Abstract
Abstract 2038
Anti-HLA antibodies are associated with several complications in solid organ transplantations but their impact after allogeneic hematopoietic stem cell transplantation (HSCT) is not very well defined yet.
To evaluate the relevance of anti-HLA antibodies, we have retrospectively analyzed 107 peripheral blood allogeneic HSCT after reduced-intensity conditioning (RIC) regimen between 2005 and 2010. Acute myeloid leukaemia (n=52,48.5%) and multiple myeloma (n=18,17%) were the most common diagnosis in the cohort. The detection of anti-HLA antibodies was systematically performed in all patients before transplantation.
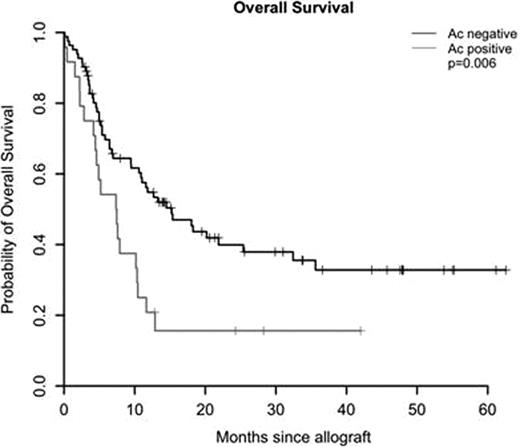
We found in 24 patients (22%) the presence of anti-HLA antibodies. There was no association between the presence of anti-HLA antibodies and engraftment, incidence of relapse or acute GvHD. The presence of anti-HLA antibodies was associated with worse survival in univariate analysis (HR 2.04; [95%CI,1.21–3.44], p=0.0056) and in multivariate analysis (HR 2.63; [95%CI, 1.32–5.25], p=0.006). The 3-year probability of OS was 34% (95%CI, 24–49) without anti-HLA antibodies and 16% (95%CI, 6–41) in their presence (Figure 1). The other significant factors on survival were the disease status at transplantation, the age, minor and major ABO incompatibilities between donor and recipient, the sex-mismatching and the CMV status. Moreover, the positive anti-HLA antibodies group showed a trend of higher TRM in univariate analysis (p=0.07) and in multivariate analysis (HR= 1.9; [95%CI, 0.94 – 3.9], p=0.076). The TRM at 3 years after transplantation were 31% (95%CI, 26–37) without anti-HLA antibodies and 46% (95%CI, 36–57) in their presence (figure 2). The causes of the pejorative effect of the anti-HLA antibodies were not defined yet but we observed microangiopathy associated with vascular endothelium damage which could be related to the presence of anti-HLA antibodies.
Our study suggests that anti-HLA antibodies should be tested and considered as an important prognostic factor for transplant outcomes after RIC HSCT.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.


This feature is available to Subscribers Only
Sign In or Create an Account Close Modal