Abstract
Abstract 1991
Body mass and composition have been well studied in survivors of childhood cancers, but little is known about these factors in those who have undergone allogeneic hematopoietic stem cell transplantation (allo-HSCT).
We prospectively and longitudinally evaluated changes in body mass index (BMI), changes in the proportion of fat and lean body mass, and associated clinical factors in 179 survivors of pediatric hematologic malignancies after allo-HSCT. BMI was analyzed as an ordinal variable (four percentile categories: underweight, healthy weight, overweight, and obese) and as a continuous variable (Z-score); dual-energy X-ray absorptiometry data were used to derive Z-scores for percent total body fat and lean mass/height2 ratio.
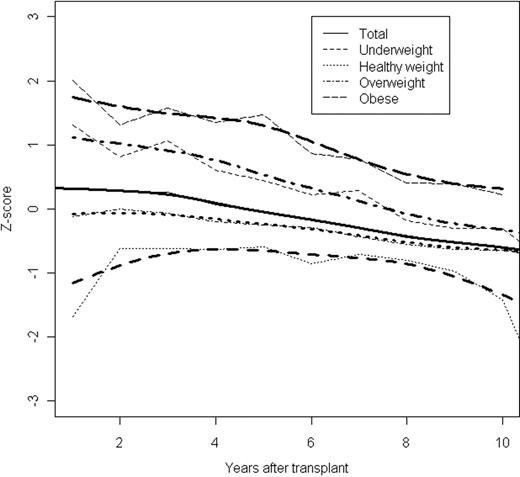
With a median follow-up of 6.6 years (range, 1.0–17.7 years), BMI decreased significantly over time (mean Z-score, 0.32 pre-HSCT and −0.60 at 10 years post-HSCT) (Figure; p<0.001). These longitudinal changes differed among pre-HSCT BMI categories (p<0.001). BMI Z-scores of patients who were underweight before HSCT increased over the first 4 years after HSCT and then declined, while those of patients in the other three pre-HSCT BMI categories continuously declined. Although the mean Z-scores for percent fat mass were higher or similar to those of the general population during follow-up (0.305 at 1 year, −0.272 at 10 years), the mean Z-scores of lean mass/height2 ratio remained below that of healthy controls and diminished significantly over time (-0.296 at 1 year, −1.256 at 10 years post-HSCT) (p=0.002). Pre-HSCT BMI categories were strongly associated with post-HSCT BMI values (p<0.001) and with Z-scores of percent total body fat and lean mass/height2 ratio (both p<0.001). Patients who had extensive chronic graft-versus-host disease were significantly more likely to be in the underweight BMI category (p=0.021) and to have a low Z-scores for lean mass/height2 ratio (p<0.001). Younger patients (less than the median age, 11.3 years, at HSCT) had a higher BMI after HSCT than older patients (p<0.001), and female survivors had higher Z-scores of percent total body fat (p=0.005) and lower Z-scores of lean mass/height2 ratio (p=0.025) than male survivors.
The finding of a significant decline of BMI and severe loss of lean mass after HSCT indicates a critical need for nutritional education and early intervention for these survivors.
Longitudinal changes in BMI after HSCT in all patients (Total), and in patients who were underweight, healthy weight, overweight, or obese categories before HSCT. The narrow lines connect the observed mean Z-scores, while the corresponding broader lines represent the statistically smoothed curve.
Longitudinal changes in BMI after HSCT in all patients (Total), and in patients who were underweight, healthy weight, overweight, or obese categories before HSCT. The narrow lines connect the observed mean Z-scores, while the corresponding broader lines represent the statistically smoothed curve.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal