Abstract
Abstract 2762
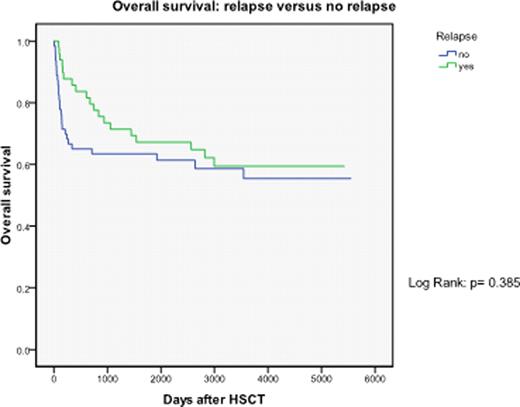
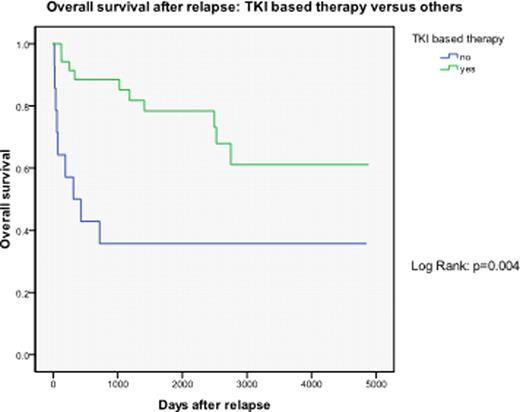
Although SCT is now uncommon treatment for CML, many patients transplanted for CML have become long term survivors and some continue to relapse late post transplant. It is therefore important to evaluate the management of relapse in CML transplant survivors in the era of TKI treatment. We studied 112 patients with Ph+ CML who underwent HLA identical sibling SCT between 1993 to 2008. The mean age was 36 years (range 13–69). Eighty (71%) were in chronic phase, 17 in accelerated phase, 5 in second chronic phase and 10 in blastic phase. Ninety-nine (88%) received myeloablative conditioning regimen with cyclophosphamide +/− fludarabine and total body irradiation and 13 received a non-myeloablative regimen. GVHD prophylaxis was with cyclosporine. Bone marrow or G-CSF mobilized peripheral blood stem cells from the donor were manipulated to achieve 4-log CD3+ cell reduction ex vivo. Peripheral blood BCR-ABL p210 product was regularly monitored by either double nested PCR (until 2003) or real time PCR (2003 to present). For molecular relapse, patients received donor lymphocyte infusions (DLI) with or without imatinib 400–600mg/day. Patients with hematological relapse received a variety of treatments including second SCT. At a median follow up of 6.2 years, 10 year-relapse free survival and overall survival were 34% and 57% respectively. Overall 49 (43.8%) patients relapsed, 28 with molecular and 22 with hematological relapse. Median time to relapse from HSCT was 379 days (range 16–3718 days). Overall survival was not significantly different between relapsed patients and non-relapsed patients. (10-year OS: 59 % vs 55%, P=0.385). Thirty-five relapsed patients (71.4%) were treated with TKI based therapy. Overall survival after relapse was significantly better after TKI based therapy compared to non-TKI based therapy. (5-year survival after relapse: 78% vs 36%, P=0.004 respectively). The benefit of TKI was greater in hematological relapse (median survival after hematological relapse 1182 days in TKI based vs 72 days in others P=0.025). At 7 years median follow up after relapse, 27 (96.4%) patients with molecular relapse are alive in major molecular remission and 20 (71%) no longer receive TKI. These results show that the outlook for relapse after SCT for CML is favorable in the TKI treatment era and that combination of TKI and DLI can achieve long-term disease free survival post relapse.
Disclosures:
No relevant conflicts of interest to declare.
Author notes
*
Asterisk with author names denotes non-ASH members.
© 2011 by The American Society of Hematology
2011

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal