Abstract
Hemophilia A and B are caused by deficiencies in coagulation factor VIII (FVIII) and factor IX, respectively, resulting in deficient blood coagulation via the intrinsic pathway. The extrinsic coagulation pathway, mediated by factor VIIa and tissue factor (TF), remains intact but is negatively regulated by tissue factor pathway inhibitor (TFPI), which inhibits both factor VIIa and its product, factor Xa. This inhibition limits clot initiation via the extrinsic pathway, whereas factor deficiency in hemophilia limits clot propagation via the intrinsic pathway. ARC19499 is an aptamer that inhibits TFPI, thereby enabling clot initiation and propagation via the extrinsic pathway. The core aptamer binds tightly and specifically to TFPI. ARC19499 blocks TFPI inhibition of both factor Xa and the TF/factor VIIa complex. ARC19499 corrects thrombin generation in hemophilia A and B plasma and restores clotting in FVIII-neutralized whole blood. In the present study, using a monkey model of hemophilia, FVIII neutralization resulted in prolonged clotting times as measured by thromboelastography and prolonged saphenous-vein bleeding times, which are consistent with FVIII deficiency. ARC19499 restored thromboelastography clotting times to baseline levels and corrected bleeding times. These results demonstrate that ARC19499 inhibition of TFPI may be an effective alternative to current treatments of bleeding associated with hemophilia.
Introduction
Hemophilia A and B are bleeding disorders characterized by deficiencies in coagulation factor VIII (FVIII) and factor IX (FIX), respectively, resulting in abnormally prolonged bleeding. Factor replacement is the most effective treatment for hemophilia, but approximately 10%-15% of hemophilia A patients and 1%-3% of hemophilia B patients form inhibitory antibodies to replacement factors.1 For these patients, bleeding episodes are treated with bypassing agents such as recombinant activated coagulation factor VII (FVIIa) or activated plasma-derived prothrombin complex concentrates. Both replacement and bypassing agents come with limitations, including high cost, short in vivo half-lives, and a requirement for intravenous administration.2 These limitations highlight the need for new therapeutic approaches to treating hemophilia; however, most new molecules in development focus on improving current replacement therapies. In this report we describe a potential new therapy that targets tissue factor pathway inhibitor (TFPI), the critical regulator of the FVIIa/tissue factor (TF) pathway.3
Deficiencies in FVIII or FIX preclude normal clot formation via the intrinsic coagulation pathway, whereas the extrinsic coagulation pathway remains intact. This pathway is responsible for the initiation of clot formation through TF/FVIIa–mediated factor Xa (FXa) generation, but it cannot sustain clot formation because of rapid inhibition of TF/FVIIa and FXa by the serine protease inhibitor TFPI. In vivo, TFPI is largely localized on endothelial cell surfaces.3 TFPI is also found in blood, distributed between plasma (∼ 90%, 2-4nM) and platelets (∼ 10%), rapidly localizing to the surface of activated platelets.4 The inhibition of TFPI could be a key mechanism for improving coagulation in hemophilia patients in the absence of factor replacement, and several studies have shown this to be a feasible mechanism both in vitro5,6 and in vivo.7 Recently published studies describe a nonanticoagulant, sulfated polysaccharide from seaweed with TFPI-dependent and -independent procoagulant activities that is efficacious in models of hemophilia, providing partial validation for this approach.8,9 In the present study, we describe ARC19499, a polyethylene glycol (PEG)–conjugated, modified oligonucleotide aptamer that potently and specifically inhibits TFPI. The data presented here underscore the important role of TFPI in extrinsic pathway regulation, and highlight the potential for specific TFPI inhibition as a treatment for bleeding associated with FVIII or FIX deficiency.
Methods
Reagents
DNA oligonucleotides were from Integrated DNA Technologies. Modified oligonucleotides were synthesized in micromole to millimole quantities on a Mermade-192, Mermade-12 (BioAutomation), or ÄKTA Oligopilot (Amersham Pharmacia Biotech) DNA/RNA synthesizer using standard solid-phase chemistry with phosphoramidites (Hongene Biotech). Pooled normal plasma (PNP), pooled plasma from hemophilia A or B patients (< 1% FVIII or FIX, respectively), and plasma from hemophilia A patients with high titers of FVIII antibody (≥ 160 Bethesda units [BU]/mL) were from George King Bio-Medical. Lyophilized TFPI-depleted plasma, recombinant full-length TFPI, FVIIa, and Spectrozyme Xa were from American Diagnostica. Factor X (FX), FXa, TF (unless noted otherwise), and sheep polyclonal anti–human FVIII antibody were from Haematologic Technologies. BSA was from Sigma (activity assays) or New England Biolabs (binding experiments). Phospholipid vesicles containing phosphatidylcholine and phosphatidylserine (PCPS; from egg yolk and porcine brain, respectively; Avanti Polar Lipids) were made as described previously at molar ratios of 80% and 20%, respectively.10
Blood preparation
For experiments using freshly drawn whole blood, single-donor samples were drawn by standard phlebotomy methods from healthy volunteers. Blood was drawn into 4.5-mL glass Vacutainer tubes containing 3.2% sodium citrate (BD Biosciences). To generate FVIII-neutralized blood, citrated blood was incubated with a polyclonal anti-FVIII antibody (3 hours at 37°C) at a final concentration of 10 BU/mL. A separate control sample was treated with 0.9% saline (3 hours at 37°C).
Aptamer generation
ARC19499 was generated via in vitro selection from a pool of randomized sequences and subsequent optimization, essentially as described previously.11-13 Briefly, a randomized pool of dC, mA, mG, and mU residues was used for the selection, where “d” denotes a 2′-H residue and “m” denotes a 2′-OCH3 residue. Eleven rounds of selection were carried out against recombinant TFPI and resulted in the identification of the parent clone. The core aptamer sequence was identified from truncated clone variants and appended at its 3′-end with an inverted dT residue (idT) to generate ARC17480 (5′-mGmGmAmAmUmAmUmAdCmUmUmGmGdCmUdCmGmUmUmAmGmGmUmGdCmGmUmAmUmAmUmAidT-3′). Addition of a 5′-hexylamine linker and a branched 40-kDa PEG (JenKem Technology) generated ARC19499. The negative control oligonucleotide was a modified, inactive version of ARC17480 (5′-mGmGmAmAmUmAmUmAdCmUmUmGmGdCmUmGdCmUmUmAmGmGmUmGdCmGmUmAmUmAmUmAidT-3′). Further details of ARC19499 generation are in the Supplemental methods (available on the Blood Web site; see the Supplemental Materials link at the top of the online article).
Binding experiments
Recombinant TFPI was used for binding experiments. Sourcing information for all other proteins used in binding experiments is in the supplemental Methods. Binding experiments with ARC17480 were carried out by incubating trace amounts of 5′-32P–labeled aptamer (< 167pM) with different concentrations of protein at 37°C for 30 minutes in Dulbecco phosphate-buffered saline with Ca2+ and Mg2+ (Mediatech) with 0.1 mg/mL of BSA in a 30-μL reaction volume. Some reactions also contained 0.1 mg/mL of tRNA (Ambion). After incubation, reactions were vacuum-filtered over a nitrocellulose and nylon filter stack to capture aptamer-protein complexes and unbound aptamer, respectively.14 The amount of radiolabeled aptamer on each filter was quantified, and the percentage of protein-bound aptamer was plotted as a function of protein concentration. For ARC17480 binding to TFPI, data were fit to the equation: % aptamer bound = max/(1 + KD/[TFPI]), where max is the maximum percentage bound and KD is the aptamer-protein dissociation constant. The average of the fits for 14 experiments was used to generate the KD. Binding experiments with all other proteins were repeated at least 3 times. Competition-binding experiments were carried out similarly except the TFPI concentration was held constant at 10nM and different concentrations of unlabeled ARC17480, ARC19499, or control oligonucleotide were used as competitors. The percentage of protein-bound aptamer was plotted as a function of competitor concentration. The data were fitted to the equation: % aptamer bound = max/(1 + [competitor]/IC50), where max is the maximum percentage bound and IC50 is the competitor half-maximal inhibitory concentration; the average of fits from 4 experiments was used to generate an IC50.
FXa activity assay
FXa activity was measured as described previously with minor variations.15 FXa and TFPI were incubated for 30 minutes, followed by the addition of aptamer and Spectrozyme Xa substrate, all at 37°C. Final concentrations were 2nM FXa, 4nM TFPI, 0.5-500nM aptamer, and 500μM Spectrozyme Xa in buffer containing 20mM HEPES, pH 7.6, 150mM NaCl, 5mM CaCl2, and 0.5 mg/mL of BSA. Some reactions were performed in the absence of TFPI and aptamer. The increase in absorbance over time was measured at 405 nm in a SpectraMax Plus plate reader (Molecular Devices). For each reaction, the rate of substrate cleavage was determined and plotted as a function of aptamer concentration.
TF/FVIIa activity assay
TF, FVIIa, and PCPS vesicles were incubated at 37°C for 5 minutes, followed by the addition of TFPI with or without aptamer and then FX. Final concentrations were 5pM TF, 170nM FX, 1nM FVIIa, 1nM TFPI, 50μM PCPS vesicles, and 0.01-1000nM ARC19499 or 1000nM control oligonucleotide in reaction buffer (20mM HEPES, pH 7.4, 150mM NaCl, 1 mg/mL of BSA, and 0.02% NaN3) with 5mM CaCl2. Aliquots were removed at various time points over 5 minutes, and reactions were quenched by dilution in cold reaction buffer with 50mM EDTA. FXa activity was evaluated by adding a chromogenic FXa substrate, S-2765 (0.2mM; Diapharma/Chromogenix), and measuring the increase in absorbance over time at 405 nm. Absorbances were compared with a FXa standard curve to determine the amount of FXa generated. An effective concentration value (EC50) was determined from terminal rates (2-5 minutes) normalized by subtracting the rate of FXa generation without ARC19499 and dividing by the rate without both ARC19499 and TFPI. Data were fitted to the equation: νARC19499 = νmax/(1 + EC50/[ARC19499]), where νARC19499 is the normalized FXa activity measured at each concentration of ARC19499 and νmax is the maximum FXa activity at saturating ARC19499.
CAT analysis
Thrombin generation was measured using the Calibrated Automated Thrombogram® (CAT) system16 containing the Fluoroskan Ascent (Thermo Electron) fluorescence plate reader configured by Thrombinoscope BV (Diagnostica Stago). ARC19499 was diluted in plasma, and 80 μL was mixed with 20 μL of PPP-reagent LOW containing TF and phospholipids. The final TF concentration was 1pM unless noted otherwise. If necessary, PPP-reagent LOW was diluted using MP Reagent. Duplicate samples were incubated at 37°C in Immulon 2 HB-High Binding 96-well U-bottom plates (VWR). In control wells, 80 μL of plasma was mixed with 20 μL of thrombin calibrator. The reaction was started by the addition of 20 μL of prewarmed Flu-Ca reagent containing CaCl2 and a fluorogenic thrombin substrate. Results were compared with baseline responses for PNP without aptamer. All CAT-specific reagents were from Diagnostica Stago. Analysis was performed using Thrombinoscope Analysis Version 3.0.
TEG analysis
Thromboelastography (TEG) was measured using a TEG 5000 analyzer (Haemonetics). Blood (320 μL), with or without FVIII antibody and ARC19499, or plasma (320 μL) was mixed with 20 or 30 μL, respectively, of 0.2M CaCl2 and 10 μL of TF (Innovin, Dade-Behring; final dilution of 1:200 000) at 37°C. If no clotting was observed by 45 minutes, the assay was stopped, the R value (time to initial clot formation) was recorded as 45.0 minutes, and no angle or maximum amplitude (MA) values were determined. Plasma samples from the nonhuman primate model of hemophilia A were analyzed in the TEG assay with 50μM PCPS vesicles.
Nonhuman primate model
Monkeys anesthetized with isoflurane were injected via catheter with a sheep polyclonal anti–human FVIII antibody at approximately 50 000 BU per monkey. Test substances (saline or ARC19499) were administered intravenously as a single bolus via the saphenous vein catheter 3.5 hours after antibody administration. Blood samples were drawn before and 2.5 hours after antibody administration and 0.25, 1, and 2 hours after test-substance treatment. Within 10 minutes of collection, samples were centrifuged at 2000g for 15 minutes at room temperature. The plasma was removed and stored at −80°C. Samples were thawed rapidly at 37°C for analysis. The ARC19499 concentration in some of the monkey samples was determined via high-performance liquid chromatography with ultraviolet absorbance detection. Further details about the model and a description of concentration determination are available in the supplemental Methods. All animal experiments were handled in compliance with the Guide for the Care and Use of Laboratory Animals according to protocols approved by the Institutional Animal Care and Use Committee of DaVinci Biomedical Research.
FVIII activity levels
FVIII activity levels in plasma from monkeys treated with anti-FVIII antibody were measured using the Coamatic FVIII assay (Chromogenix/Diapharma) as per the manufacturer's instructions. A standard curve was generated using plasma from untreated monkeys.
Bleeding time assessment
The saphenous vein was exposed and a 22-gauge needle was bent at the bevel 5 mm from the needle tip to 90° using a hemostat. The needle was inserted into the exposed vein up to the needle bend, puncturing only one venous wall. Blood was wicked away using Surgicutt Bleeding Time Blotting Paper (International Technidyne) without touching the actual puncture site. Time was measured from the moment bleeding began until bleeding cessation, as determined by the inability to wick away blood. Blood pressure readings were taken 1-5 minutes before and after bleeding time assessment. After bleeding time assessment, the wound was closed with Gluture (skin glue). Further details are provided in the supplemental Methods.
Results
Generation of ARC17480 and ARC19499
The TFPI-binding core oligonucleotide of ARC19499 was generated using systematic evolution of ligands by exponential enrichment12 with a modified nucleotide pool using recombinant TFPI derived from the human gene. Iterative rounds of selection for binding to TFPI followed by the identification of individual clones resulted in the generation of the 84-nucleotide precursor to ARC19499. This molecule was subsequently minimized to the 32-nucleotide core aptamer and appended with a 3′-idT to generate ARC17480. ARC19499 has the ARC17480 sequence appended at its 5′-end with a 40-kDa PEG moiety via an amine linker.
Binding specificity for TFPI
ARC19499 is not amenable to in vitro experiments requiring radiolabeling because of its 5′-40 kDa PEG moiety; therefore, the core aptamer ARC17480 was used in binding experiments. ARC17480 bound tightly to TFPI with a KD of 2.8 ± 0.3nM (Figure 1A-C). Competition-binding experiments demonstrated that ARC17480 and ARC19499 had a similar affinity for TFPI. Unlabeled ARC17480 and ARC19499 competed with radiolabeled ARC17480 for binding to TFPI with an IC50 of 15.0 ± 0.3nM and 17.9 ± 1.4nM, respectively (Figure 1D). The control oligonucleotide showed only a small amount of competition at high concentrations. Further binding studies measuring the affinity of ARC17480 for selected Kunitz-domain proteins, protease inhibitors, and coagulation factors indicated that the aptamer was highly specific for human TFPI. The aptamer demonstrated no specific binding to tested activated coagulation proteins (factor Va, α-thrombin, FVIIa, FIXa, FXa, factor XIa, kallikrein, or plasmin; Figure 1A), protease inhibitors (antithrombin, heparin cofactor II, serpin A1, or TFPI-2; Figure 1B), or coagulation zymogens (factor XII or prothrombin; Figure 1C). Minor aptamer binding was observed at high concentrations of factor XII, but was eliminated in the presence of tRNA, indicating nonspecific binding (Figure 1C). These experiments demonstrated that ARC17480, and by extension ARC19499, interacts specifically with TFPI.
ARC17480 and ARC19499 binding to TFPI and other proteins. (A-C) Representative curves showing binding between radiolabeled ARC17480 and TFPI, as well as activated coagulation proteins (A), protease inhibitors (B), and coagulation zymogens (C). The percentage of protein-bound aptamer is plotted as a function of protein concentration. (D) Competition-binding experiments using 10nM TFPI and radiolabeled ARC17480, with unlabeled ARC17480, ARC19499, or control oligonucleotide as competitors. The percentage of protein-bound radiolabeled aptamer is plotted as a function of the unlabeled competitor concentration. Representative curves are shown.
ARC17480 and ARC19499 binding to TFPI and other proteins. (A-C) Representative curves showing binding between radiolabeled ARC17480 and TFPI, as well as activated coagulation proteins (A), protease inhibitors (B), and coagulation zymogens (C). The percentage of protein-bound aptamer is plotted as a function of protein concentration. (D) Competition-binding experiments using 10nM TFPI and radiolabeled ARC17480, with unlabeled ARC17480, ARC19499, or control oligonucleotide as competitors. The percentage of protein-bound radiolabeled aptamer is plotted as a function of the unlabeled competitor concentration. Representative curves are shown.
Inhibition of TFPI function by ARC19499
TFPI is a slow-acting but potent inhibitor of FXa.15 Inhibition requires the Kunitz-2 domain of TFPI,17,18 and other regions contribute to the strength of the interaction.15 To investigate the ability of ARC19499 to modulate TFPI inhibition of FXa, the activity of FXa was measured in the presence and absence of TFPI, with or without aptamer. TFPI and FXa were preincubated to allow complex formation, followed by the addition of a chromogenic substrate with various aptamer concentrations. The rate of substrate cleavage under each condition was determined and plotted as a function of aptamer concentration (Figure 2A). ARC19499 decreased TFPI inhibition of FXa activity by up to 70%, as measured by a concentration-dependent increase in FXa activity. The negative control oligonucleotide had no effect on FXa activity, and ARC19499 did not affect FXa activity in the absence of TFPI (data not shown). These results demonstrate that ARC19499 disrupts the interaction between TFPI and FXa.
Activity of ARC19499 in TFPI-dependent assays using purified proteins. (A) Effect of ARC19499 on TFPI inhibition of FXa activity. The rate of FXa (2nM) cleavage of a chromogenic substrate is shown in the absence (solid line) and presence (dashed line) of 4nM TFPI. ARC19499 (□) and the negative control oligonucleotide (○) were tested in the presence of TFPI. The rate of substrate cleavage is plotted as a function of aptamer concentration. (B) Effect of ARC19499 on TFPI inhibition of TF/FVIIa activity. The inhibitory activity of increasing concentrations of ARC19499 was tested in the presence of 1nM TFPI. Terminal rates were determined from data obtained between 2 and 5 minutes and normalized against the rate of FXa generation in the absence of TFPI or aptamer. Inset shows representative plots of FXa generation as a function of time used to generate the normalized data. The rate of FXa generation was measured in the absence of TFPI (■), in the presence of 1nM TFPI (●), and with 0.01-1000nM ARC19499 in the presence of 1nM TFPI. Results are represented as means ± SEM (error bars or shaded area); n = 4 (A) or n = 3 (B).
Activity of ARC19499 in TFPI-dependent assays using purified proteins. (A) Effect of ARC19499 on TFPI inhibition of FXa activity. The rate of FXa (2nM) cleavage of a chromogenic substrate is shown in the absence (solid line) and presence (dashed line) of 4nM TFPI. ARC19499 (□) and the negative control oligonucleotide (○) were tested in the presence of TFPI. The rate of substrate cleavage is plotted as a function of aptamer concentration. (B) Effect of ARC19499 on TFPI inhibition of TF/FVIIa activity. The inhibitory activity of increasing concentrations of ARC19499 was tested in the presence of 1nM TFPI. Terminal rates were determined from data obtained between 2 and 5 minutes and normalized against the rate of FXa generation in the absence of TFPI or aptamer. Inset shows representative plots of FXa generation as a function of time used to generate the normalized data. The rate of FXa generation was measured in the absence of TFPI (■), in the presence of 1nM TFPI (●), and with 0.01-1000nM ARC19499 in the presence of 1nM TFPI. Results are represented as means ± SEM (error bars or shaded area); n = 4 (A) or n = 3 (B).
In the presence of FXa, TFPI is a rapid and potent inhibitor of TF/FVIIa, blocking further activation of FX. To investigate ARC19499 interference of this inhibition, the aptamer was evaluated in an assay measuring FXa generation in the presence of TF/FVIIa and TFPI. TF, FVIIa, and phospholipid vesicles were mixed in the presence and absence of TFPI and ARC19499. FX addition initiated the reaction, and aliquots were removed at various time points. FX activation was monitored using a chromogenic substrate cleaved by FXa. In the absence of TFPI or ARC19499, FXa generation occurred at a linear rate that decreased significantly after TFPI addition. As reported previously,19,20 FXa generation in the presence of TFPI was nonlinear (Figure 2B inset), reflecting the initial, slow buildup of the inhibitory TFPI/FXa complex. Rates were calculated from the terminal portion of the curve (2-5 minutes), where substantial TFPI/FXa is present. Increasing concentrations of ARC19499 increased the rate of FXa generation, reaching a rate nearly equivalent to that in the absence of TFPI (Figure 2B inset). Normalized rates demonstrated that ARC19499 restored nearly complete FXa generation (Figure 2B), with an EC50 of 1.8nM. The control oligonucleotide had no effect on FXa generation (data not shown). These results demonstrate that ARC19499 functionally blocks the ability of TFPI to inhibit FX activation by TF/FVIIa.
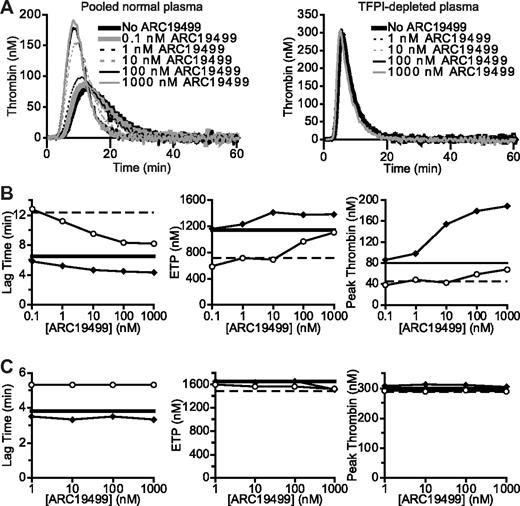
Specificity of ARC19499 for TFPI in plasma
To address the specificity of ARC19499 for TFPI, the effect of the aptamer on thrombin generation was compared in fresh-frozen PNP and reconstituted, lyophilized, TFPI-depleted plasma using the CAT assay (Figure 3). Thrombin-generation assays such as CAT assess the global hemostatic state of plasma. In this assay, thrombin generation in plasma is initiated by the addition of TF, phospholipid vesicles, and CaCl2, and is measured by monitoring the cleavage of a fluorescent substrate.21 The effects of ARC19499 were tested in the CAT assay using 0.1 and 1.0pM TF concentrations. Increasing concentrations of ARC19499 affected the thrombin generation curves in PNP but not in TFPI-depleted plasma (Figure 3A). The change in thrombin generation as a result of ARC19499 addition to PNP was manifested as a decrease in lag time (time required for initial thrombin generation) and an increase in both endogenous thrombin potential (ETP; determined by the area under the thrombin generation curve) and peak thrombin (the highest amount of thrombin generated at any one point in the assay) at both TF concentrations (Figure 3B). In TFPI-depleted plasma, a decrease in lag time and an increase in both ETP and peak thrombin were observed relative to PNP in the absence of ARC19499, which is consistent with a lack of TFPI activity. Increasing concentrations of ARC19499 caused no further change in any of these parameters at either 0.1 or 1.0pM TF (Figure 3C), indicating that ARC19499 has no TFPI-independent effects on thrombin generation in plasma. Similar results were found in PNP treated with an anti-TFPI antibody to neutralize TFPI activity (supplemental Figure). These results demonstrate that the procoagulant activity of ARC19499 in plasma relies on the presence of functioning TFPI.
ARC19499 inhibition of TFPI in human plasma. (A) Representative thrombin generation curves with 1pM TF. Left, ARC19499 dose response in PNP. Right, ARC19499 dose response in TFPI-depleted plasma. (B-C) Effect of ARC19499 on thrombin generation with 1.0pM (♦) or 0.1pM (○) TF. The solid and dashed lines correspond to plasma in the absence of ARC19499 with 1.0 or 0.1pM TF, respectively. Left panel shows lag time; middle panel, ETP; right panel, peak thrombin. Thrombin generation activity was tested in PNP (B) and in TFPI-depleted plasma (C).
ARC19499 inhibition of TFPI in human plasma. (A) Representative thrombin generation curves with 1pM TF. Left, ARC19499 dose response in PNP. Right, ARC19499 dose response in TFPI-depleted plasma. (B-C) Effect of ARC19499 on thrombin generation with 1.0pM (♦) or 0.1pM (○) TF. The solid and dashed lines correspond to plasma in the absence of ARC19499 with 1.0 or 0.1pM TF, respectively. Left panel shows lag time; middle panel, ETP; right panel, peak thrombin. Thrombin generation activity was tested in PNP (B) and in TFPI-depleted plasma (C).
ARC19499 enhances thrombin generation in hemophilia plasma
Thrombin-generation assays such as the CAT assay are used in hemophilia care centers22,23 because deficiency in FVIII or FIX activity is correlated with reduced thrombin generation.22,24 The ability of ARC19499 to enhance thrombin generation was tested in 3 platelet-poor hemophilia plasmas: plasma pooled from 7-8 patients with severe hemophilia A (< 1% FVIII; “hemophilia A plasma”), plasma from 3 different hemophilia A patients with high titers of anti-FVIII antibodies (≥ 160 BU/mL; “inhibitor plasma”), and plasma pooled from 2 patients with severe hemophilia B (< 1% FIX; “hemophilia B plasma”; Figure 4). Hemophilia A plasma had a slightly shorter lag time and a markedly decreased ETP and peak thrombin (∼ 50% and ∼ 75%, respectively) compared with normal plasma. This is consistent with previous observations that FVIII-deficient plasma has a greater impact on the prolongation in clotting, manifested by larger changes in ETP and peak thrombin, than on clot initiation, manifested in an almost unchanged lag time.25 Increasing concentrations of ARC19499 largely corrected the defect in thrombin generation. ETP was corrected to near-normal levels with 3nM ARC19499, and peak thrombin was corrected with 100nM aptamer (Figure 4A). Inhibitor plasma also exhibited decreased ETP and peak thrombin (∼ 50% and ∼ 70%, respectively) compared with normal plasma. As with the severe hemophilia A plasma, ARC19499 increased thrombin generation in this plasma. With 30nM ARC19499, both the ETP and peak thrombin were at normal levels (Figure 4B). Hemophilia B had an even greater defect in thrombin generation, with significantly decreased ETP and peak thrombin (∼ 70% and ∼ 90%, respectively) and an increased lag time. As with the other hemophilia plasmas, increasing concentrations of ARC19499 improved thrombin generation, achieving normal ETP levels with 30nM ARC19499 and normal peak thrombin levels with 100-300nM aptamer (Figure 4C). These results demonstrate that 30-100nM ARC19499 is effective in restoring coagulation in 3 different types of hemophilia plasma. The negative control oligonucleotide was also tested in the 3 different plasmas and demonstrated no correction of thrombin generation (Figure 4).
ARC19499 effect on thrombin generation in human plasma. (A-C) Left panels show lag time; middle panels, ETP; right panels, peak thrombin. Thrombin generation was initiated with 1pM TF. In all graphs, the effect of ARC19499 (♦) was compared with the negative control oligonucleotide (■). Lines represent the activity of normal plasma (solid lines) and factor-deficient plasma (dashed lines) in the absence of aptamer. (A) Activity in hemophilia A plasma. (B) Activity in inhibitor plasma. (C) Activity in hemophilia B plasma. Results are represented as the means ± SEM. Shaded areas around the solid and dashed lines represent the SEM for the normal and factor-deficient plasma, respectively, in the absence of aptamer; n = 3 for each plasma.
ARC19499 effect on thrombin generation in human plasma. (A-C) Left panels show lag time; middle panels, ETP; right panels, peak thrombin. Thrombin generation was initiated with 1pM TF. In all graphs, the effect of ARC19499 (♦) was compared with the negative control oligonucleotide (■). Lines represent the activity of normal plasma (solid lines) and factor-deficient plasma (dashed lines) in the absence of aptamer. (A) Activity in hemophilia A plasma. (B) Activity in inhibitor plasma. (C) Activity in hemophilia B plasma. Results are represented as the means ± SEM. Shaded areas around the solid and dashed lines represent the SEM for the normal and factor-deficient plasma, respectively, in the absence of aptamer; n = 3 for each plasma.
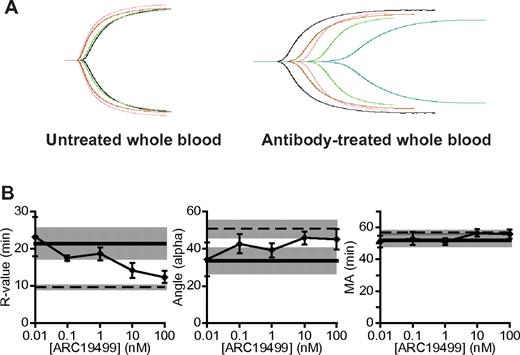
ARC19499 enhances clot formation in FVIII-depleted whole blood
TEG is another global assay of hemostasis that measures the kinetics of clot formation.26 Like the CAT assay, it is used to measure the hemostatic response of hemophilic whole blood or plasma,27,28 and is currently under intense study as a monitoring method to guide the dosing of bypass agents such as activated prothrombin complex concentrates and recombinant FVIIa.27,29 To assess the effect of ARC19499 on clot formation in whole blood, FVIII-depleted whole blood was prepared using an inhibitory, anti-FVIII polyclonal antibody. Increasing ARC19499 concentrations were tested in both untreated and antibody-treated whole blood using the TEG assay, with clotting initiated by the addition of TF and CaCl2 (Figure 5). ARC19499 had a strong, positive impact on clot formation in the antibody-treated blood and little to no impact in the untreated whole blood (Figure 5A).
ARC19499 effect on clot formation in FVIII antibody–treated whole blood. (A) Representative TEG tracings in untreated (left) and antibody-treated (right) whole blood. Black lines show untreated whole blood without aptamer; green, 1nM ARC19499; pink, 10nM ARC19499; red, 100nM ARC19499; and blue, antibody-treated whole blood without aptamer. (B) Effect of ARC19499 on TEG parameters of FVIII antibody–treated whole blood. Left panel shows the R value; middle, angle; right, MA. Lines represent the activity of untreated (dashed lines) and antibody-treated (solid lines) whole blood in the absence of aptamer, with the shaded areas representing SEM. Results are represented as the means ± SEM; n = 3.
ARC19499 effect on clot formation in FVIII antibody–treated whole blood. (A) Representative TEG tracings in untreated (left) and antibody-treated (right) whole blood. Black lines show untreated whole blood without aptamer; green, 1nM ARC19499; pink, 10nM ARC19499; red, 100nM ARC19499; and blue, antibody-treated whole blood without aptamer. (B) Effect of ARC19499 on TEG parameters of FVIII antibody–treated whole blood. Left panel shows the R value; middle, angle; right, MA. Lines represent the activity of untreated (dashed lines) and antibody-treated (solid lines) whole blood in the absence of aptamer, with the shaded areas representing SEM. Results are represented as the means ± SEM; n = 3.
Hemophilia blood is characterized by profound changes in TEG assay parameters relative to normal blood, including prolongation of the R value and reduction in the angle (a measure of the rate of clot growth).9,30 Treatment of normal whole blood with the anti-FVIII antibody induced a hemophilia A–like state, characterized by a significantly prolonged R value and a decreased angle (Figure 5B). The addition of ARC19499 to the antibody-treated blood resulted in a dose-dependent decrease in the R value, reaching levels observed with untreated blood with 100nM aptamer (Figure 5B). ARC19499 also increased the angle, reaching levels observed with untreated blood with 10nM aptamer (Figure 5B). The MA, a measure of the strength of the clot, did not change significantly on FVIII depletion or with subsequent ARC19499 addition (Figure 5B). The control oligonucleotide had no impact on clot formation (data not shown). These results demonstrate that ARC19499 acts as a procoagulant in hemophilia A–like blood.
ARC19499 restores TEG parameters in a nonhuman primate model of acquired hemophilia A
Hemophilic dogs and mice have been essential in the discovery and development of hemophilia treatments.9,31-34 ARC19499, however, is highly specific for human and nonhuman primate TFPI, showing no evidence of anti-TFPI activity in plasma from mouse, rat, rabbit, dog, or pig (Q. Wang, X. Tian, unpublished observations, May 2009), precluding the use of established models to assess aptamer activity. Therefore, we generated a model of acquired hemophilia A in cynomolgus monkeys to assess aptamer activity in vivo. The model is adapted from an acquired hemophilia A model in rabbits7 and an acquired hemophilia B model in cynomolgus monkeys.35 In our model, healthy, normal cynomolgus monkeys were injected with an anti-human FVIII polyclonal antibody that neutralized FVIII activity, creating a temporary hemophilia A–like state. Before antibody administration, the plasma from all monkeys had normal FVIII activity levels, varying from 65.8%-81.5% compared with a standard plasma sample pooled from untreated animals. After antibody administration, this activity decreased to below measurable levels (< 0.6%) and remained at this low level for the course of the study (data not shown).
The ability of ARC19499 to restore clot formation was first assessed in the TEG assay by adding aptamer to plasma from monkeys previously treated with a bolus of anti-FVIII antibody (Figure 6A). Plasma from these monkeys had prolonged R values after antibody administration compared with baseline levels from plasma acquired before antibody administration. ARC19499 addition improved the R value to near-baseline values. Monkeys that received anti-FVIII antibody were then treated with 100, 300, or 600 μg/kg of ARC19499 via intravenous injection. A control group of monkeys was treated with 1 mL/kg of saline instead of aptamer. Blood samples were drawn at baseline, after antibody administration, and 0.25, 1, and 2 hours after aptamer or saline treatment (Figure 6B). Plasma was isolated from the blood samples and analyzed with the TF-initiated TEG assay to determine the effect of ARC19499 on clot formation. Tracings from the TEG analysis showed that antibody administration diminished clot formation, and subsequent treatment with higher concentrations of ARC19499 restored clot formation (Figure 6C). Plasma samples from monkeys in all groups had prolonged R values and reduced angles after antibody administration, which is consistent with diminished coagulation (Figure 6D). After treatment with either 300 or 600 μg/kg of ARC19499, the R value was reduced to near-baseline levels, which is indicative of an improvement in coagulation. The 600 μg/kg dose also modestly improved the angle. The 100 μg/kg dose of ARC19499 had no effect on either R value or angle, similar to the saline negative control (Figure 6D). These results indicate that ARC19499 is procoagulant in ex vivo measures of coagulation in a nonhuman primate model of hemophilia A.
ARC19499 effect on clot formation in FVIII antibody–treated cynomolgus monkeys. (A) In vitro dose response of ARC19499 added to plasma from cynomolgus monkeys previously treated with a bolus of anti-FVIII antibody to eliminate FVIII activity. Lines represent activity of cynomolgus monkey plasma before (solid lines) and after (dashed lines) antibody treatment in the absence of aptamer, with shaded areas representing SEM. (B) Schematic of in vivo dosing and blood drawing schedule for the study. There were 4 distinct groups of monkeys treated with saline or with 100, 300, or 600 μg/kg of ARC19499. (C) Representative TEG tracings from plasma of cynomolgus monkeys treated with FVIII antibody followed by saline (left), 100 μg/kg of ARC19499 (middle), or 600 μg/kg of ARC19499 (right). Black line shows the baseline time point; green, 2.5 hours after antibody administration; pink, 0.25 hours after aptamer or saline treatment; red, 1 hour after treatment; and blue, 2 hours after treatment. (D) Effect of ARC19499 treatment on TEG parameters. Left panel shows the R value; right, angle. Monkeys were treated with anti-FVIII antibody, followed by saline (▵) or 100 (●), 300 (♦), or 600 (■) μg/kg of ARC19499. Results are represented as the means ± SEM; n = 3 for saline and the 100 μg/kg ARC19499 dose; n = 6 for the 300 μg/kg dose; and n = 2 for the 600 μg/kg dose.
ARC19499 effect on clot formation in FVIII antibody–treated cynomolgus monkeys. (A) In vitro dose response of ARC19499 added to plasma from cynomolgus monkeys previously treated with a bolus of anti-FVIII antibody to eliminate FVIII activity. Lines represent activity of cynomolgus monkey plasma before (solid lines) and after (dashed lines) antibody treatment in the absence of aptamer, with shaded areas representing SEM. (B) Schematic of in vivo dosing and blood drawing schedule for the study. There were 4 distinct groups of monkeys treated with saline or with 100, 300, or 600 μg/kg of ARC19499. (C) Representative TEG tracings from plasma of cynomolgus monkeys treated with FVIII antibody followed by saline (left), 100 μg/kg of ARC19499 (middle), or 600 μg/kg of ARC19499 (right). Black line shows the baseline time point; green, 2.5 hours after antibody administration; pink, 0.25 hours after aptamer or saline treatment; red, 1 hour after treatment; and blue, 2 hours after treatment. (D) Effect of ARC19499 treatment on TEG parameters. Left panel shows the R value; right, angle. Monkeys were treated with anti-FVIII antibody, followed by saline (▵) or 100 (●), 300 (♦), or 600 (■) μg/kg of ARC19499. Results are represented as the means ± SEM; n = 3 for saline and the 100 μg/kg ARC19499 dose; n = 6 for the 300 μg/kg dose; and n = 2 for the 600 μg/kg dose.
The aptamer concentration in the plasma from monkeys that received either 300 or 600 μg/kg of ARC19499 was measured using high-performance liquid chromatography. The mean aptamer level was essentially constant, between 0.61 and 0.73μM (6.80 and 8.05 μg/mL), over the posttreatment period in monkeys treated with 300 μg/kg of ARC19499. In the 600 μg/kg group, ARC19499 was sustained at levels between 1.35 and 1.42μM (14.93 and 15.73 μg/mL). These observations suggest a pharmacokinetic elimination half-life in great excess of the 2-hour posttreatment observation period, which is consistent with previous observations for PEG-modified aptamers.36,37
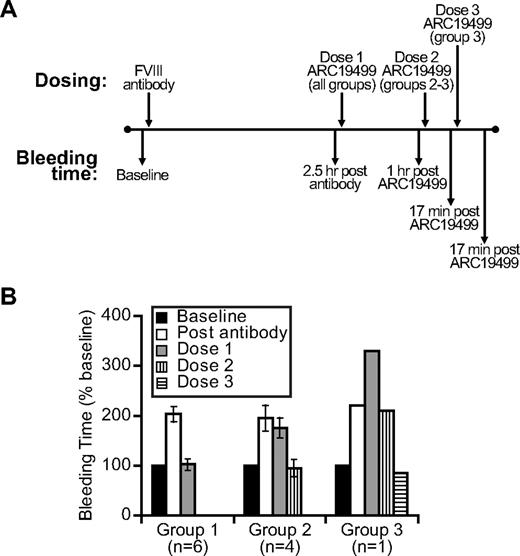
ARC19499 can correct saphenous vein primary bleeding times in a nonhuman primate model of acquired hemophilia A
In addition to examining the correction of TEG values in monkey plasma after the administration of ARC19499, the ability of the aptamer to correct saphenous vein primary bleeding times was assessed. For this assay, 12 healthy cynomolgus monkeys received anti-FVIII antibody to neutralize FVIII activity, generating a hemophilia A–like state. Before antibody administration, the monkeys exhibited normal FVIII activity (58%-94% compared with a standard plasma sample). After antibody administration, activity levels decreased to below measurable levels (< 0.6%) and remained at this level throughout the posttreatment period (data not shown).
The monkey saphenous vein was exposed, punctured with a needle, and the time to bleeding cessation was measured, reflecting the formation of an effective clot. Bleeding time was measured before and after antibody administration to assess baseline bleeding and a FVIII deficiency–induced prolongation, respectively. After antibody administration, monkeys were treated with 1 mg/kg of ARC19499 and bleeding was reassessed. Dose concentrations were selected to expand the dose-response curve beyond that of the previous study evaluating 100-600 μg/kg aptamer doses. Aptamer treatments and bleeding measurements were repeated until the bleeding time was restored to baseline for each monkey. ARC19499-treated monkeys were segregated on the basis of their treatment response. One group of monkeys received 1 dose of ARC19499, 1 group received 2 doses of ARC19499, and 1 group received 3 doses (Figure 7A).
ARC19499 effect on bleeding time in a cynomolgus monkey model of acquired hemophilia A. (A) In vivo dosing scheme used to measure bleeding times in cynomolgus monkeys. (B) Effect of ARC19499 treatment on bleeding time of monkeys that responded to ARC19499. Group 1 received 1 dose of 1 mg/kg ARC19499, group 2 received 2 doses of 1 mg/kg ARC19499, and group 3 received 3 doses of 1 mg/kg ARC19499. Data for groups 1 and 2 represent the means ± SEM.
ARC19499 effect on bleeding time in a cynomolgus monkey model of acquired hemophilia A. (A) In vivo dosing scheme used to measure bleeding times in cynomolgus monkeys. (B) Effect of ARC19499 treatment on bleeding time of monkeys that responded to ARC19499. Group 1 received 1 dose of 1 mg/kg ARC19499, group 2 received 2 doses of 1 mg/kg ARC19499, and group 3 received 3 doses of 1 mg/kg ARC19499. Data for groups 1 and 2 represent the means ± SEM.
All 12 monkeys displayed prolongation of bleeding time after FVIII-antibody administration, as reflected in the mean bleeding time (expressed as a percentage of group mean baseline bleeding time ± SEM) for each group of monkeys (Figure 7B). For all of the monkeys in groups 1 and 2, and for 1 monkey in group 3, mean bleeding times were prolonged roughly 2-fold after antibody administration. The second monkey in group 3 had a 1.4-fold bleeding time prolongation. For the 6 monkeys in group 1, the mean bleeding was corrected to baseline levels after 1 dose of ARC19499 (203% ± 15% after antibody administration, and 102% ± 11% after ARC19499 treatment). For the 4 monkeys in group 2, the mean bleeding time was corrected to baseline levels after 2 doses of ARC19499. After the first dose of ARC19499, the mean bleeding time remained prolonged at 175% ± 20% compared with 195% ± 26% after antibody administration; the second dose of ARC19499 restored the mean bleeding time to baseline levels (94% ± 17%). In group 3, 1 monkey had a bleeding time that was prolonged to 220% of baseline after antibody administration. The first 2 doses of ARC19499 did not shorten the bleeding time, but after the third dose of ARC19499, the bleeding time was returned to 85% (Figure 7B). The bleeding time of the second monkey of group 3 was never corrected even after 3 doses of ARC19499. These results demonstrate that ARC19499 could correct acute bleeding with a variable dose and efficacy response in this nonhuman primate model of hemophilia A.
Discussion
Our results demonstrate that the PEG-conjugated, modified oligonucleotide aptamer ARC19499 is a potent and specific antagonist of TFPI, blocking its inhibition of both TF/FVIIa and FXa, and is an effective procoagulant agent in models of hemophilia both in vitro and in vivo. ARC19499 specifically inhibited TFPI in vitro to restore normal thrombin generation in hemophilia plasma and clot formation in FVIII-depleted whole blood, and in vivo to restore normal clotting parameters and bleeding times in a model of hemophilia in nonhuman primates. These results support the notion that TFPI inhibition is a viable mechanism for hemophilia treatment.
Successful development of this aptamer as a novel therapy for hemophilia could offer improvement compared with current therapies. Most hemophilia treatments are directed at replacing missing or deficient coagulation factors or bypassing the need for these factors by supplying suprapharmacologic doses of TF pathway activators such as recombinant FVIIa.38 However, these proteins are either recombinant or plasma derived,39 and their administration can stimulate inhibitor-antibody development.1 In contrast, aptamers such as ARC19499 are prepared by a scalable synthetic process, resulting in a chemically well-defined molecule and reducing the risk of bacterial or viral contamination and inhibitor induction associated with natural protein products.40 Many hemophilia patients receive prophylactic treatment with replacement factors that requires intravenous infusion 2-3 times weekly. This treatment regimen can negatively impact compliance and increase the risk of infection through the venous access devices.41,42 The bioavailability of aptamers, specifically of ARC19499 (Q. Wang, X. Tian, unpublished observations, May 2009), carries the potential for subcutaneous administration, which would be favorable to patients over intravenous dosing.37,40 Some therapies, including recombinant FVIIa, have relatively short half-lives (∼ 2 hours for recombinant FVIIa)43 and therefore require frequent and often costly infusions. Conversely, the half-life of aptamers can be prolonged by high-molecular-weight PEG conjugation,36 providing the opportunity for less-frequent dosing.
Hemophilia treatment targeting a negative regulator of the clotting cascade, such as TFPI, is an approach that differs from the protein-based replacement and bypass therapies currently used.44,45 Anti-TFPI antibody5 and polysaccharide8,9 TFPI inhibitor studies provide a conceptual foundation for anti-TFPI therapy as a novel hemophilia therapy. These studies suggest that TFPI inhibition has the potential to be useful in improving coagulation in hemophilia patients,5,6,9 both as a single agent and in combination with current replacement factors or bypassing agents. ARC19499 is the first nonprotein molecule to integrate specificity of TFPI inhibition with extended duration of action and the potential for subcutaneous dosing. Further study of ARC19499 in inhibitor and noninhibitor hemophilia A and B patients will demonstrate the scope of its applicability as a hemostatic agent, and will enhance our understanding of the role of TFPI in the regulation of coagulation.
An Inside Blood analysis of this article appears at the front of this issue.
The online version of this article contains a data supplement.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 USC section 1734.
Acknowledgments
We thank DaVinci Biomedical Research for their help in planning and executing the nonhuman primate studies, Dr Saulius Butenas for helpful advice on the FXa activity assay, and Qianfan Wang and Drs Jou-Ku Chung and Xianbin Tian for their help in analyzing aptamer concentrations in the monkey plasma samples.
Authorship
Contribution: E.K.W., J.A.N., R.G.S., K.A.O., J.C.K., and K.E.M designed experiments; E.K.W., R.M.G., M.C.S., J.A.N., R.G.S., and K.A.O performed experiments; all authors analyzed data; and E.K.W., R.G.S., J.C.K., and K.E.M prepared the manuscript.
Conflict-of-interest disclosure: All authors were employees of Archemix Corp during the time this work was completed.
The current affiliation of E.K.W., R.M.G., M.C.S., J.C.K., and K.E.M. is Baxter Healthcare Corporation, Cambridge, MA. The current affiliation of K.A.O. is Aileron Therapeutics, Cambridge, MA.
Correspondence: Kathleen E. McGinness, Baxter Healthcare Corporation, 148 Sidney St, Cambridge, MA 02139; e-mail: kathleen_mcginness@baxter.com.





This feature is available to Subscribers Only
Sign In or Create an Account Close Modal