Abstract
To increase (tumor) vaccine efficacy, there is an urgent need for phenotypic and functional characterization of human dendritic cell (DC) subsets residing in lymphoid tissues. In this study we identified and functionally tested 4 human conventional DC (cDC) subsets within skin-draining sentinel lymph nodes (SLNs) from early-stage melanoma patients. These SLNs were all tumor negative and were removed on average 44 days after excision of the primary melanoma. As such, they were considered representative of steady-state conditions. On comparison with skin-migrated cDC, 2 CD1a+ subsets were identified as most likely skin-derived CD11cint Langerhans cells (LC) with intracellular langerin and E-cadherin expression or as CD11chi dermal DCs with variable expression of langerin. Two other CD1a− LN-residing cDC subsets were characterized as CD14−BDCA3hiCD103− and CD14+BDCA3loCD103+, respectively. Whereas the CD1a+ skin-derived subsets displayed greater levels of phenotypic maturation, they were associated with lower levels of inflammatory cytokine release and were inferior in terms of allogeneic T-cell priming and IFNγ induction. Thus, despite their higher maturation state, skin-derived cDCs (and LCs in particular) proved inferior T-cell activators compared with the CD1a− cDC subsets residing in melanoma-draining LNs. These observations should be considered in the design of DC-targeting immunotherapies.
Introduction
Dendritic cells (DCs) are the most powerful APCs and play critical roles in keeping the balance between immune tolerance and activation. DCs are therefore also important for starting an efficient antitumor immune response and are seen as promising targeting candidates for tumor immunotherapy strategies.1,2 Current DC-based immunotherapies generally use ex vivo–generated autologous monocyte-derived or CD34+ hematopoietic precursor-derived DCs.2,3 Despite occasionally observed clinical benefits from DC-based vaccination, there is a large gap between the actual and expected efficacy of such trials on the basis of in vivo animal experiments.4 Many questions remain as to which DC type to use, how to stimulate them, or where best to administer the DCs to achieve vaccination with mature, migratory, and Th1-inducing DCs that provoke an efficient antitumor immune response.5-7
An ever-increasing insight in specialized functions of murine DC subsets is sadly mirrored by a lack of knowledge on how human DCs relate to mouse DCs and whether subsets that have been identified in mice have a (phenotypically different, but functionally equivalent) counterpart in humans.4,8-11 In particular the interrelationship between nonplasmacytoid, conventional DC (cDC) subsets has been obscure, in large part because of their plasticity and dynamic changes in their differentiation and maturation state, which is accompanied by shifts in associated phenotypic markers.12 In mice, extensive DC-subset analyses have been performed through the use of transgenic models, the ability to track and monitor cells in vivo, and the ability to remove specific organs, whereas in humans, especially for DC subsets present at low frequencies in lymphoid tissues such as lymph nodes (LNs; 0.1%-2%), this is more complicated.13-15 Because skin is generally regarded an attractive site for the delivery of vaccines, identification and characterization of DC subsets in skin-draining LN are particularly relevant. Although the authors of previous immunohistochemical studies have indicated the presence of both Langerhans cells (LCs) and dermal DCs (DDCs) in steady-state skin-draining LNs,14,15 until now it has proven technically unfeasible to perform more extensive flow cytometry–based phenotypic and functional cDC subset analyses.
We and others previously described a method to obtain viable cells from melanoma-draining sentinel lymph nodes (SLNs) without hindering routine diagnostic procedures.16,17 We have used this methodology to study the in vivo effects of immune modulators such as the CpG-B TLR9-ligand PF-3512676 and GM-CSF on DC and T-cell subsets in the SLN.18-21 In the context of 3 separate clinical phase 2 trials, we have collected a sizeable number of SLNs from untreated or saline placebo-administered melanoma patients, from which phenotypic DC data were obtained through multiparameter flow cytometric analysis and of which viable cells were cryopreserved for further functional analysis. From these, we have selected tumor-negative SLNs from Stage I-II melanoma patients, which were removed 1-2 months after excision of the primary melanoma, to perform an in-depth analysis of cDC subsets in steady-state skin-draining LNs. In 4 discernable cDC subsets we have studied the differential expression patterns of markers that have been linked to maturation, costimulation, and cross-presentation or tolerance-induction (ie, BDCA3/CD141, CD103, B7-H1/-H4) or that identify human skin-derived subsets (ie, CD1a, dendritic cell-specific intercellular adhesion molecule-3-grabbing non-integrin [DC-SIGN], E-cadherin, and langerin), and we performed comparative analyses with human skin-emigrated cDCs.
Our data indicate the presence of at least 2 skin-derived and 2 LN-resident cDC subsets with differential maturation states and functional T-cell priming abilities. In analogy to recent mouse data,14,22-25 Langerin+ cells, with lower Langerin expression levels than found in LC, were observed within the DDC subset derived from human skin and its putative equivalent from skin-draining LN, as well as BDCA3/CD141+ and CD103+ cDCs. These data represent the first functional characterization of human LN cDC subsets and supply new leads for the development of human DC-targeted immunotherapies.
Methods
Patient selection and isolation of viable LN cells
Human LN material was obtained with informed consent from stage I/II melanoma patients undergoing the SLN triple technique procedure16 at the VU University Medical Center, without interference with pathologic diagnostics and following hospital guide lines. The SLN were sampled in the context of 3 clinical phase 2 trials performed between 2002 and 2009, which were approved by the institutional review board of the VU University Medical Center. Patients included in the analyses presented here were either untreated or received intradermal injections of a saline placebo; 8 women and 6 men were included (mean age of 50 years; range, 29-76 years). All had tumor-negative SLN and an average Breslow thickness of 1.5 mm (range, 0.5-3.6 mm). All patients were provided with informed consent in accordance with the Declaration of Helsinki.
Before SLN removal, the primary tumors had been excised at a mean interval of 44 days (range, 12-94 days). Viable cells were isolated from the SLN by the use of a cytologic scraping method as previously described.16,17 In short, LN were bisected lengthwise with a surgical scalpel. From one half, 10 scrapes were made with a surgical blade (no. 22); we rinsed the blade after each scrape in a tube filled with 15 mL of 0.1% DNase and 0.14% collagenase A (Roche Nederland B.V.). The cell suspension was then transferred to a sterile flask in a total volume of 30 mL of DNase/collagenase, after which the suspension was incubated in a 37°C water bath on a magnetic stirrer for 45 minutes. The cell suspension was run through a 100-μm sterile cell strainer, and the flask and strainer were rinsed with 20 mL of IMDM (Lonza) with 10% FCS (Perbio). Cells were centrifuged at 490g rpm, 4°C for 5 minutes, washed with 10 mL of IMDM with 10% FCS, and taken up in 3 mL of IMDM with 10% FCS for viable cell count by trypan blue exclusion.
Skin explant culture and collection of skin-emigrated DCs
Human skin tissue was obtained after informed consent from patients undergoing corrective breast or abdominal plastic surgery at the VU University Medical Center or the Tergooi Hospital, following hospital guidelines. Biopsies of 6 mm in diameter were taken as described previously and cultured in IMDM supplemented with 5% human pooled serum (Sanquin).26 Cells were allowed to migrate from the biopsies for 48 hours, after which they were harvested and analyzed by flow cytometry.
Flow cytometric phenotyping
Human SLN single-cell suspensions were phenotypically analyzed by flow cytometry with the following mAbs diluted in PBS supplemented with 0.1% BSA and 0.02% NaN3 (FACS buffer) and incubated for 30 minutes at 4°C: IgG1-FITC/PE (1:25), CD11c-APC (1:10), CD14-PerCP_Cy5 (1:10), CD1a-PE (1:25), CD1a-FITC (1:10), PD-1L FITC (1:25), DC-SIGN PE (1:25), CD40-FITC (1:10), CD80-FITC (1:10), CD86-FITC (1:25; BD Biosciences), BDCA3-PE (1:10; Miltenyi Biotec), CD103-PE (1:25; Caltag Laboratories), E-cadherin PE (1:10), Langerin-PE (1:10), CD83-PE (1:10), CD83-FITC (1:10; Beckman Coulter Immunotech), and B7H4-FITC (1:10; AbD Serotec).
After incubation, cells were washed in FACS buffer to remove excess antibodies. Cells (0.25-0.5 × 106) were analyzed on a FACSCalibur flow cytometer (Becton Dickinson) equipped with CellQuest analysis software. Of note, inclusion of a lineage cocktail (consisting of anti-CD3, anti-CD19, ant-CD56, and anti-CD15) in a set of 3 SLN samples showed contaminating non-DC cells in each of the measured DC subsets to average 6.4% (range 0%-18%). For intracellular staining of langerin, E-cadherin and DC-SIGN, surface markers CD14, CD1a, and CD11c were first stained as described previously. Subsequently, cells were fixed and permeabilized with the BD Fix-Perm kit, following manufacturer's guidelines. Intracellular staining with PE-labeled DC-SIGN, langerin, or control IgG1 was performed for 30 minutes at 4°C in 1 × permeabilization buffer. Cells were washed once with 1 × permeabilization buffer and once with FACS buffer before analysis.
Flow-based cell sorting
cDC subsets were isolated by fluorescent cell sorting by the use of a FACS Aria (BD) and BD Diva software. Cells (10-30 × 106) were first stained with 5 μL of CD1a-PE, 10 μL of CD14-PerCP-Cy5, and 10 μL of CD11c-APC in sterile PBS for 30 minutes at 4°C. After staining, the cells were washed and taken up in IMDM, supplemented with 10% FCS (HyClone), 100 IU/mL sodium penicillin (Yamanouchi Pharma), 100 μg/mL streptomycin (Radiumfarma-Fisopharma), and 2.0mM l-glutamine (Invitrogen) and were filtered over a cell filter (Miltenyi Biotec) to remove clumps that could clog the system. The 4 cDC subsets were sorted over 4 streams at a time, based on the expression of the 3 surface markers. After sorting, cells were washed and were used for functional assays.
Mixed leukocyte reaction
Peripheral blood leukocyte (PBL) proliferation induced by sorted LN cDC subsets was assessed by mixed leukocyte reaction (MLR) with a CFSE-based proliferation readout.27 Allogeneic donor PBLs were labeled with 1μM CFSE in PBS supplemented with 5% FCS for 7 minutes at 37°C (in a water bath). Cells were washed 3 times with PBS/5% FCS and once with IMDM + 10% human pooled serum, penicillin, streptomycin, and glutamine. PBL (10 000-30 000; 1 × 106 cells/mL) were stimulated with 1000-3000 LN-cDC (0.1 × 106 cells/mL; 10:1 ratio responder/stimulator cells). PBL proliferation, measured by CFSE dilution, was analyzed by flow cytometry on day 7. Before harvesting, culture supernatants were collected for T-cell cytokine analysis (see “Cytokine analysis”).
Imprint specimens and cytospins
Imprints were made from the SLN cutting surface that was not scraped and immunocytochemically analyzed. The imprints and cytospins were air-dried overnight, fixed in acetone for 10 minutes, and stained by the use of a biotin-streptavidin staining technique as described previously.28 CD1a, BDCA3/CD141 (Miltenyi Biotec), CD14 (Novocastra), DC-SIGN (BD), and CD3 mAbs (Dakopatts) were used at dilutions of 1:10. Cytospins were made of the FACS-sorted cDC subsets and subsequently stained according to May Grünwald-Giemsa.28 At room temperature, with air as medium, expression was analyzed by the use of a Leica DMR microscope (Leica) with 40×/0.75 HCX PL Fluotar and 10×/0.30 and 20×/0.50 HC PL Fluotar objectives (Leica). Images were captured with a Leica DC200 digital camera (Leica Microsystems) and Leica DC Viewer (Leica Microsystems).
Cytokine analysis
Freshly isolated SLN cells were cultured overnight at 37°C (1×/105 per 100 μL) in IMDM with 10% FCS. The supernatants were harvested and stored at −20°C until analysis. For ex vivo T-cell cytokine detection, freshly isolated SLN cells were incubated for 1 hour on ice with 2 μg of anti-CD3 and 0.4 μg of anti-CD28 per 106 cells (kindly provided by Dr René van Lier) in 100-200 μL of IMDM with 5% FCS. After incubation and washing, cells were placed in 24-well tissue culture plates (Greiner Bio-One), which were previously coated with affinity-purified goat antimouse immunoglobulin (1:100 in PBS; DAKO), in complete medium with 10% FCS at a concentration of 106/mL/well for 1 hour at 4°C. Subsequently, the plates were transferred to a humidified incubator and cultured overnight at 37°C, after which the culture supernatants were harvested and stored at −20°C until analysis. Supernatants were analyzed using the inflammatory cytokine bead array (CBA) kit or the Th1/Th2 CBA kit (both from BD Biosciences) for the simultaneous flow cytometric detection of IL-8, IL-1β, IL-6, IL-10, TNF-α, and IL-12p70, or IL-2, IL-4, IL-5, IL-10, TNF-α, and IFN-γ, respectively, following the manufacturer's instructions and with the use of CBA analysis software (BD Biosciences).
Statistical Analyses
Differences between DC subsets were analyzed by use of the one-way analysis of variance test. The post hoc multiple comparison Tukey test was used to analyze differences between 2 DC subsets. The 2-sided paired Student t test was used for comparisons between 2 samples. Correlations were determined by use of the Pearson r test. Differences were considered significant when P < .05.
Results
Definition of 4 human cDC subsets in LN
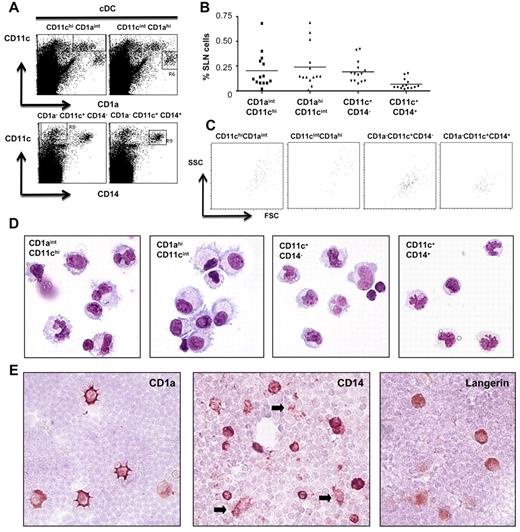
Because cDC subsets from human skin have previously been characterized by differential expression of CD1a, CD11c, and CD14,28,29 we set out to identify their migrated equivalents by expression analysis of these markers in SLN suspensions. We identified 4 cDC subsets (Figure 1A): 2 distinct CD1a+ populations with different expression levels of CD11c and CD1a (CD1aintCD11chi and CD1ahiCD11cint) and 2 distinct CD1a− populations with differential CD14 expression, gated out by high CD11c expression levels (CD11c+CD14− and CD11c+CD14+). Of note, CD1a and CD14 expression in these populations was mutually exclusive. Figure 1B shows the frequencies of the 4 cDC subsets as percentages of total leukocytes within the SLN single-cell suspensions (n = 14) and indicates the CD14+ subset to be relatively rare under steady-state conditions. The CD1a+ subsets had greater forward and side scatter properties (Figure 1C), suggestive of a larger and more DC-like morphology.
Identification of 4 cDC subsets in human SLN. (A) Flow cytometric dot plots for CD11c, CD1a, and CD14: gating of 4 different cDC subsets in human SLN, ie, 2 CD1a+ subsets, CD11chi CD1aint and CD11cint CD1ahi (top) and 2 CD1a− subsets, CD1a− CD11c+ CD14− and CD1a+ CD11c− CD14+ (gated to exclude CD1a+ cells). (B) Frequencies of the 4 cDC subsets within SLN single-cell suspensions (n = 14). (C) Forward scatter (FSC) and side scatter (SSC) plots for the 4 cDC subsets, gated on CD11chi CD1aint, CD11cint CD1ahi, CD1a− CD11c+ CD14−, and CD1a− CD11c+ CD14+ and back-gated onto forward/side scatter. (D) Morphologic characterization (cytochemical May-Grünwald-Giemsa staining) of sorted CD11chiCD1aint, CD11cintCD1ahi, CD1a−CD11c+CD14−, and CD1a−CD11c+CD14+ cells, isolated (FACS-sorted) from human SLN. (E) Immunocytochemical staining for CD1a, CD14, and langerin cells on SLN imprints, arrows indicate CD14+ cell protrusions (magnification 400×).
Identification of 4 cDC subsets in human SLN. (A) Flow cytometric dot plots for CD11c, CD1a, and CD14: gating of 4 different cDC subsets in human SLN, ie, 2 CD1a+ subsets, CD11chi CD1aint and CD11cint CD1ahi (top) and 2 CD1a− subsets, CD1a− CD11c+ CD14− and CD1a+ CD11c− CD14+ (gated to exclude CD1a+ cells). (B) Frequencies of the 4 cDC subsets within SLN single-cell suspensions (n = 14). (C) Forward scatter (FSC) and side scatter (SSC) plots for the 4 cDC subsets, gated on CD11chi CD1aint, CD11cint CD1ahi, CD1a− CD11c+ CD14−, and CD1a− CD11c+ CD14+ and back-gated onto forward/side scatter. (D) Morphologic characterization (cytochemical May-Grünwald-Giemsa staining) of sorted CD11chiCD1aint, CD11cintCD1ahi, CD1a−CD11c+CD14−, and CD1a−CD11c+CD14+ cells, isolated (FACS-sorted) from human SLN. (E) Immunocytochemical staining for CD1a, CD14, and langerin cells on SLN imprints, arrows indicate CD14+ cell protrusions (magnification 400×).
This finding was confirmed by cytochemical analysis of the FACS-sorted subsets (Figure 1D) as well as by imprint cytology of the SLN, which also revealed a paracortical localization of the CD1a+ cDC (Figure 1E). Like CD1a, langerin has been associated with skin-derived cDC subsets, and we found it expressed on large cells scattered throughout the paracortical T-cell areas (Figure 1E). The CD14+ subset had a smaller, monocyte-like appearance (Figure 1D) and was often localized around vessel-like structures (see Figure 1E right). Nevertheless, CD14+ protrusions that extended between lymphocytes, suggestive of a DC-like appearance, were clearly discernable in situ (Figure 1E arrows).
Flowcytometric identification of langerin+ dermal DCs and LCs in human LN
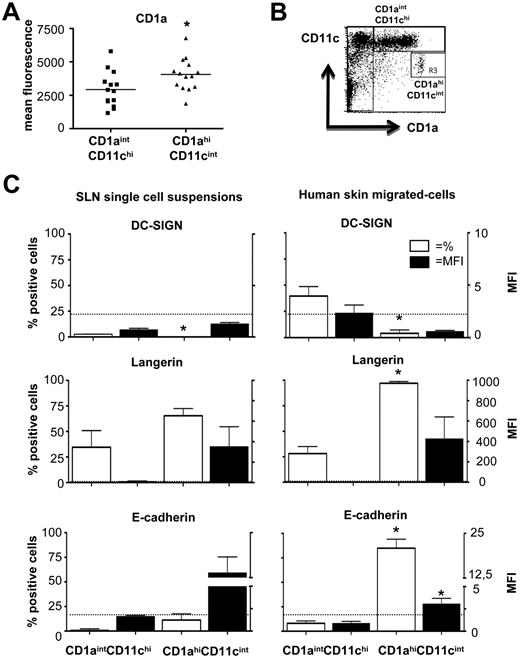
Because in human skin, langerin+ LCs are typified by high CD1a expression levels, we hypothesized that the CD1ahiCD11cint LN subset might represent skin-emigrated LC and that the CD1aintCD11chi subset might be migrated DDCs with reported lower levels of CD1a (Figure 2A).29 Indeed, FACS analysis of human skin explant-emigrated DCs clearly showed CD1ahiCD11cint and CD1aintCD11chi populations (Figure 2B) reminiscent of the populations found in SLN (Figure 1A). No surface expression of either of the C-type lectins langerin or DC-SIGN was detected on the CD1a+ LN-DC subsets (data not shown), which would have facilitated easy discrimination between LC and DDC. However, on intracellular staining for these markers, expression was detectable, and there were clear differences between the 2 CD1a+ cDC subsets (see Figure 2C: expression in percentages [open bars, left-hand y-axis] or in median fluorescence intensity [MFI, closed bars, right-hand y-axis]).
Identification of skin-migrated DDCs and LCs in human SLN. (A) Average mean fluorescence intensity (MFI) values for CD1a expression levels on CD11chiCD1aint and CD11cintCD1ahi SLN cDC (n = 14) (B) Gating strategy for CD11chiCD1aint and CD11cintCD1ahi DCs, migrated from human skin explants (data from one representative experiment of 4 is shown). (C) Percentages positive cells (of SLN leukocytes, open bars: left y-axis) and the median fluorescence intensities (MFI, closed bars: right y-axis) for intracellular DC-SIGN, langerin, and E-cadherin on CD11chiCD1aint and CD11cintCD1ahi cDC in SLN single-cell suspensions (left, n = 3) and skin-migrated cells (right, n = 4). Bars represent the mean ± SEM; dotted line indicates MFI = 2; *P < .05 in paired 2-sided Student t test.
Identification of skin-migrated DDCs and LCs in human SLN. (A) Average mean fluorescence intensity (MFI) values for CD1a expression levels on CD11chiCD1aint and CD11cintCD1ahi SLN cDC (n = 14) (B) Gating strategy for CD11chiCD1aint and CD11cintCD1ahi DCs, migrated from human skin explants (data from one representative experiment of 4 is shown). (C) Percentages positive cells (of SLN leukocytes, open bars: left y-axis) and the median fluorescence intensities (MFI, closed bars: right y-axis) for intracellular DC-SIGN, langerin, and E-cadherin on CD11chiCD1aint and CD11cintCD1ahi cDC in SLN single-cell suspensions (left, n = 3) and skin-migrated cells (right, n = 4). Bars represent the mean ± SEM; dotted line indicates MFI = 2; *P < .05 in paired 2-sided Student t test.
By making direct comparisons with DCs migrated from ex vivo healthy donor skin explants,28 we were able to draw clear phenotypic parallels between the CD1a+ LN-DC subsets and skin-emigrated LCs and DDCs. Whereas DC-SIGN expression was generally low, it was significantly lower (percentage-wise) in the CD1ahiCD11cint cDCs, which also expressed intracellular langerin at high levels. In conjunction with their exclusive expression of E-cadherin, these features clearly revealed these CD1ahiCD11cint cDCs to be epidermis-derived LCs (Figure 2C). Interestingly, heterogeneous expression of intracellular langerin was observed in the CD1aintCD11chi cells (and at much lower intensity levels than in the LC), suggesting the presence of migrated human langerin+ DDCs, previously identified in mouse studies.23,25,30,31 Remarkably consistent expression patterns were observed between the SLN-derived and skin-emigrated subsets, with the exception of lower expression levels of DC-SIGN in the SLN-derived CD1aintCD11chi DDCs, suggesting its down-regulation on migration and accompanying maturation. Of note, although neither of the CD1a− LN-cDC subsets expressed langerin, heterogeneous DC-SIGN expression was also observed in the CD14+ subset (data not shown).
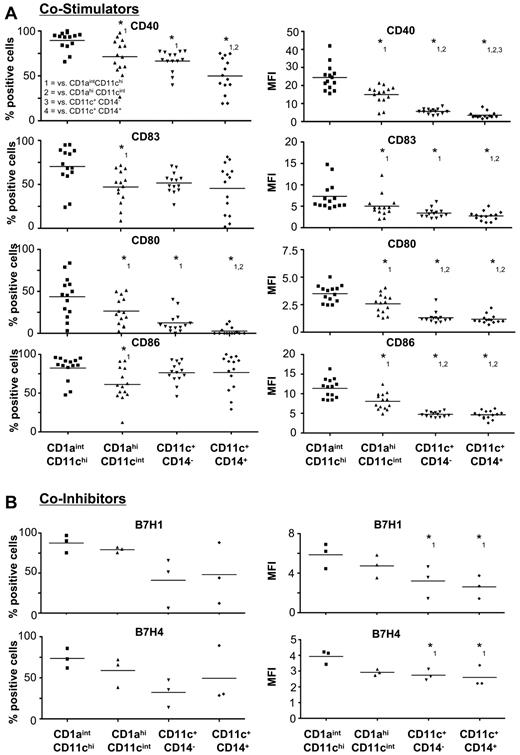
Expression of costimulatory and coinhibitory receptors on human LN-cDCs
By using 4-color flow cytometry, we compared CD1aintCD11chi DDC, CD1ahiCD11cint LC, and the CD1a−CD11c+CD14− or CD1a−CD11c+CD14+ cDC subsets for the expression of various costimulatory (Figure 3A) and coinhibitory (Figure 3B) receptors at their cell surface. Both CD1a− cDC subsets displayed a relatively immature phenotype as reflected by low percentages and low expression levels of the various activation markers and costimulatory molecules, such as CD40, CD83, CD80, and CD86. In contrast, the CD1a+ skin-derived cDC subsets expressed significantly greater intensity levels of all the tested costimulatory molecules, with the CD1a+CD11chi DDC-like subset displaying the most mature phenotype, clearly demonstrated by its superior expression levels of CD40, CD80, and CD83 (Figure 3A). In accordance with their mature state, in addition most CD1a+ cDCs expressed the coinhibitory molecules B7H1 and B7H4. In contrast, generally less than half of the CD1a−CD11c+ cDC expressed these surface markers and at lower-intensity levels compared with the CD1a+ LN-DC (Figure 3B).
Activation status of human SLN cDC subsets. Percentages (left) and the MFIs (right) of (A) costimulatory (CD40, CD83, CD80, CD86) (n = 14) and (B) coinhibitory (B7H1 and B7H4) (n = 3) surface receptors. *P < .05 in 1-way ANOVA with post hoc multiple comparison Tukey test. Numbers indicate the significant difference compared with the (1) CD11chi CD1aint, (2) CD11cint CD1ahi, (3) CD11c+CD1a−CD14−, and (4) CD11c+CD1a−CD14+ subsets.
Activation status of human SLN cDC subsets. Percentages (left) and the MFIs (right) of (A) costimulatory (CD40, CD83, CD80, CD86) (n = 14) and (B) coinhibitory (B7H1 and B7H4) (n = 3) surface receptors. *P < .05 in 1-way ANOVA with post hoc multiple comparison Tukey test. Numbers indicate the significant difference compared with the (1) CD11chi CD1aint, (2) CD11cint CD1ahi, (3) CD11c+CD1a−CD14−, and (4) CD11c+CD1a−CD14+ subsets.
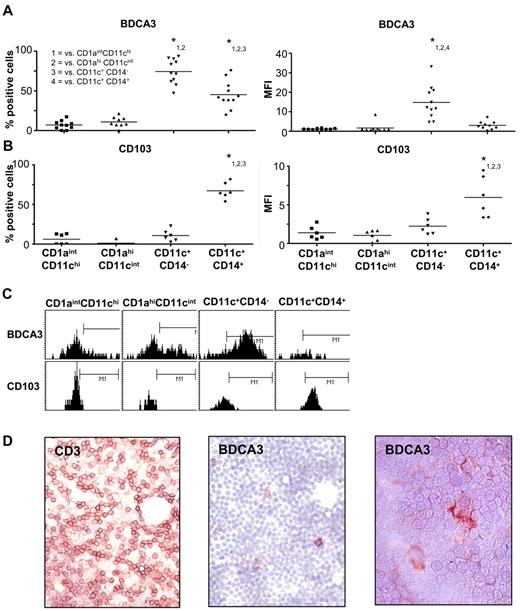
Identification of BDCA3/CD141- and CD103-expressing cDC subsets
Recently, human BDCA3/CD141+ cDCs in peripheral blood were identified as cross-presenting DCs that most closely resembled the much-studied splenic murine CD8α+ cDC subset, established as mainly responsible for in vivo cross-presentation.9-11 Similarly, CD103 is also expressed on cDC subsets that were associated with cross-presentation.32,33 In the SLN, both CD1a− cDC subsets were found to express BDCA3 (Figure 4A). Although high percentages of BDCA3-expressing cells were detected both in the CD14− and CD14+ subsets, expression levels were much greater on the CD11c+CD14− subset (Figure 4A,C). A small percentage of the CD1a+CD11cint LC subset also expressed low levels of BDCA3 (Figure 4A,C). In mice, CD103 expression has been associated with a small subset of langerin+ DDCs that patrol the dermis in the steady state and can migrate to skin-draining LNs.22 In contrast, in human skin-draining SLN CD103 was almost exclusively expressed on the CD11c+CD14+ cDC subset (Figure 4B-C). Although paracortical CD14 staining shed light on the morphology of the CD14+CD103+ subset (Figure 1E), we used the high BDCA3 levels that characterize the CD1a−CD14− cDC subset to study its localization and morphology in LN. Immunocytochemical analysis of SLN imprints showed these cells to be located in the paracortical T-cell areas of the LN and to display a classic DC morphology (Figure 4D). Indeed, high-magnification microscopy revealed long BDCA3+ protrusions interdigitating between the lymphocytes (Figure 4D right).
Expression of BDCA3 and CD103 on SLN cDC subsets. Percentages positive cells (left) and MFI levels (right) of (A) BDCA3/CD141 (n = 11) and (B) CD103 (n = 6) surface expression on the 4 cDC subsets identified in human SLNs. *P < .05 in 1-way ANOVA with post hoc multiple comparison Tukey test. Numbers indicate the significant difference compared with (1) CD11chiCD1aint, (2) CD11cintCD1ahi, (3) CD11c+CD1a−CD14−, and (4) CD11c+CD1a−CD14+ subsets. (C) Histogram plots of one representative experiment showing expression levels of BDCA3/CD141 (top) and CD103 (bottom) on SLN cDC subsets. The markers were placed based on respective isotype control staining. (D) Characterization of the localization and morphology of BDCA3/CD141+ cells within SLN imprint samples. Shown is a CD3 staining to identify the paracortical T-cell areas (left, magnification ×400) as well as BDCA3 staining in 2 magnifications (middle, ×400 and right, ×630).
Expression of BDCA3 and CD103 on SLN cDC subsets. Percentages positive cells (left) and MFI levels (right) of (A) BDCA3/CD141 (n = 11) and (B) CD103 (n = 6) surface expression on the 4 cDC subsets identified in human SLNs. *P < .05 in 1-way ANOVA with post hoc multiple comparison Tukey test. Numbers indicate the significant difference compared with (1) CD11chiCD1aint, (2) CD11cintCD1ahi, (3) CD11c+CD1a−CD14−, and (4) CD11c+CD1a−CD14+ subsets. (C) Histogram plots of one representative experiment showing expression levels of BDCA3/CD141 (top) and CD103 (bottom) on SLN cDC subsets. The markers were placed based on respective isotype control staining. (D) Characterization of the localization and morphology of BDCA3/CD141+ cells within SLN imprint samples. Shown is a CD3 staining to identify the paracortical T-cell areas (left, magnification ×400) as well as BDCA3 staining in 2 magnifications (middle, ×400 and right, ×630).
T-cell stimulatory capacity of LN cDC subsets
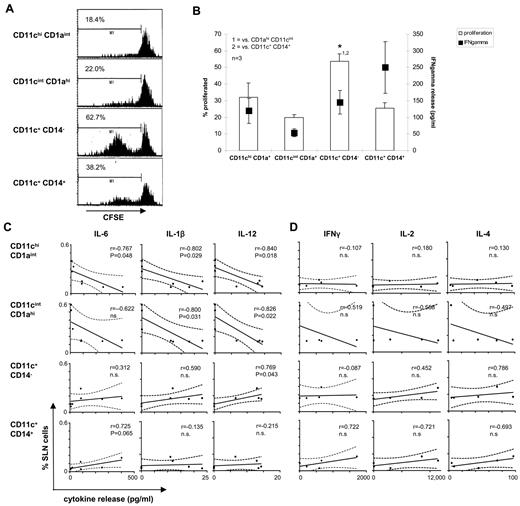
To study their T-cell stimulatory capacity, we cocultered isolated SLN cDC subsets from 3 donors with CFSE-labeled allogeneic PBL in independent experiments. Surprisingly, in view of its relatively immature phenotype (Figure 2A), the CD1a−CD11c+CD14− cDC subset turned out to be the most powerful inducer of T-cell proliferation (Figures 5A-B). However, in seeming contrast with their mature phenotype, the CD1a+ cDC subsets, and the CD1ahiCD11cint LC in particular, were poor inducers of T-cell alloreactivity (Figure 5A-B). Of the T-cell cytokines measured in supernatants of the MLR cultures, only IFNγ was consistently detected. As shown in Figure 5B, high levels of IFNγ were induced in particular by the CD1a−CD11c+CD14+ subset, whereas the CD1ahiCD11cint LC proved poor stimulators in this respect.
T-cell stimulatory ability of the CD1a− and CD1a+ SLN cDC subsets. T-cell stimulatory abilities of human SLN cDC subsets were analyzed by allogeneic MLR with CFSE-labeled human T cells. Data from one representative experiment of 3 performed are shown in panels A and in B the average percentage of proliferated cells (n = 3, left y-axis) combined with IFNγ present in day 7 MLR supernatants (right y-axis) are shown. Correlations between the frequencies of SLN cDC subsets and (C) IL-6, IL-1β, and IL-12p70 present in 24-hour unstimulated cultures of SLN single-cell suspensions (n = 7) or (D) IFNγ, IL-2, and IL-4 in 24-hour supernatants of SLN T cells stimulated by anti-CD3 and anti-CD28 (n = 5). Correlations were determined by use of the Pearson r test. Differences were considered significant when P < .05.
T-cell stimulatory ability of the CD1a− and CD1a+ SLN cDC subsets. T-cell stimulatory abilities of human SLN cDC subsets were analyzed by allogeneic MLR with CFSE-labeled human T cells. Data from one representative experiment of 3 performed are shown in panels A and in B the average percentage of proliferated cells (n = 3, left y-axis) combined with IFNγ present in day 7 MLR supernatants (right y-axis) are shown. Correlations between the frequencies of SLN cDC subsets and (C) IL-6, IL-1β, and IL-12p70 present in 24-hour unstimulated cultures of SLN single-cell suspensions (n = 7) or (D) IFNγ, IL-2, and IL-4 in 24-hour supernatants of SLN T cells stimulated by anti-CD3 and anti-CD28 (n = 5). Correlations were determined by use of the Pearson r test. Differences were considered significant when P < .05.
To further assess the association of the 4 cDC subsets with a microenvironment conducive to T-cell activation, available data were analyzed to determine their relative frequencies in SLN single-cell suspensions in relation to spontaneous ex vivo release levels of inflammatory cytokines as well as to anti-CD3/anti-CD28–induced release of T-cell cytokines. Consistently negative correlations with the release of inflammatory cytokines (IL-6, IL-1β, and IL-12p70) were observed for both of the CD1a+ skin-derived subsets, whereas positive correlations (at various levels of significance) were found for the CD1a−CD11c+ LN-resident subsets (Figure 5C). Accordingly, T-cell cytokine release levels correlated with CD1a− subset content rather than with CD1a+ subset frequencies, although not significantly so because of the low numbers of available data (shown for IFNγ, IL-2, and IL-4 in Figure 5D).
Discussion
The lack of knowledge on phenotype and function of human cDC subsets in skin-draining LNs has proven a major hurdle in translating preclinical DC-based therapies in mice into successful DC-based therapies for humans.4,8 The data provided in this manuscript are a first step toward a more detailed discrimination of different human LN-cDC subsets, both in terms of phenotype and of function. This information could provide new insights leading to improved immunotherapeutic strategies. In particular the identification of LN-cDC subsets, which are primarily tolerogenic and thereby disadvantageous for antitumor immunity, and the exploration of ways in which to break this tolerance, are of prime importance in this regard. However, establishing which DC subsets are the most potent in inducing antitumor immunity and studying ways to promote their functions may push the envelope for future immune-enhancing therapies.
The skin is commonly regarded as an attractive gateway for the delivery of (tumor) vaccines. A dense network of DC and lymphatic vessels facilitates antigen capture and subsequent transport to the draining LN. In mice, different cDC subsets in skin have been described in detail, delineating their origins and specialized functions. LCs in the steady state are derived from precursor cells residing in the skin, whereas under inflammatory conditions they can also develop from monocytes originating from the blood.14,34 There is evidence to suggest that on their activation and migration to LN, LC preferentially bind and activate T cells.35 Recently, langerin+ and CD103+ DDCs were identified in murine studies as a major migratory DDC subset with the ability to cross-present proteins from the skin environment.22,33,36 It has been suggested that CD1a+ DDCs may be the human equivalent of this subset,35 but evidence to back up this claim has been lacking.
Beside these skin-migrated cDC subsets, murine skin-draining LNs also harbor resident subsets, most notably the CD8α+ subset with a superior CD8+ T-cell activating capacity and the ability to cross-present antigens.13,14 Clearly, to optimize the efficacy of cutaneously applied vaccines in humans, it is of the utmost importance to positively identify functional equivalents of these DC subsets in human skin and LN. To establish a baseline, it is vital to study these subsets in steady state tissues, which, in the case of skin-draining LN, is near-impossible. We therefore used SLN that drained early-stage melanomas. We believe that single-cell suspensions from tumor-negative SLN of which the primary tumor has been removed more than a month before provide a valid model resembling the steady state. Nevertheless, interpretation of the obtained results warrants caution, as some lingering tumor influences cannot be excluded.
On the basis of 4-color flow cytometry and by making head-to-head comparisons with skin-emigrated DCs, we discerned and characterized 4 human cDC subsets in skin-draining LN, ie, the skin-derived CD1ahiCD11cint LC- and CD1aintCD11chi DDC-like subsets, and the CD1a− LN-resident CD11c+CD14− and CD11c+CD14+ subsets.
Although, for obvious reasons, it was impossible to demonstrate a direct physical link between the human CD1a+ skin-emigrated and LN-residing DCs (as demonstrated by, eg, FITC painting in mice), the clear phenotypic parallels nevertheless strongly supported the identity of CD1ahiCD11cint and CD1aintCD11chi as skin-derived LC and DDC, respectively. Despite their more activated phenotype, the CD1a+ skin-derived subsets proved not to be very efficient in inducing T-cell proliferation in an allogeneic MLR. This might in part be because of their relatively high surface expression levels of the coinhibitory molecules B7H1 and B7H4. Although this may be a common feature of steady-state skin-migrated cDC in LN, it cannot be excluded that it might also be a residual tumor-induced suppressive effect.37 The observed mature phenotype of in particular the CD1a+ DDC subsets is in keeping with our previous observation of a correlation and contiguous relationship between migrating CD1a+CD83+ DDC and mature CD1a+ DC in SLNs.38 Interestingly, the observation of consistently negative correlations between the CD1a+ DDC and LC frequencies in the SLN and ex vivo inflammatory cytokine release (Figure 5D) suggests that these subsets may be actively tolerogenic in the steady state despite their mature status. This may either be because of their B7H1/-H4 expression or expression of indoleamine 2,3-dioxygenase, which has previously been associated with T-cell suppression by activated LCs.39 Nevertheless, on intradermal delivery of GM-CSF, the maturation state and frequencies of CD1a+ DC in the SLNs were up-regulated and correlated significantly with melanoma-specific CD8+ effector T cells, indicative of the validity of activational targeting of these LN-cDC subsets for tumor vaccination.21 These observations reflect seemingly contradictory reports on the tolerizing or T-cell stimulatory function of LC in mice.14
Whereas in mice langerin+ DDC with cross-presenting and T-cell activating abilities have been identified22,24,30 and have extensively been studied in elegant transgenic mouse models,14,25,31,40,41 no direct proof has been published demonstrating these cells to be present in human dermis or human LNs. Their existence has nevertheless been implied.41 Our data, which uses intracellular staining of langerin in both human skin explant-migrated DDC and their CD1aintCD11chi LN equivalents, clearly demonstrated the presence of langerin-expressing cells within this subset, providing the first proof that also in human tissues langerin+ DDCs can be distinguished. Further comparative phenotypic and functional studies between langerin− and langerin+ human DDCs are now underway.
Although CD14+ DCs were previously identified among skin-emigrated DC by us and by others,28,29,42,43 these differed from the CD14+ cDCs detected in the SLN suspensions in that they lacked expression of CD83 and displayed morphologic features more reminiscent of macrophages.28 In addition, CD1a−CD14−CD11c+ DCs that had migrated from human skin explants lacked the high levels of BDCA3 that we observed on the CD1a−CD14−CD11c+ cDC subset in the SLN suspensions.28 Thus, in contrast to the CD1a+ subsets, the CD1a− subsets did not appear to have analogues among the skin-emigrated DC. Rather than deriving from skin, we propose these CD1a− LN-resident subsets to originate from precursors in the blood. It could be envisioned that they might be mobilized and rapidly activated under inflammatory conditions. This would be in line with their superior allogeneic T-cell priming and cytokine release properties and the observed correlation between their frequencies and ex vivo proinflammatory, T-cell–activating cytokine profiles (Figure 5).
DC-mediated cross-presentation of tumor-derived antigens to CD8+ T cells is vital for the elicitation of an effective antitumor immune response. In murine spleens CD8α-expressing DCs have been pinpointed as mainly responsible for cross-presenting exogenous antigens on MHC class I and for effective CTL priming.36,37,44,45 Interestingly, a genome-wide transcriptional profiling study suggested BDCA3+ DC in LNs to be the human equivalent of this CD8α+ DC subset.46 Recently, 3 groups independently confirmed this observation and reported BDCA3+ cDCs in human blood to most closely resemble the murine CD8α+ subset, both in phenotype and in cross-presenting ability.9-11
In reaction to this, others have compared mammalian DC subsets with cross-priming abilities for their relatedness and found that mouse CD8α+, sheep CD26+, and human blood-derived BDCA3+ DCs all expressed signal regulatory protein-α, cell adhesion molecule 1, the C-type lectin domain family 9, member A, chemokine receptor 1, and CD205.47,48 BDCA3+ cells have previously been detected in melanoma SLN.49 Our data now show that specifically both CD1a− cDC subsets as well as a small subpopulation within the CD1ahiCD11cint LC-like compartment express BDCA3. In addition, the CD11c+CD14+ cells were shown to express CD103, another marker previously linked to antigen cross-presentation in mice, although, remarkably, in that case by LN-migrating DDC rather than by blood-mobilized DCs.33 Additional polychromatic flow cytometric and functional analyses will have to reveal the exact (co)expression profiles of BDCA3; CD103; C-type lectin domain family 9, member A; chemokine receptor 1; signal regulatory protein; cell adhesion molecule 1; and/or CD205 and how these profiles may define specific LN-cDC subsets with demonstrable cross-presenting ability. Cross-presentation may result in either T-cell activation or tolerization, depending on input from the microenvironment, and may independently differ per defined cDC subset.32,50 In this regard, extensive C-type lectin and Toll-like receptor expression profiling of the discerned cDC subsets is of the utmost importance.
In summary, whereas the CD1a+ LC- and DDC-like subsets derived from human skin-draining LN displayed greater phenotypic maturation, the LN-resident BDCA3/CD141+ subsets were more potent in terms of allogeneic T-cell priming and cytokine release. The SLN-derived LC subset in particular proved a poor inducer of allogeneic T-cell proliferation and cytokine release. These data reflect earlier findings from in vivo murine studies and reveal phenotypic and functional heterogeneity among cDC subsets in skin-draining LN, which should be taken into account in the design of cutaneously applied (tumor) vaccines.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 USC section 1734.
Acknowledgments
The authors thank all the patients who provided their informed consent for the use of the clinical material for scientific research.
This work was supported by the Netherlands Organization for Scientific Research, NWO VIDI grant 917-56-32 to T.D.d.G., Stichting Cancer Center Amsterdam (CCA), and contains the work that resulted in a Dutch Cancer Society (KWF BUIT-4346) fellowship to R.v.d.V.
Authorship
Contribution: R.v.d.V. performed research, analyzed and interpreted data, and drafted and cowrote the manuscript; M.F.C.M.v.d.H. performed research and analyzed and interpreted data; J.J.L., B.J.R.S., and S.M.L. performed research and analyzed data; P.A.M.v.L., S.M., and M.P.v.d.T. treated patients and supplied the clinical research material; R.J.S. drafted the manuscript; and T.D.d.G. designed the research, interpreted data, and drafted and cowrote the manuscript.
Conflict-of-interest disclosure: The authors declare no competing financial interests.
Correspondence: Dr Tanja D. de Gruijl, Division of Immunotherapy, Department of Medical Oncology, VU University Medical Center, De Boelelaan 1117-CCA 2.44, 1081 HV Amsterdam, The Netherlands; e-mail: TD.deGruijl@Vumc.nl.
References
Author notes
R.v.d.V and M.F.C.M.v.d.H contributed equally to this paper.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal