Abstract
Serine protease inhibitors, termed serpins, are key regulators in many biologic events. Protease nexin-1 (PN-1) is a serpin that is barely detectable in plasma but found in many organs and produced by most cell types, including monocytes, platelets, and vascular cells. It has a large inhibition spectrum because it is the most efficient tissue inhibitor of thrombin but also a powerful inhibitor of plasminogen activators and plasmin. It has a high affinity for glycosaminoglycans, such as heparan sulfates, which potentiate its activity toward thrombin and target it to the pericellular space. PN-1 has been previously largely described as a crucial regulator of the proteolytic activity in nerves and of central and peripheral nervous system function. In contrast, little was known about its involvement in hemostasis and vascular biology. This article reviews recent data underlining its emerging role as a key factor in the responses of vessels to injury. Indeed, studies of PN-1–deficient mice have established important antithrombotic and antifibrinolytic properties of this serpin that have heretofore gone unrecognized. The roles of PN-1 in the areas of hemostasis and thrombosis summarized here provide insights that may allow the development of drugs and treatment strategies to prevent or limit thrombotic disorders.
Introduction
Serine proteases play a predominant role in the homeostasis of the cardiovascular system, including coagulation, fibrinolysis, and tissue remodeling. In blood, they circulate as inactive proforms or zymogens, and once activated, are quickly and irreversibly inhibited by circulating inhibitors, in particular by serine protease inhibitors, termed serpins. In contrast, at the tissue level, it is still not clear how endogenous inhibitors control the activity of the different proteases. In the context of vascular biology, both the thrombus, which can be considered as a neo-tissue, and the arterial wall are good examples of the importance of the regulation of serine protease activity by serpins.
Serpins form a large family of structurally related proteins present in the plasma and/or in tissues. Some of them are mainly synthesized by the liver and directly secreted into the bloodstream. Others are synthesized by peripheral cells, including circulating cells, mesenchymal stromal cells of the vascular wall, and cardiac myocytes. Although not all serpins are protease inhibitors,1 many of the members of this large superfamily act by interacting with the active site of the target proteases via the reactive site, which is positioned on an exposed loop. The protease trapped in the complex is then irreversibly inhibited. Serpins are direct or indirect key regulators of numerous cell and tissue responses to changes in environmental conditions.1 Via their molecular flexibility and their antiprotease activity, serpins play a key role in the modulation of cell adhesion, migration, proliferation, metabolism, and death. They are also involved in the prevention of proteolytic degradation of the extracellular matrix and of fibrin formation and lysis.2
One of the better-known and most studied members of the serpin superfamily is serpinC1,or antithrombin (AT), which circulates in the bloodstream and is the principal inhibitor of blood coagulation proteases. Moreover, particular emphasis has been placed on serpinE1 or plasminogen activator inhibitor-1 (PAI-1), an inhibitor of tissue plasminogen activator (tPA) and urokinase plasminogen activator (uPA), which are synthesized by numerous circulating and stromal cells in the cardiovascular system3 and whose concentration in the circulation was found to be a biomarker of cardiovascular risk.4
In many studies in animals and humans, investigators have demonstrated that, besides its role in the fibrinolytic system, PAI-1 plays a role in many human vascular disorders, including atherosclerosis and restenosis after balloon angioplasty.5 More recent investigations have revealed that another serpin, serpinE2, also known as protease nexin-1 (PN-1), the phylogenetically closest relative of PAI-1, is produced by most cell types, found in many organs, and has major pleiotropic functions. Until recently, only a few data were available concerning the role of PN-1 in the vascular system. Now, PN-1 appears to be a potential key factor in the regulation of thrombin and/or fibrinolytic enzyme activities in both the intra- and extravascular space compartments. This review will detail the functions of PN-1 related to hemostasis, thrombosis, and vascular biology that have emerged in the last decade.
Biochemistry of PN-1
PN-1 is a 45- to 50-kDa glycoprotein that is encoded by the SERPINE2 gene on human chromosome 2q99-q35.6 PN-1 is a 378 amino acid residue single-chain containing 3 cysteine residues that do not form disulfide bonds within the protein core of the molecule.7 The other members of the serpin superfamily, AT and PAI-1, share 30% and 41%, respectively, of PN-1 sequence.6,8 The protease recognition region (reactive center loop) of PN-1 is located near the carboxy-terminal end of the serpin domain. Two isoforms of human PN-1, named α- and βPN-1, have been identified, but their respective roles are still unknown. These forms only differ by the insertion of 3 nucleotides into the coding sequence and arise from alternative splicing.8
The tridimensional structure of PN-1 has not yet been reported, although it has been recently determined; the serpin is likely to exhibit the typical suicide substrate mechanism of action that is shared by the other superfamily members.9 Once the target serine protease binds to the substrate sequence of the serpin and cleaves the reactive site (P1-P′1), Arg364-Ser365 in the case of PN-1,10 it results in the formation of an acyl-intermediate complex, a massive molecular rearrangement, and the formation of a covalent SDS- and heat-stable enzyme–PN-1 complex.7
The precise molecular nature of the PN-1 protease inhibitory complexes under native conditions remains to be clarified but is assumed to follow the 1:1 covalently linked stoichiometric model classically observed for serpins. In vitro, PN-1 has been shown to rapidly inhibit different serine proteases (Table 1),7,11-13 including trypsin and thrombin,11 tPA and uPA,11 plasmin and factor Xa,7 factor XIa,12 activated protein C,13 and factor VII-activating protease (FSAP).14 Like many other serpins, the affinity of PN-1 for its target proteases can be enhanced by heparin, which acts as a bridge between the serpin and the protease, leading to a ternary complex15 and thus enhancing the rate of complex formation. The heparin-binding site of PN-1 contains 7 lysine residues that are located between residues 90 and 105 in the amino-terminal region of the protein.16 Heparin stimulates markedly the rate of inhibition of thrombin by PN-1.11,17 Interestingly, in vitro studies demonstrated that PN-1 inactivates thrombin at approximately a 100-fold faster rate than AT.18 In the presence of heparin, PN-1 is still a much faster inhibitor of thrombin than AT, the most important circulating inhibitor of thrombin.7,19 Heparin also strongly accelerates FXIa inhibition by PN-1, making PN-1 a far better inhibitor of FXIa than C1 inhibitor.12
Summary of published Ka values (M−1·s−1) of protease inhibition by PN-1
| Ka (M−1 × s−1) . | |||
|---|---|---|---|
| Enzyme . | Without heparin . | With heparin . | References . |
| Thrombin | 6-8.3 × 105 | 0.7-1.6 × 109 | 7,11 |
| Trypsin | 2.2-4.2 × 107 | 1 × 107 | 7,11 |
| uPA | 1.5-1.7 × 105 | 9.6 × 105 | 11, personal data* |
| tPA | 1.2-3 × 104 | 3.4 × 104 | personal data* |
| Plasmin | 1-2.3 × 105 | 1-4.1 × 105 | 7,11, personal data* |
| Factor Xa | 5.1 × 103 | 3.5 × 105 | 7 |
| Factor XIa | 7.9 × 104 | 1.7 × 106 | 12 |
| Activated protein C | 5.2 × 103 | 2.3 × 105 | 13 |
| Ka (M−1 × s−1) . | |||
|---|---|---|---|
| Enzyme . | Without heparin . | With heparin . | References . |
| Thrombin | 6-8.3 × 105 | 0.7-1.6 × 109 | 7,11 |
| Trypsin | 2.2-4.2 × 107 | 1 × 107 | 7,11 |
| uPA | 1.5-1.7 × 105 | 9.6 × 105 | 11, personal data* |
| tPA | 1.2-3 × 104 | 3.4 × 104 | personal data* |
| Plasmin | 1-2.3 × 105 | 1-4.1 × 105 | 7,11, personal data* |
| Factor Xa | 5.1 × 103 | 3.5 × 105 | 7 |
| Factor XIa | 7.9 × 104 | 1.7 × 106 | 12 |
| Activated protein C | 5.2 × 103 | 2.3 × 105 | 13 |
All constants determined at 37°C, except Evans et al,7 which was determined at 20°C.
PN-1 indicates protease nexin-1; tPA, tissue plasminogen activator; and uPA, urokinase plasminogen activator.
V.A., September 2001.
In contrast, heparin induces no significant change in plasminogen activators (V.A., personal data, September 2001) and plasmin7 inhibition by PN-1, probably because these proteases do not exhibit high affinity for heparin. Unlike AT, PN-1 complexed with thrombin does not lose affinity for heparin.7,15 This finding might be of importance for the catabolism of thrombin-PN-1 complexes. Indeed, PN-1/protease complexes are actively internalized from the pericellular environment by low-density lipoprotein receptor–related protein 1 (LRP1) via an interaction with cell-surface heparins or heparan sulfate proteoglycans, as observed in fibroblasts. In contrast, the catabolism of uPA–PN-1 complexes, also mediated by the LRP, proceeds through a pathway that uses the uPA receptor.20,21 The FSAP–PN-1 complexes have also been shown to bind to the LRP and to be subsequently internalized in vascular smooth muscle cells.14
Cell expression of PN-1 in the vascular system
In contrast to AT and PAI-1, which are synthesized by the liver and secreted into the blood, PN-1 is barely detectable in plasma22 but is found in many organs, such as brain, male and female reproductive systems, kidneys, lungs, cartilage, spleen, and muscle.23 PN-1 is also largely expressed in the heart,23 where a high level of PN-1 promotor activation has been observed in mice.24 Unpublished data from our group confirmed the strong immunohistochemical staining of PN-1 in the human myocardium (Figure 1). Moreover, PN-1 expression in striated skeletal muscle cells has been found to depend on the differentiation state of the cells.25 Further investigation is necessary to determine whether PN-1 expression is up-regulated after myocardial injury and participates in the control of tissue remodeling.
Immunohistochemical localization of PN-1 in human heart. PN-1 is homogeneously distributed in the myocardial tissue. A negative IgG control of PN-1 immunostaining was completely negative.
Immunohistochemical localization of PN-1 in human heart. PN-1 is homogeneously distributed in the myocardial tissue. A negative IgG control of PN-1 immunostaining was completely negative.
Injury-related cytokines induce an increase in PN-1 expression in different cell types.26,27 The first evidence for the presence of PN-1 in blood vessels came from immunohistochemical studies demonstrating an abundance of PN-1 around cerebral blood vessels.28 Direct evidence of PN-1 expression in the arterial wall has been also provided in rat aortas29 and human aortic and mammary arteries.30 PN-1 is expressed in all 3 tunica of the vascular wall, the intimal, medial, and adventitial layers, and is synthesized by their respective predominant stromal cells: endothelial cells,31 smooth muscle cells (SMCs),29 and fibroblasts.32
Our group demonstrated that PN-1 expression is tightly regulated. It is increased in the media of hypertensive rats29 and decreased in vascular SMCs stimulated with thrombin via an indirect mechanism involving fibroblast growth factor-2.33 PN-1 is also present in blood cells. We and others detected PN-1 in monocytes30 and in platelets by indirect34 and direct approaches.30 Most of platelet PN-1 is stored in the α-granules, but a minor fraction is also present at the surface of resting platelets.35 When taking a blood platelet concentration of ∼ 3 × 108/mL, we have estimated the concentration of platelet PN-1 released by platelets at approximately 15 to 20 nmol/L. Moreover, by comparing PN-1 expression in different cell lysates via Western blot analysis, we observed that the amount of PN-1 in platelets is more important than the amount observed in vascular cells such as endothelial cells or smooth SMCs (Y.B. and M.-C.B., personal data, January 2006). PN-1 expression is also regulated in blood cells. It is up-regulated in monocytes in response to stimulation with lipopolysaccharides, whereas it is down-regulated during monocyte-macrophage differentiation in which degraded forms of PN-1 were produced, suggesting a modified trafficking process.30
Platelet PN-1 in thrombus formation and dissolution
The finely tuned time and location-dependent control of platelet and fibrin plug formation and dissolution is essential for efficient hemostasis. The fact that platelets represent a significant reservoir of PN-1 raises the question of how platelet PN-1 can affect thrombus growth. Active and heparin-bound PN-1 is secreted during platelet activation and efficiently inhibits thrombin, thereby inhibiting fibrin formation, thrombin-induced platelet activation, and amplification of thrombin generation in vitro. This was witnessed in both human and mouse platelets. The inhibitory activity of PN-1, secreted during platelet activation, was blocked when secreted products of activated human platelets incubated with a PN-1–blocking antibody were used or was absent when platelet secretion products from PN-1–deficient mice were used.35 Tissue factor–induced thrombin generation in platelet-rich plasma (PRP), measured with the thrombogram method, was accelerated and increased when either human PRP preincubated with a PN-1–blocking antibody or PRP from PN-1–deficient mice was used.35
A complete deficiency of PN-1 in mice36 does not result in any alteration of the vascular phenotype. However, we observed that PN-1 deficiency significantly increases (1) the rate and extent of platelet aggregation, as well as the surface exposure of P-selectin, in response to low doses of thrombin; and (2) the speed of thrombin generation in platelet-rich plasma.35 Moreover ex vivo studies based on thrombus formation in whole blood under conditions of flow together with in vivo studies based on a model of ferric chloride (FeCl3)–induced thrombosis in mesenteric arterioles and venules revealed that thrombus formation was significantly accelerated in PN-1–deficient mice compared with wild-type mice (Figure 2A). In fact, PN-1 imposes a local threshold concentration of thrombin below which platelet activation cannot proceed and therefore plays a critical protective role against thrombosis.
PN-1 is antithrombotic and antifibrinolytic. (A) Time to occlusion of mesenteric venules measured after application of 15% FeCl3 in wild-type and PN-1–deficient mice. ***P < .001 (linear mixed-effects model) versus wild type. (B) Quantification of the incidence of recanalyzed vessels within 1 hour after tPA treatment after an occlusion induced by 15% FeCl3. The incidence of recanalization was 15% in wild-type mice (2 of 13 vessels) and 92% in PN-1–deficient mice (12 of 13 vessels).
PN-1 is antithrombotic and antifibrinolytic. (A) Time to occlusion of mesenteric venules measured after application of 15% FeCl3 in wild-type and PN-1–deficient mice. ***P < .001 (linear mixed-effects model) versus wild type. (B) Quantification of the incidence of recanalyzed vessels within 1 hour after tPA treatment after an occlusion induced by 15% FeCl3. The incidence of recanalization was 15% in wild-type mice (2 of 13 vessels) and 92% in PN-1–deficient mice (12 of 13 vessels).
Platelets not only initiate thrombus formation and participate in thrombus growth but also contribute to thrombus stability by preventing fibrinolysis. Until now, PAI-1 released locally by activated platelets was assumed to be the major contributor to thrombus stabilization by inhibiting endogenous fibrinolysis.37,38 However, PAI-1–independent mechanisms have also been proposed to contribute to platelet-dependent inhibition of fibrinolysis.39 Interestingly, PN-1 inhibits not only plasmin generation induced by fibrin-bound tPA but also fibrin-bound plasmin and thereby decreases the rate of fibrinolysis, as observed in an ex vivo model of platelet-rich clot lysis.40 This was also evidenced on both human and mouse platelets. Indeed, platelet-rich clot lysis was enhanced when they were obtained from human platelet-rich plasma in the presence of a PN-1–blocking antibody or from PN-1–deficient mice platelet-rich plasma. Moreover, an acceleration of the clot lysis front was observed in both mice PN-1–deficient clots, and human clots, in the presence of a PN-1–blocking antibody. PN-1 thus appears to be an underestimated negative regulator of fibrinolysis via its ability to inhibit both generation and activity of plasmin within the clot.
Regulation of fibrinolysis by PN-1 is particularly well illustrated in an in vivo model of tPA-induced thrombolysis. Using this model, we demonstrated that PN-1 deficiency accelerates and enhances thrombolysis after treatment with tPA (Figure 2B).40 It appears that both PAI-1 and PN-1 play a complementary role in maintaining the fibrin clot. Regulation of plasmin generation by PAI-1 may be most effective at the interface between plasma and the surface of the fibrin clot, because PAI-1 has no access to the catalytic domain of fibrin-bound tPA.41 In contrast, we can speculate that PN-1 is rather more involved in the protection of the fibrin clot core, because fibrin-bound plasmin and tPA remain accessible to PN-1. Additional studies are needed to clarify the respective role of each serpin in physiologic, pathologic or therapeutic fibrinolysis.
PN-1 is a cell regulator in the vascular system
Besides that stocked in platelets, the physiologic distribution of PN-1 is primarily localized at the cell surface as a result of the high affinity of PN-1 for glycosaminoglycans (GAGs) present in large amounts on cell membranes,15 which trap and potentiate PN-1 activity within the pericellular space. There are indeed several examples in which the activity of proteases on cells is modulated by PN-1 bound to cell-surface GAGs. One example concerns the role played by PN-1 at the interface between blood and the endothelium. Thrombomodulin is a membrane glycoprotein specifically expressed on endothelial cells that induces a shift in thrombin specificity. Indeed, when bound to thrombomodulin, thrombin loses its procoagulant activity, including its ability to cleave fibrinogen and activate platelets, whereas its anticoagulant activity is fully expressed because of an increased rate of protein C activation. Immunofluorescence studies, together with immunoprecipitation and immunoblot analysis, demonstrated that PN-1 binds to the chondroitin sulfate moiety of thrombomodulin.42 This interaction results in a marked enhancement in the inhibition of fibrin formation and a limitation of the generation of activated protein C.42 Another example concerns the role played by PN-1 expressed in the arterial media, where it controls protease activities in vascular SMCs. It decreases the mitogenic response of the cells to thrombin29 and prevents the proapoptotic effect of high thrombin concentrations.43 SMCs synthesize and secrete tPA that is able to drive plasminogen activation to plasmin at the cell surface, leading to matrix degradation, cell detachment and death.44 PN-1 was shown to inhibit plasmin generation on the cell surface.33 It can be hypothesized that some protease–PN-1 complexes are cleared from the vessel wall by internalization via LRP as observed for FSAP-PN-1 complexes.45 Therefore, PN-1 is proposed to actively participate in limiting matrix breakdown.
The net effect of proteases on vascular cells might be regulated by the presence of PN-1. Thus, local variations in PN-1 expression are likely determinants for the regulation of thrombin- or plasmin-induced vascular responses. Whether PN-1 expression is variable in different vascular beds remains to be established.
The aforementioned described cellular effects of PN-1 within the vascular system are related to its ability to inhibit its target serine proteases. However, we observed that PN-1 also exhibits specific and direct effects on vascular cells, effects that were hypothesized to be independent of its AT activity.46 Indeed, overexpression of PN-1 by vascular SMCs resulted in a significant reduction in adhesion, spreading, and migration on a matrix of vitronectin. An attractive explanation for such observations is a direct inhibition by PN-1 of cell binding to vitronectin related to the high binding affinity of PN-1 to this glycoprotein, as shown by direct-binding in vitro assays.47 However, such an effect of PN-1 should be further demonstrated in vivo, and the consequences of PN-1 interaction with its multiple cell partners (eg, GAGs, vitronectin, LRP) need to be explored.
PN-1 in vascular diseases
A lack of control of protease activity is known to be critical in vessel injury and is assumed to contribute to pathologic processes. Exacerbated thrombin and plasminergic protease activities are, for instance, involved in the development of atherothrombosis and aneurysm. An important issue thereby concerns the regulation of such proteases within the vessel wall. In this context, the aforementioned data support the hypothesis that PN-1 might be a significant actor in the regulation of serine protease activities within vascular lesions. Histochemical studies demonstrated the presence of PN-1 in advanced carotid atherosclerotic lesions.48 Moreover, our group showed that the accumulation of PN-1 is already detectable in early lesions and increases in complicated plaques. Combined histochemical and biochemical analysis have demonstrated that monocytes/macrophages and platelets are the major sources of PN-1 within the plaque necrotic core and the mural thrombus.30 Whether PN-1 accumulation has a protective or a deleterious role in the progression of atherothrombosis cannot yet be anticipated.
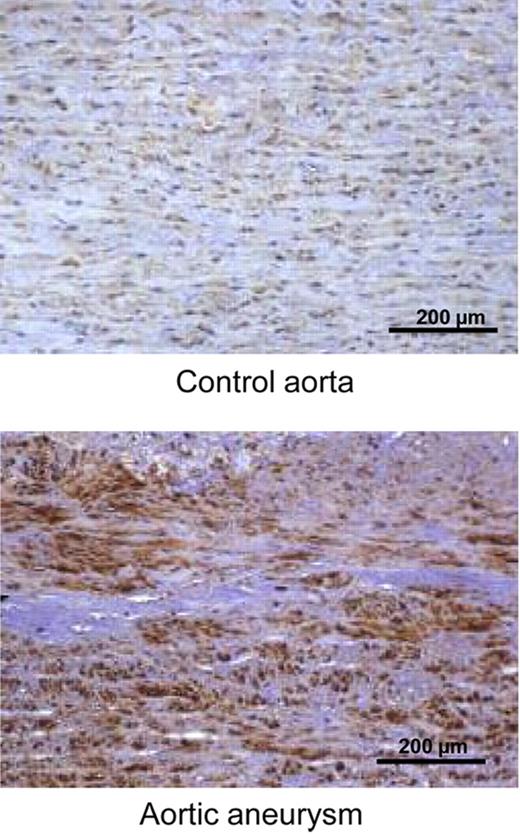
The potential role of PN-1 in thoracic aneurysms of the ascending aorta (TAA) also deserves some interest. TAA have been characterized by an increase in transmural plasminogen transport, leading to a very significant activation of the fibrinolytic system within the arterial wall of TAA.49 Interestingly, we observed that PN-1 is overexpressed in TAA (Figure 3). PN-1 expression is thus acutely up-regulated in different vascular pathologies, suggesting that it is one of the numerous proteins whose role is to maintain or restore homeostasis during damage or stress. These observations lead to the appealing hypothesis that PN-1 overexpression is a mechanism of cell defense against aggressive proteases, to limit the degeneration of the media by regulating protease-induced matrix degradation and protease-induced cell death and/or migration.
Immunohistochemical localization of PN-1 in human control aorta and thoracic aortic aneurysm. The immunostaining for PN-1 is diffuse throughout the medial layer in control aortas and largely increased in aortic aneurysm.
Immunohistochemical localization of PN-1 in human control aorta and thoracic aortic aneurysm. The immunostaining for PN-1 is diffuse throughout the medial layer in control aortas and largely increased in aortic aneurysm.
Perspectives and clinical applications for PN-1
Studies conducted during the last decade have allowed identification of PN-1 as an underestimated regulator in vascular physiology (Figure 4). No abnormal phenotype was observed in the unchallenged PN-1 knockout mouse except for male fertility defects,50 and until now no human deficiency has been described. However, our studies revealed PN-1 as an important regulating protein for appropriate responses to stressed conditions, as demonstrated in models in which thrombosis or fibrinolysis were triggered.
Several points deserve to be mentioned. First, one could speculate that modifications in PN-1 expression or function could represent a risk factor for cardiovascular diseases. In this context, it would be important to determine whether PN-1 expression and function are genetically regulated. Indeed, there is substantial evidence for a link between elevated PAI-1 levels and a greater risk for cardiovascular disease. Second, recent findings strongly suggest that the coordinated regulation of serine proteases by PN-1 and PAI-1 plays a key role under pathologic conditions. It would be very informative to determine the relative impact of each serpin in the global risk for thrombotic diseases.
The fact that PN-1 is important to protect the developing thrombus from premature lysis suggests that it could be used as a therapeutic target for thrombolysis. Thrombolytic therapy consists of the pharmacologic dissolution of the blood clot by intravenous infusion of plasminogen activators to restore arterial blood flow. Thrombolysis by recombinant tPA is of particular importance in the treatment of stroke, but its use is limited by the risk of adverse side effects, such as hemorrhage and neural toxicity. One could hypothesize that an antagonist of PN-1, by limiting its antifibrinolytic activity, could act as an adjuvant to thrombolytic therapy by increasing the efficacy of lower doses of tPA and thus decreasing its side effects. PN-1 is thus an attractive pharmacologic target to improve the therapeutic efficacy of classic thrombolytic agents.
Conclusion
Progress in PN-1 research during the last decade has revealed a significant contribution of this serpin to the regulation of coagulation and fibrinolysis, via its actions on thrombin, plasminogen activators, and plasmin. PN-1 can also modulate extracellular matrix degradation and vascular cell behavior. PN-1 can thus influence vascular remodeling or the development of vascular lesions. It is obvious that the complementary actions of PN-1 and PAI-1 are involved in the spatiotemporal regulation of thrombosis and fibrino/thrombolysis, but questions still remain to be answered to understand the role of each of these serpins in the development of vascular diseases.
Acknowledgments
This work was supported by Inserm, Université Paris Diderot, and Fondation de France (grant no. 2009002497).
Authorship
Contribution: M.-C.B., Y.B., B.R., V.A., J.-B.M., and M.J.-P. contributed to writing and revising the manuscript.
Conflict-of-interest disclosure: The authors declare no competing financial interests.
Correspondence: Marie-Christine Bouton, Unité Inserm U698, CHU Xavier Bichat, 46 rue Henri Huchard, 75877 Paris Cedex 18, France; e-mail: marie-christine.bouton@inserm.fr.




This feature is available to Subscribers Only
Sign In or Create an Account Close Modal