Abstract
Abstract 2702
Tumor Lysis Syndrome (TLS) is a potentially life-threatening metabolic syndrome that frequently complicates the management of newly diagnosed mature B-NHL in children and adults (Cairo et al., BJH 2010). We have demonstrated rasburicase to be superior to allopurinol in the rapid reduction of uric acid (UA). (Goldman/Cairo et al, Blood 2001) In the previous FAB/LMB/96 international mature B-NHL trial, variables associated with a significant inferior EFS included advanced stage, elevated LDH, primary mediastinal involvement (PMBL) and combined BM/CNS disease (Cairo et al, JCO, 2011). We have previously reported the pharmacokinetics and safety of the addition of rituximab to a modified FAB/LMB/96 backbone in children and adolescents with advanced stage mature de-novo B-NHL. (Cairo et al., ASCO, 2010) Here we focus on outcome in those specific high-risk sub-categories of advanced childhood mature B-NHL following the incorporation of a recombinant urate oxidase (Rasburicase) and targeted immunotherapy (Rituximab) to the FAB/LMB/96 chemotherapy backbones.
Children with newly diagnosed stage III/IV or high-risk (BM+±CNS+) de-novo mature B-NHL were prospectively treated with cyclophosphamide, vincristine, and prednisone (COP) reduction therapy preceded by 4–24 hours of non-alkaline hydration and rasburicase (0.2mg/kg) (generously supplied by Sanofi-Aventis). Laboratory and clinical TLS (LTLS and CTLS) was prospectively monitored as previously defined (Cairo & Bishop, BJH, 2004). Immunochemotherapy consisted of FAB B4 or C1 therapy (adriamycin 1 hr infusion) as we have previously described (Patte et al and Cairo et al, Blood, 2007) with the addition of rituximab 375 mg/m2/dose (generously supplied by Genentech) with 2 doses administered in each induction cycle and 1 dose in each consolidation cycle.
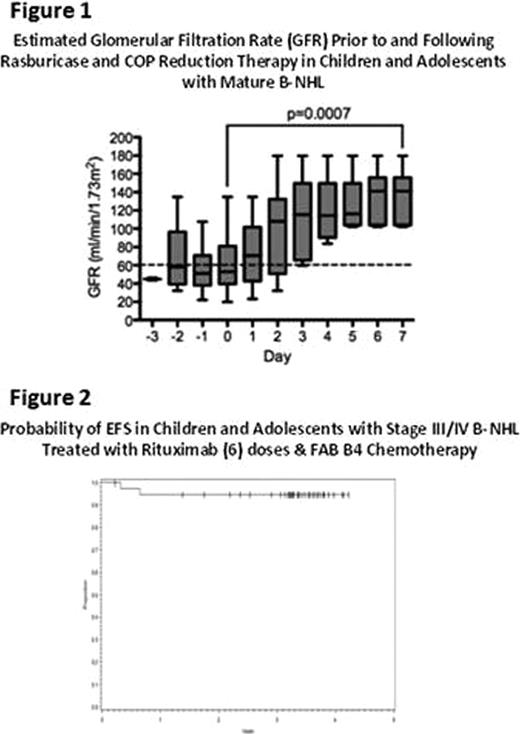
With respect to LTLS and CTLS, 78 patients were evaluable: group B (stage III/IV) with NL-LDH (<2X ULN, n=23), Group B with HI-LDH (≥ 2X ULN, n=18), and Group C (n=37). The mean initial UA levels (mg/dl +/− SD) were 4.7±2, 8.7±4.6, and 7.1±4.6, respectively. At presentation, 31% of patients (all groups) had an elevated (> 8mg/dl) UA, and 47% received elective doses of rasburicase in the days prior to the first day of chemotherapy. The incidence of LTLS prior to rasburicase in Group B NL-LDH, Group B HI-LDH, and Group C, was 4.3%, 5.5%, and 16.6%, respectively. The incidence of CTLS prior to rasburicase was 0%, 11%, and 8.6%, respectively. Following the administration of rasburicase, the incidence of new onset LTLS and CTLS for the entire cohort was 13% (2.6% with hyperuricemia) and 4% (1% with hyperuricemia), respectively. Furthermore, there was a significant improvement in the estimated GFR in those with renal impairment from day -1 prior to rasbursicase to day+7 post R-COP (55 ± 29 ml/min1.73 m2 to 136 ± 29 respectively; p<0.0007; Figure 1). Following combined FAB 96 chemotherapy (with 1 hour Adriamycin) and rituximab, the 3- year EFS (95% CI) for pilot patients (6 doses of rituximab) with Stage III/IV and Group C BM/CNS patients were 95% (80–99%) (Figure 2) and 89% (73–98%), respectively. Interestingly, two of four patients with centrally reviewed mediastinal primaries developed recurrent disease, while none of the 19 stage III/IV patients with LDH < 2X ULN developed recurrent disease or toxic deaths.
Rasburicase and non-alkaline hydration largely prevented (94% of the time) new onset TLS with hyperuricemia safely during COP reduction therapy in children with advanced stages of de-novo mature B-NHL. For patients with mediastinal primaries, the high failure rate with group B4 therapy + rituximab suggests it would be appropriate to investigate new treatment strategies. Excluding this histology, combined modified FAB/LMB 96 chemotherapy and rituximab resulted in only 5 deaths (2 toxic deaths, 3 disease related deaths) among our cohort of 62 with advanced mature B-NHL. In comparing these current results from the previous FAB/LMB 96 trial without rituximab, the stage III/IV patients had a 95% vs. 84% and patients with CNS+ disease a 93% vs. 72% 3 year EFS. (Patte et al., Cairo et al. Blood, 2007) Future efforts to intensify chemotherapy in patients with CNS involvement should proceed only with careful toxicity monitoring, as preliminarily these patients seem to have excellent outcome with this immunochemotherapy approach.
Gross:Pfizer Oncology: Consultancy; Roche/Genentech: Consultancy; Eli Lilly: Consultancy.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal