Abstract
Abstract 2026
High-dose therapy (HDT) and autologous stem cell transplantation (ASCT) is frequently employed to improve outcomes in patients with mantle cell lymphoma (MCL), yet results after transplant vary widely. We and others have shown that the Mantle Cell International Prognostic Index (MIPI) measured at diagnosis can predict overall survival (OS) after HDT and ASCT (Geisler, Blood 2010; Budde JCO 2011). Unfortunately, this approach is often limited at the time of transplant by the lack of available MIPI data from the time of diagnosis. Furthermore, the MIPI at diagnosis does not take into account other disease-related data that may be present at transplant. We hypothesized that the MIPI measured immediately before initiation of HDT could be attainable and predictive of outcomes after ASCT and explored the contribution of this measure along with other clinical factors to OS and progression-free survival (PFS).
Records of consecutive MCL patients undergoing HDT and ASCT at our centers were reviewed under an IRB approved minimal risk protocol. Patients undergoing planned tandem autologus-allogenic transplants were excluded. MIPI elements, simplified MIPI score, and other clinical data were collected from the period immediately prior to initiation of conditioning and evaluated for their independent association with OS and PFS.
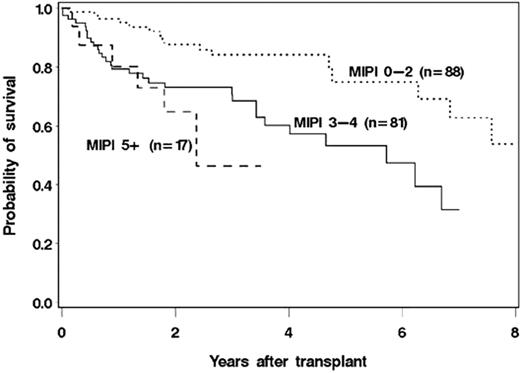
Between November 1995 and May 2011 190 MCL pts meeting the above criteria underwent HDT and ASCT at our centers, of these 186 (98%) had all available pretransplant MIPI data and were included in the analysis. Pretransplant MIPI scores of 0–1, 2, 3, 4, and 5–7 were seen in 27 (15%), 61 (33%), 60 (32%), 21 (11%), and 17 (9%) patients, respectively. Other baseline pretransplant characteristics included: median age 57 years (range 35–71years), elevated LDH = 48 (26%), median WBC = 4.51/μL (range 0.7 –42.43/μL), performance score 0 = 103 (55%), median prior regimens = 2 (range 1–9), blastoid variant = 16 (8%), leukemic variant = 6 (3%), chemosensitive disease = 157 (86%), and administration of rituximab (R) within 3 months prior to transplant = 139 (75%). The 8-year estimates of OS and PFS for the entire cohort were 43% (95% CI 27 – 57%) and 31% (95% CI 16 – 48%), respectively with 3 years median follow up for survivors. The pretransplant MIPI was highly associated with OS when modeled as a continuous (p=0.008) or categorical variable (p=0.002). Survival at 2 years was 88% (95% CI 78 – 93%) for MIPI 0–2, 73% (61 – 82%) for MIPI 3 or 4, and 65% (34 – 84%) for MIPI 5 or greater (Figure). Of the MIPI elements, age (hazard ratio [HR] for death 1.5 for every 10 yrs, p=0.03) and performance score (HR 1.6 for score >1, p=0.08) had the greatest independent impact on OS. In addition, chemosensitive disease (HR 0.3, p<0.001), number of prior regimens (p<0.001), and R within 3 months prior to transplant (HR 0.6, p=0.05) were all independently associated with OS after adjusting for the pretransplant MIPI.
The pretranplant MIPI score was also predictive of PFS, but less so than with OS (global and categorical p=0.02) with age providing the greatest independent association (HR for death or progression 1.3 for every 10 years, p=0.08). Again, non-MIPI factors including number of prior regimens (p<0.001), blastoid variant (HR=2.1, p=.05), chemosensitive disease (HR 0.3, p<0.001), and R within 3 months prior to transplant (HR=0.4, p=0.001) independently added to predictive ability of the MIPI for PFS.
Our data suggest that the simplified MIPI score measured immediately prior to HDT and ASCT is a readily available and robust predictive tool for OS and PFS in MCL pts undergoing transplant. This score along with other clinical factors can be utilized to counsel patients and to compare results between various treatment options. The independent association of pretransplant R with improved outcomes supports its use in this setting.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal