Abstract
Abstract 2017
Multiple myeloma (MM) remains an incurable disease and is the most common hematologic malignancy among African-Americans. In the United States, MM and its precursor monoclonal gammopathy of undetermined significance (MGUS) are twice as common in African Americans (Hari et al 2010). Analysis of the Surveillance Epidemiology and End Results (SEER) database from 1969 to 2003 demonstrated African-Americans have twice the mortality from MM compared to Caucasians. However this may be a function of the considerable difference in incidence of MM between Caucasian and African-American populations. Retrospective data from Southwest Oncology Group showed comparable outcomes between groups before the advent of autologous stem cell transplantation (auto-HCT). Recently Hari et al. determined that African-American and Caucasians have similar outcomes after auto-HCT for MM. In the age of novel therapy, Waxman et al addressed racial disparity in population based query of SEER and found disease specific survival was greater for African-Americans than Caucasians; and over time, survival improvement was much less pronounced among African-Americans than Caucasians. Nevertheless transplant specific data is sparse in the contemporary era with novel treatment options.
We performed a retrospective review of 196 African-American multiple myeloma patients (pts) and 806 Caucasian patients initially seen at the M.D. Anderson Cancer Center from 1/1/2002 to 12/31/2010 who underwent autologous transplantation after high dose chemotherapy. The year 2002 was used to incorporate patients who had been exposed to novel agents.
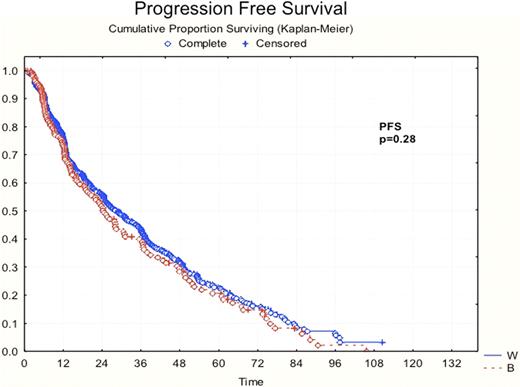
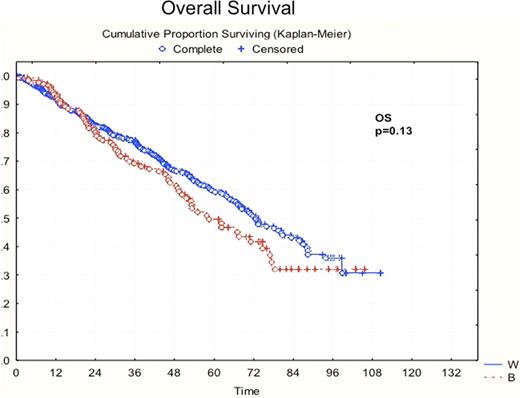
A total of 1002 patients were analyzed, 196 African American and 806 Caucasian pts with multiple myeloma who underwent an autologous transplant. Median age at diagnosis was 59 years for both cohorts. Initial response prior to transplant was fairly evenly matched between groups (TABLE 1) as well as final response after transplant. 25% of Caucasian pts and 21% of African-American pts achieved a very good partial response (VGPR) while 28% of Caucasian and 21% of African-American pts achieved a complete response (CR). For evaluable patients, the International Staging System (ISS) at diagnosis was determined. The percentage of stage I, II and III patients in the African-American group was 27%, 20% and 17% respectively. The percentage of stage I, II and III patients in the Caucasian group was 26%, 19% and 17% respectively. Importantly 133/806 of Caucasians and 33/196 of African Americans were diagnosed at ISS stage III (p value=0.91). There was no measurable difference in progression free survival (figure 1) or overall survival (figure 1figure 2) with a maximum follow-up of >100 months.
| . | Caucasian (n = 806) . | African-American (n = 196) . |
|---|---|---|
| Median age at auto-HCT | 59 (31–80) | 59 (34–78) |
| Age over 65 at auto-HCT | 178/806 (22%) | 26/196 (13%) |
| Response prior to transplant | PD = 46 (6%) | PD = 13 (6%) |
| SD = 68 (8%) | SD = 12 (6%) | |
| MR = 29 (3. 5%) | MR = 11 (6%) | |
| PR = 437 (54%) | PR = 102 (52%) | |
| VGPR = 179 (23%) | VGPR = 38 (19%) | |
| CR = 35 (4%) | CR = 13 (7%) | |
| Untreated = 2 (0. 2%) | Unknown = 7 (4%) | |
| Unknown = 10 (1. 3%) | ||
| Median time from diagnosis to transplant | 237 days (51– 7985) | 238 days (83 – 6495) |
| Final Response | PD = 24 (3%) | PD = 9 (5%) |
| < PR = 90 (11%) | < PR = 32 (16%) | |
| PR = 260 (32%) | PR = 69 (35%) | |
| VGPR = 198 (25%) | VGPR = 42 (21%) | |
| CR = 227 (28%) | CR = 41 (21%) | |
| Unknown = 7 (1%) | Unknown = 3 (2%) | |
| ISS score | I = 210 (26%) | I = 52 (27%) |
| II = 157 (19%) | II = 39 (20%) | |
| III = 133 (17%) | III = 33 (17%) | |
| Unknown = 306 (38%) | Unknown = 72 (36%) | |
| Median PFS | 36 months | 34 months |
| Median OS | 46 months | 48 months |
| . | Caucasian (n = 806) . | African-American (n = 196) . |
|---|---|---|
| Median age at auto-HCT | 59 (31–80) | 59 (34–78) |
| Age over 65 at auto-HCT | 178/806 (22%) | 26/196 (13%) |
| Response prior to transplant | PD = 46 (6%) | PD = 13 (6%) |
| SD = 68 (8%) | SD = 12 (6%) | |
| MR = 29 (3. 5%) | MR = 11 (6%) | |
| PR = 437 (54%) | PR = 102 (52%) | |
| VGPR = 179 (23%) | VGPR = 38 (19%) | |
| CR = 35 (4%) | CR = 13 (7%) | |
| Untreated = 2 (0. 2%) | Unknown = 7 (4%) | |
| Unknown = 10 (1. 3%) | ||
| Median time from diagnosis to transplant | 237 days (51– 7985) | 238 days (83 – 6495) |
| Final Response | PD = 24 (3%) | PD = 9 (5%) |
| < PR = 90 (11%) | < PR = 32 (16%) | |
| PR = 260 (32%) | PR = 69 (35%) | |
| VGPR = 198 (25%) | VGPR = 42 (21%) | |
| CR = 227 (28%) | CR = 41 (21%) | |
| Unknown = 7 (1%) | Unknown = 3 (2%) | |
| ISS score | I = 210 (26%) | I = 52 (27%) |
| II = 157 (19%) | II = 39 (20%) | |
| III = 133 (17%) | III = 33 (17%) | |
| Unknown = 306 (38%) | Unknown = 72 (36%) | |
| Median PFS | 36 months | 34 months |
| Median OS | 46 months | 48 months |
PD: progressive disease SD: stable disease MR: minimal response PR: partial response
VGPR: very good partial response CR: complete response
In this retrospective single-center study we demonstrated no difference in progression free survival or overall survival between African-American and Caucasian patients with MM treated in the era of novel agents and autologous stem cell transplantation. These findings concur with previous studies showing no difference in response to treatment between racial groups. In light of older SEER data this may be an effect of novel agents, improved access of care for African Americans or a combination of both.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal