In this issue of Blood, Harrison and coworkers report on toxicity and efficacy observed with a novel antimyeloma triple combination of romidepsin (a histone deacetylase [HDAC] inhibitor), bortezomib, and dexamethasone in 25 previously treated patients.1
The number of noncytotoxic drugs featuring significant single-agent activity in relapsed or relapsed and refractory (disease progression during treatment or within 60 days of its termination) myeloma is clearly limited.2 The proteasome inhibitors and the imunomodulatory derivatives of thalidomide (IMiDs) have proven effective, with several compounds already in routine clinical care. As duration of response to either drug or drug combination is restricted, further options are needed.
Next-generation novel agents that claimed to more precisely target oncogenic signaling pathways in the myeloma cell have, however, often failed to produce antitumor responses in the clinical setting. This is also true with the initial experience with single-agent inhibitors of HDACs in myeloma.2,3
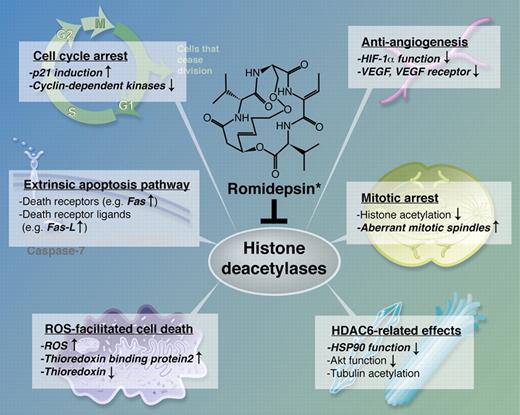
Four histone core proteins together with DNA form the structure of chromatin. Histones can be deacetylated via HDACs while their counterparts, histone acetyltransferases, increase the extent of acetylation of histone lysine residues.4 Neutralizing the positively charged lysines via acetylation results in a reduced attraction of DNA and, therefore, less condensed chromatin structure. This is thought to facilitate DNA access by transcription factors and RNA polymerase.5 In addition to histones, a considerable number of nonhistone proteins (ie, DNA binding transcriptional factors; signaling mediators; DNA repair enzymes, chaperone protein) were identified as HDAC substrates. The overall effects of pharmacologic HDAC inhibition on malignant cells in vitro (cell-cycle arrest; activation of apoptosis; induction of reactive oxygen species; and antiangiogenesis; see figure)4 prompted the evaluation of deacetylase inhibitors in clinical trials in various malignancies. Relatively early during its clinical development in 2001, the only member of the cyclic peptide class, romidepsin, turned out to be effective in treating patients with T-cell non-Hodgkin lymphomas (NHLs). In contrast to a single-agent phase 2 trial in advanced cutaneous NHLs where the compound yielded a 38% objective response,6 a similar myeloma study failed to demonstrate activity.3 Considering the lack of objective remission and only a 31% stable disease (SD) rate in the latter trial, another single-agent trial of romidepsin in recurrent myeloma did not appear attractive. Now that Harrison and colleagues have demonstrated an overall response rate of 60% to their novel triplet of romidepsin, bortezomib, and dexamethasone,1 one may conclude that HDAC inhibition may be ready for a comeback. Their trial was designed innovatively in that a so-called “accelerated dose escalation schedule” partially replaced the classic 3 + 3 dose escalation. It was chosen to avoid treatment of patients well below the effective dose, however, with an increased risk of unanticipated toxicities. The study included patients with at least one prior antimyeloma treatment (bortezomib permitted if it had been effective) and adequate bone marrow and organ function. The primary end point was to determine the maximum tolerated dose (MTD) of romidepsin/bortezomib/dexamethasone; secondary end points were efficacy variables and survival. The study protocol foresaw the “conventional” administration of bortezomib/dexamethasone: bortezomib 1.3 mg/m2 as an intravenous push on cycle days 1, 4, 8, and 11 along with dexamethasone 20 mg on every bortezomib day and the day after. Dose escalation was restricted to romidepsin. The starting dose of 8 mg/m2 intravenously on days 1, 8, and 15 was to be increased in 2-mg increments. A cycle length of 28 days was chosen and romidepsin maintenance was available for responding subjects on days 1 and 8 of every 4-week cycle. In all, 25 patients with a median of 2 prior lines of therapy (range, 1-3) were enrolled in the study. Pretreatment intensity appeared moderate with only half of the patients having received prior autologous transplant and IMiDs, respectively; 24% had a history of bortezomib exposure. When 2 subjects receiving the HDAC inhibitor at 12 mg/m2 experienced dose-limiting toxicities (DLTs), the MTD turned out to be romidepsin 10 mg/m2 on days 1, 8, and 15 along with bortezomib/dexamethasone. This dose is well below that (14 mg/m2) used when romidepsin is given as a single agent in cutaneous T-cell lymphomas. This was the first indication approved by the US Food and Drug administration in 2009.
Romidepsin-mediated HDAC inhibition enhances myeloma cell death via several mechanisms (adapted from Xu et al4 ). Professional illustration by Alice Y. Chen.
Romidepsin-mediated HDAC inhibition enhances myeloma cell death via several mechanisms (adapted from Xu et al4 ). Professional illustration by Alice Y. Chen.
Thrombocytopenia is an overlapping toxicity between bortezomib and romidepsin and had been anticipated by the investigators. Severe (Common Terminology Criteria for Adverse Events [CTC AE] grade 3 and higher) thrombocytopenia at MTD level was 58%. Even with this level of toxicity, there was 1 fatal hemorrhage that was attributable to disease progression but not to study drug treatment, and no other bleeding episodes were reported. Incidence of nonfebrile neutropenia (CTC AE grade 3 and higher) at MTD was 36%. The main nonhematologic toxicity was bortezomib-induced peripheral neuropathy (PNP) in 76% of patients. Incidence of clinically relevant PNP without improvement after interruption of bortezomib was 20%. Incidences of all other severe nonhematologic toxicity except hyponatremia and fatigue were below 10%. Overall response rate (ORR) according to the International Myeloma Working Group uniform response criteria (partial response [PR] or better) was 60%, including a very good PR plus complete response rate of 36%, which is quite impressive for this setting. Response rates with single-agent HDAC inhibitors, as mentioned earlier, were far below that,3,7 as were those seen in the SUMMIT trial: single-agent bortezomib induced an ORR of 35%.8
Considering results from those 3 studies, the activity reported by Harrison et al suggests a synergism of romidepsin and bortezomib in myeloma.1 And indeed, very recently Kikuchi and colleagues in this journal reported on a clear synergistic effect of bortezomib and romidepsin in vitro.9 Furthermore, Kikuchi et al demonstrated that bortezomib transcriptionally down-regulates class I HDACs while romidepsin seems able to inhibit both class I and II enzymes and suggested HDAC inhibition may be important in the efficacy of bortezomib in multiple myeloma. They proposed to further investigate bortezomib-HDAC combinations.9
While several clinical trials are still ongoing, the study by Harrison and colleagues is the first fully published trial supporting this combinatorial approach: the synergism that had previously been observed in vitro translated to superior response rates in the clinical setting.1 The 7-month duration of response, however, was disappointing. This observation leads to the question on how to dose-modify the regimen (bortezomib weekly or subcutaneously) to allow for a prolonged administration of this effective regimen.
Conflict-of-interest disclosure: The author has received honoraria from Millennium, Janssen (Germany), and Celgene (Germany). ■