Abstract
Abstract 333
Impact of Non High-Risk Chromosomal Abnormalities on the Outcome of Autologous Hematopoietic Stem Cell Transplantation in Multiple Myeloma
Despite novel therapeutic agents and high-dose chemotherapy with autologous hematopoietic stem cell transplantation (auto-HCT), most patients eventually progress and die of their disease. Recent advances in cytogenetic, molecular and genomic studies have led to identification of several chromosomal and molecular abnormalities. These abnormalities are important predictors of response to therapy, progression-free survival (PFS) and overall survival (OS). On conventional cytogenetic (CC) analyses, del 13, t(4;14), t(14;16) and del 17p are considered high-risk (HR). On Fluorescence in situ hybridization (FISH) analysis, all except del 13 are considered HR (Munshi, N et al. Blood 2011 117: 4696–4700). However there are a number of chromosomal abnormalities whose significance is not clearly identified (non-HR). In this study we report the impact of these non-HR chromosomal abnormalities on the outcome of patients who received high-dose chemotherapy and auto-HCT.
We performed a retrospective review of patients with multiple myeloma who underwent high dose chemotherapy followed by auto-HCT at the M.D. Anderson Cancer Center. Between 10/1991 and 12/2010, 1570 patients received auto-HCT. The results of CC studies were available for 1329 patients, either at diagnosis or at relapse, but before auto-HCT. The primary objective was to study the impact of non-HR chromosomal abnormalities on PFS and OS, and to compare them to patients without chromosomal abnormalities.
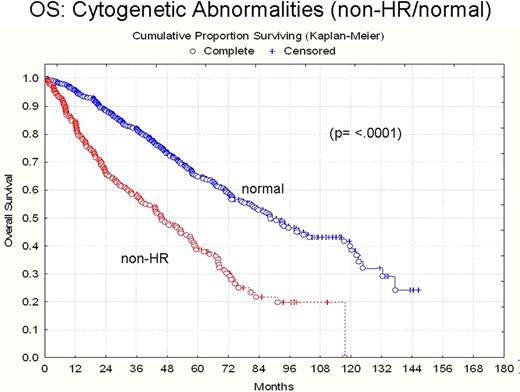
Patient characteristics and major outcomes are summarized in the attached Table. In 1329 patients with available CC analyses before auto-HCT, chromosomal abnormalities were identified in 405 (30%) patients. One-hundred and seven (7%) patients had known HR chromosomal abnormalities, while 298 (23%) patients had non-HR chromosomal abnormalities. Fifty (17%) patients with non-HR chromosomal abnormalities and 296 patients (32%) with normal CC achieved complete or stringent complete responses (CR + sCR) (p=0.0001). Median follow up in surviving patients was 36 months. Median PFS in patients with non-HR chromosomal abnormalities and normal CC were 18.2 months (95%CI: 16–22.7) and 32.7 months (95% CI: 27.8–36.3), respectively (p= <.0001) (Figure 1). The OS in patients with non-HR chromosomal abnormalities and with normal CC were 56.5 months (95% CI: 43.2–66.9) and 87.2 months (95%CI: 80.1–102.4), respectively (p= <.0001) (Figure 2).
In this large single center study with a long follow up, we demonstrated that non-HR chromosomal abnormalities in myeloma are associated with a lower CR rate and shorter PFS and OS after auto-HCT. Further studies are needed to better define these non-HR abnormalities and their impact on prognosis.
| . | Normal (n= 924) . | Non-High Risk (n= 298) . |
|---|---|---|
| Median age at auto-HCT | 57 | 59 |
| Age >65 at auto-HCT | 137/924 (14.8%) | 70/298 (23.4%) |
| Race | White = 605 (65%) Black = 148 (16%) Other = 171 (19%) | W = 202 (67%) B = 44 (14%) O = 52 (19%) |
| Gender | Female = 391 (42%) Male = 533 (58%) | F = 104 (34%) M = 194 (66%) |
| Disease status at transplant | First Remission = 799 (86%) Relapsed: 110 (12%) Unknown = 15 (2%) | First Remission = 224 (75%) Relapsed = 72 (24%) Unknown = 2 (1%) |
| Conditioning Regimen | Melphalan or non melphalan = 198 (79%) Melphalan alone = 726 (21%) | Melphalan or non melphalan = 57 (81%) Melphalan alone = 241 (19%) |
| Final Response | PD = 17 (1.8%) <PR = 132 (14%) PR = 278 (30%) VGPR = 194 (20%) CR = 221 (23%) sCR = 75 (8.1%) Unknown = 7 | PD = 20 (6.7%) <PR = 45 (15%) PR = 103 (34%) VGPR = 73 (24%) CR = 34 (11%) sCR = 16 (5%) Unknown = 7 |
| Progressed | 447/924 (48%) | 172/298 (57%) |
| Died | 278/924 (30%) | 123/298 (41%) |
| . | Normal (n= 924) . | Non-High Risk (n= 298) . |
|---|---|---|
| Median age at auto-HCT | 57 | 59 |
| Age >65 at auto-HCT | 137/924 (14.8%) | 70/298 (23.4%) |
| Race | White = 605 (65%) Black = 148 (16%) Other = 171 (19%) | W = 202 (67%) B = 44 (14%) O = 52 (19%) |
| Gender | Female = 391 (42%) Male = 533 (58%) | F = 104 (34%) M = 194 (66%) |
| Disease status at transplant | First Remission = 799 (86%) Relapsed: 110 (12%) Unknown = 15 (2%) | First Remission = 224 (75%) Relapsed = 72 (24%) Unknown = 2 (1%) |
| Conditioning Regimen | Melphalan or non melphalan = 198 (79%) Melphalan alone = 726 (21%) | Melphalan or non melphalan = 57 (81%) Melphalan alone = 241 (19%) |
| Final Response | PD = 17 (1.8%) <PR = 132 (14%) PR = 278 (30%) VGPR = 194 (20%) CR = 221 (23%) sCR = 75 (8.1%) Unknown = 7 | PD = 20 (6.7%) <PR = 45 (15%) PR = 103 (34%) VGPR = 73 (24%) CR = 34 (11%) sCR = 16 (5%) Unknown = 7 |
| Progressed | 447/924 (48%) | 172/298 (57%) |
| Died | 278/924 (30%) | 123/298 (41%) |
PD: Progressive Disease PR: Partial Remission CR: Complete Response
VGPR: Very Good Partial Response sCR: Stringent Complete Response
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.


This feature is available to Subscribers Only
Sign In or Create an Account Close Modal