Abstract
Abstract 2032
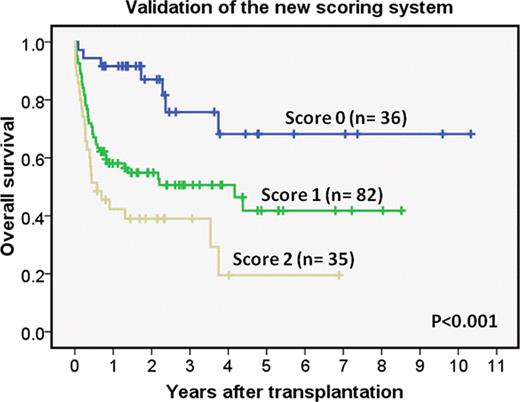
Recent studies have suggested that iron overload is one of important predictors for outcome in allogeneic hematopoietic stem cell transplantation (allo-HSCT). We previously reported that a new scoring system by combination with pre-transplant serum ferritin (SF) and disease risk is useful for predicting outcome in patients with acute myeloid leukemia (AML) and myelodysplastic syndrome (MDS) who underwent allo-HSCT at Kanagawa Cancer Center (KCC) (Bone Marrow Transplantation 46: 150–151, 2011). To clarify the availability of this scoring system in another cohort, we performed a validation in multicenter study.
We retrospectively collected clinical data of adult patients with AML and MDS who received allo-HSCT between 2000 and 2010 at three institutes. The patients analyzed in the previous study were excluded. Pre-transplant SF value was categorized as low-SF (<1000 ng/ml) and high-SF (≥1000 ng/ml) according to the previous report. First/second complete remission in AML and refractory anemia in MDS were defined as standard disease risk and others were defined as high risk. Pre-transplant SF and disease risk were each assigned a score, and the sum total was tested as prognostic score based on three risk groups: low (score=0), intermediate (score=1) and high (score=2). The log-rank test was used for comparisons of Kaplan-Meier curves. Cox regression model was used for multivariate analyses.
A total of 153 patients were analyzed. Their median age was 48 years old (range: 17–65), with 57 males and 96 females. Related or unrelated bone marrow (n=106), related peripheral blood stem cell (n=14) or unrelated cord blood (n=33) were transplanted as stem cell sources. Myeloablative conditioning regimens were used in 112 patients while reduced-intensity regimens in 41. The median level of pre-transplant SF was 1,139 ng/ml (range:22–6,262) in all patients. Standard and high disease risks were 82 and 71 patients, respectively. There were no significant differences of patient characteristics among the three institutes except pre-transplant SF level. The median follow-up period among survivors was 25.9 months (range: 7.1–124). Univariate analysis for 5-year overall survival (OS) demonstrated an inferior outcome in patient with high SF (41% vs. 48%, p=0.025) or high disease risk (21% vs. 61%, p<0.001), compared with low SF or standard disease risk, respectively. Multivariate analysis for 5-year OS demonstrated high SF (HR: 1.794, 95% CI: 1.11–2.91, p=0.018) and high disease risk (HR: 2.08, 95% CI: 1.26–3.41, p=0.004) at transplantation as inferior prognostic predictors. According to the scoring system with pre-transplant SF and disease risk, the 5-year OS of the low (n=36), intermediate (n=82) and high (n=35) risk group was 68%, 42% and 20%, respectively (p<0.001).
The usefulness of the simple scoring system with pre-transplant SF and disease risk was validated by the multicenter analysis. This prognostic scoring system might help to stratify patients in clinical studies and choose patients for iron chelating therapy.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal