used for immunoprecipitation analysis. To monitor the loading of gel lanes, the membrane was stripped and reprobed with the anti-FAK antibody FAK(A17; Santa Cruz Biotechnology). Results are representative of 2 and 3 independent experiments for platelets and transfected cells, respectively. (G) Abnormal cytoplasmic protrusions in αIIb-W995/β3-transfected CHO cells. Stably transfected CHO cells were seeded onto 100 μg/mL fibrinogen-coated glass coverslips and incubated for 2 hours at 37°C. Cells were fixed with 3.7% formaldehyde and permeabilized with 0.2% Triton X-100. Coverslips were then stained with anti-CD41a antibody HIP8 (BD Biosciences) followed by Alexa-488-labeled goat antimouse IgG (Invitrogen) and tetramethylrhodamine isothiocyanate-phalloidin (Sigma-Aldrich). Images were obtained using a confocal microscope with a Plan-Apochromat 63×/1.4 oil DIC objective lens LSM5Pascal (Carl Zeiss). Arrowheads indicate membrane ruffling (middle panel) and abnormal cytoplasmic protrusions with the bulbous tips (right panel) in αIIb-W995/β3-transfected CHO cells. Representative images from 3 independent experiments are shown. (H) Abnormal proplatelet formation in αIIb-W995/β3-transfected megakaryocytes. Mouse fetal liver-derived megakaryocytes infected with EGFP-αIIb and Kusabira-Orange-β3 retrovirus were examined in suspension cultures under an IX71 fluorescence microscope with an LCPlanFI 40×/0.60 objective lens (Olympus). (i) The percentage of megakaryocytes extending proplatelets was evaluated manually under a fluorescence microscope 1 to 4 days after infection. For each specimen, at least 100 megakaryocytes were evaluated. The number of proplatelet tips per megakaryocyte (ii) and the size of the proplatelet tips (iii) were measured on acquired images by the ImageScope software Version 10.2.2 (Aperio Technologies). At least 10 megakaryocytes were analyzed for each sample. An unpaired, 2-tailed t test was used to analyze data. A value of P less than .05 was considered statistically significant. Data are mean plus or minus SD. *P < .05. **P < .01. ***P < .0001. (iv) Representative megakaryocytes from 3 independent experiments are shown. Note that the number of proplatelet tips/bulbous structures (arrowheads) is decreased and the size of the tips increased in αIIb-W995/β3-transfected megakaryocytes than in wild-type αIIb/β3-transfected megakaryocytes. Scale bar represents 10 μm.
Platelet characteristics of patients with the ITGA2B R995W mutation
| Patient . | Sex . | Age, y . | ITGA2B mutation . | Platelet count, × 109/L* . | Platelet size, μm† . | Surface expression relative to control platelets, %‡ . | αIIb/β1 tubulin ratio to controls§ . | Duke bleeding time, minutes‖ . | Platelet aggregation¶ . | Bleeding tendency . | Initial diagnosis . | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| αIIb . | β3 . | αIIbβ3 . | GPIbα . | GPIX . | ADP, % . | Collagen (2.0 μg/mL), % . | Ristocetin (1.3 mg/mL), % . | ||||||||||
| Family 1 | |||||||||||||||||
| Patient 1 | Male | 55 | R995W | 65 | 3.9 ± 0.9 | 53.8 | 67.0 | — | 143.1 | 143.8 | 0.82 | 4.5 | 11 (3μM) | 28 | 77 | − | Unknown thrombocytopenia |
| Family 2 | |||||||||||||||||
| Father | Male | 46 | R995W | 79 | 3.3 ± 0.9 | 51.3 | 51.4 | 56.5 | 106.7 | 109.8 | — | — | — | — | — | − | — |
| Patient 2 | Male | 4 | R995W | 82 | 3.6 ± 1.0 | 54.0 | 58.6 | 61.8 | 138.3 | 134.7 | 0.75 | 5 | — | — | — | Epistaxis | Congenital thrombocytopenia |
| Sister | Female | 9 | R995W | 85 | 3.4 ± 1.0 | 55.6 | 60.6 | 68.4 | 120.0 | 133.1 | 0.71 | 3.5 | — | — | — | − | — |
| Family 3 | |||||||||||||||||
| Mother | Female | 56 | R995W | 80 | 2.8 ± 0.8 | 58.4 | 63.4 | 65.8 | 116.5 | — | 0.73 | — | − | — | |||
| Patient 3 | Female | 27 | R995W | 74 | 3.5 ± 1.0 | 64.4 | 69.7 | 63.8 | 124.8 | — | — | — | 43 (10μM) | 44 | 72 | − | cITP |
| Sister | Female | 24 | R995W | 100 | 3.6 ± 1.0 | 59.3 | 70.2 | 70.8 | 110.9 | — | 0.63 | — | — | — | — | − | — |
| Family 4 | |||||||||||||||||
| Maternal grandfather | Male | 58 | R995W | 66 | 3.4 ± 0.9 | — | — | — | — | — | 0.63 | — | 20 (3μM) | 9 | — | Hemorrhage in exodontia | — |
| Mother | Female | 30 | R995W | 66 | 2.8 ± 0.8 | 56.3 | 62.5 | 57.5 | 127.2 | 112.1 | 0.63 | 2.5 | — | — | Purpura, hemorrhage in exodontia | cITP | |
| Patient 4 | Female | 4M | R995W | 82 | 3.2 ± 1.0 | 63.3 | 62.9 | 62.3 | 147.7 | 140.5 | 0.63 | — | 23 (3μM) | 11 | — | − | NAITP |
| Brother | Male | 5 | R995W | 122 | 3.1 ± 0.8 | — | — | — | — | — | — | — | — | — | — | − | — |
| Mean ± SD | 81.9 ± 16.8# | 3.3 ± 0.3# | 57.4 ± 4.4** | 62.9 ± 5.8** | 63.3 ± 5.0** | 126.1 ± 14.3** | 129.0 ± 14.5** | 0.7 ± 0.07# | |||||||||
| Patient . | Sex . | Age, y . | ITGA2B mutation . | Platelet count, × 109/L* . | Platelet size, μm† . | Surface expression relative to control platelets, %‡ . | αIIb/β1 tubulin ratio to controls§ . | Duke bleeding time, minutes‖ . | Platelet aggregation¶ . | Bleeding tendency . | Initial diagnosis . | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| αIIb . | β3 . | αIIbβ3 . | GPIbα . | GPIX . | ADP, % . | Collagen (2.0 μg/mL), % . | Ristocetin (1.3 mg/mL), % . | ||||||||||
| Family 1 | |||||||||||||||||
| Patient 1 | Male | 55 | R995W | 65 | 3.9 ± 0.9 | 53.8 | 67.0 | — | 143.1 | 143.8 | 0.82 | 4.5 | 11 (3μM) | 28 | 77 | − | Unknown thrombocytopenia |
| Family 2 | |||||||||||||||||
| Father | Male | 46 | R995W | 79 | 3.3 ± 0.9 | 51.3 | 51.4 | 56.5 | 106.7 | 109.8 | — | — | — | — | — | − | — |
| Patient 2 | Male | 4 | R995W | 82 | 3.6 ± 1.0 | 54.0 | 58.6 | 61.8 | 138.3 | 134.7 | 0.75 | 5 | — | — | — | Epistaxis | Congenital thrombocytopenia |
| Sister | Female | 9 | R995W | 85 | 3.4 ± 1.0 | 55.6 | 60.6 | 68.4 | 120.0 | 133.1 | 0.71 | 3.5 | — | — | — | − | — |
| Family 3 | |||||||||||||||||
| Mother | Female | 56 | R995W | 80 | 2.8 ± 0.8 | 58.4 | 63.4 | 65.8 | 116.5 | — | 0.73 | — | − | — | |||
| Patient 3 | Female | 27 | R995W | 74 | 3.5 ± 1.0 | 64.4 | 69.7 | 63.8 | 124.8 | — | — | — | 43 (10μM) | 44 | 72 | − | cITP |
| Sister | Female | 24 | R995W | 100 | 3.6 ± 1.0 | 59.3 | 70.2 | 70.8 | 110.9 | — | 0.63 | — | — | — | — | − | — |
| Family 4 | |||||||||||||||||
| Maternal grandfather | Male | 58 | R995W | 66 | 3.4 ± 0.9 | — | — | — | — | — | 0.63 | — | 20 (3μM) | 9 | — | Hemorrhage in exodontia | — |
| Mother | Female | 30 | R995W | 66 | 2.8 ± 0.8 | 56.3 | 62.5 | 57.5 | 127.2 | 112.1 | 0.63 | 2.5 | — | — | Purpura, hemorrhage in exodontia | cITP | |
| Patient 4 | Female | 4M | R995W | 82 | 3.2 ± 1.0 | 63.3 | 62.9 | 62.3 | 147.7 | 140.5 | 0.63 | — | 23 (3μM) | 11 | — | − | NAITP |
| Brother | Male | 5 | R995W | 122 | 3.1 ± 0.8 | — | — | — | — | — | — | — | — | — | — | − | — |
| Mean ± SD | 81.9 ± 16.8# | 3.3 ± 0.3# | 57.4 ± 4.4** | 62.9 ± 5.8** | 63.3 ± 5.0** | 126.1 ± 14.3** | 129.0 ± 14.5** | 0.7 ± 0.07# | |||||||||
— indicates not applicable; ADP, adenosine diphosphate; cITP, chronic immune thrombocytopenia; and NAITP, neonatal alloimmune thrombocytopenic purpura.
Controls, 273.5 ± 60.4 ( × 109/L) (n = 1014).
Determined by microscopic observation of 200 platelets on a stained peripheral blood smear. Controls, 2.5 ± 0.3 μm (n = 31).
Platelets were reacted with fluorescein isothiocyanate-labeled monoclonal antibodies against αIIb (5B12; Dako Denmark), β3 (SZ21), αIIbβ3 (P2), GPIbα (SZ2; Beckman-Coulter), or GPIX (ALMA16; BD Biosciences) and analyzed in an Epics XL flow cytometer (Beckman-Coulter). Values are expressed as percentage of mean fluorescence intensities of control platelets.
Platelet αIIb/β1-tubulin ratio was determined by densitometric analysis of immunoblots using ImageQuant software Version 5.0 (Molecular Dynamics).
Normal range, 2 to 5 minutes.
Platelet aggregation was performed in platelet-rich plasma. Results are given as percentage maximum aggregation.
P < .001,
P < .0001 vs controls (2-tailed t test).
Bleeding tendency was absent or mild (eg, patient 1 had undergone total colectomy without platelet transfusion). Platelet aggregation induced by adenosine diphosphate and collagen was reduced, although the bleeding time was within the normal limit (Table 1). Platelet spreading on immobilized fibrinogen was partially impaired: the number of fully spread platelets was decreased (supplemental Figure 1). These findings indicate that patients are asymptomatic or exhibit a marginal bleeding tendency and that the clinical and laboratory phenotype is distinct from Glanzmann thrombasthenia.
There was spontaneous PAC-1 binding to resting patients' platelets as well as to αIIb-W995/β3-transfected 293T cells. Although fibrinogen did not bind to platelets in whole blood, increased fibrinogen binding to the washed platelets was observed (Figure 1D; supplemental Figure 2). The activation state, quantified as an activation index in 293T cells, was higher for αIIb-W995 than for β3-H723 but was weaker than that for a strong activating mutant, β3-N56213 (Figure 1E). CD62p expression was absent on the resting platelets (supplemental Figure 2). Spontaneously phosphorylated FAK, a downstream effector of integrin signaling, was not evident in resting platelets in suspension, probably because of low expression level of abnormal αIIbβ3 receptor. However, FAK phosphorylation occurred in αIIb-W995/β3-transfected 293T cells in suspension, indicating constitutively activated αIIbβ3 (Figure 1F). These results indicate that R995W mutation changes αIIbβ3 to a constitutively, albeit partially, activated conformation, but does not induce platelet activation.
αIIb-R995 forms a salt bridge with β3-D723 in the membrane-proximal region and maintains the inactive conformation of the αIIbβ3.20,21 Disruption of the interaction because of partially activated αIIb/β3-H723 or αIIb/β3-A723 mutants but not fully activated mutants, such as αIIb/β3-N562, was reported to cause microtubule-dependent abnormal proplatelet-like cytoplasmic extensions in megakaryocytes and CHO cells.8,22 We found that αIIb-W995/β3-transfected CHO cells exhibited membrane ruffling and abnormal cytoplasmic protrusions with the bulbous tips on fibrinogen-coated surfaces (Figure 1G), indicating that the salt bridge-disrupting mutations exert the same influence on the integrin activation and cytoskeletal events. Abnormal clustering of αIIbβ3, which was reported in ITGB3 L718P mutation,10 was not observed in these cells or in platelets spread on immobilized fibrinogen (supplemental Figure 1). It is worth noting that macrothrombocytopenia-associated ITGB3 mutations in the ectodomain and the cytoplasmic membrane-proximal region have different properties in terms of outside-in signaling and bleeding tendency.9,10
Finally, to determine the functional consequences of R995W mutation on platelet production, we coexpressed αIIb and β3 in mouse fetal liver cells by retroviral transfer and differentiated them into megakaryocytes (Figure 1H). There was an early increase and decrease in the percentage of proplatelet formation-positive megakaryocytes in αIIb-W995/β3-transfected megakaryocytes. The number of proplatelet tips was decreased, and the size of the tips increased. These results are consistent with thrombocytopenia and the increased platelet size in patients, indicating that the stimulation of mutant αIIbβ3 leads to abnormal proplatelet formation. However, not all ITGA2B- and ITGB3-activating mutations are associated with macrothrombocytopenia. Patients with homozygous ITGB3 C549R or C560R mutation inducing constitutively active αIIbβ3 have a normal platelet count and size,23,24 suggesting different molecular mechanisms for the induction of abnormal proplatelet formation.
αIIbβ3 has not been implicated in an abnormal platelet count or morphology.5 Our data support and extend the recent reports that heterozygous, activating mutations in ITGA2B and ITGB3, in the juxtamembrane region, cause macrothrombocytopenia.6-10 We thus propose that such mutations represent the etiology of a subset of congenital macrothrombocytopenias. It is also probable that homozygosity causes Glanzmann thrombasthenia, as demonstrated in the original report of macrothrombocytopenia-associated ITGA2B R995Q mutation.6,7 The creation of a knock-in mouse model and/or use of an in vivo megakaryocyte infusion model25 should clarify the mechanism underlying the production and processing of giant platelets.
The online version of this article contains a data supplement.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 USC section 1734.
Acknowledgments
The authors thank Dr R. C. Mulligan (Children's Hospital Boston, Harvard Medical School, Boston, MA) for 293gp and 293gpg cells, Dr M. Handa (Department of Transfusion Medicine & Cell Therapy, Keio University School of Medicine, Tokyo, Japan) for PT25-2 antibodies, Dr A. Saito (Department of Clinical Research Promotion, Clinical Research Center, National Hospital Organization Nagoya Medical Center) for statistical analysis, and Yoshimi Ito-Yamamura for her skillful technical assistance.
This work was supported by the Japan Society for the Promotion of Science (Grant-in-Aid for Scientific Research), the Ministry of Health, Labor and Welfare, Academic Frontier Project in Japan, Mitsubishi Pharma Research Foundation, the 24th General Assembly of the Japanese Association of Medical Sciences Promotion Fund, the Mother and Child Health Foundation, and the National Hospital Organization Research Fund.
Authorship
Contribution: S.K. designed and performed research, analyzed data, and wrote the paper; H.K. and Y. Tomiyama performed platelet experiments and interpreted the results; M. Onodera constructed retrovirus vectors; M. Otsu, N.T., K.E., and M. Onodera designed the retroviral transfection experiments; Y.M., Y. Takamatsu, J.S., and K.M. contributed patient samples; and H.S. supervised the research.
Conflict-of-interest disclosure: The authors declare no competing financial interests.
Correspondence: Shinji Kunishima, Department of Advanced Diagnosis, Clinical Research Center, National Hospital Organization Nagoya Medical Center, 4-1-1 Sannomaru, Naka-ku, Nagoya 4600001, Japan; e-mail: kunishis@nnh.hosp.go.jp.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal