Human erythrocytes have a low basal permeability to L-glutamate and are not known to have a functional glutamate transporter. Here, treatment of human erythrocytes with arsenite was shown to induce the uptake of L-glutamate and D-aspartate, but not that of D-glutamate or L-alanine. The majority of the arsenite-induced L-glutamate influx was via a high-affinity, Na+-dependent system showing characteristics of members of the “excitatory amino acid transporter” (EAAT) family. Western blots and immunofluorescence assays revealed the presence of a member of this family, EAAT3, on the erythrocyte membrane. Erythrocytes infected with the malaria parasite Plasmodium falciparum take up glutamate from the extracellular environment. Although the majority of uptake is via a low-affinity Na+-independent pathway there is, in addition, a high-affinity uptake component, raising the possibility that the parasite activates the host cell glutamate transporter.
Introduction
It has long been recognized that after infection of the human erythrocyte by the malaria parasite Plasmodium falciparum, the host cell membrane undergoes a profound increase in its permeability to a diverse range of low molecular weight solutes including amino acids, sugars, nucleosides, and a range of organic and inorganic anions and cations.1,,,–5 The increased permeability facilitates the uptake into the infected cell of several key nutrients,6,–8 as well as the uptake of various antiparasitic agents.8,,,–12 Parasite-induced pathways also mediate both the efflux of metabolic wastes,6,13 and a marked change in the ionic composition of the host cell cytosol.4,14
The question of the number and origin of the pathways underpinning the parasite-induced increase in host erythrocyte permeability has been a vexed one. Subjecting uninfected human erythrocytes to oxidative stress,15,16 or to protein kinase A–mediated protein phosphorylation,17,–19 results in the activation of membrane channels that confer on the membrane of the uninfected cell, similar to permeability characteristics seen in the infected cell. This is consistent with at least some part of the parasite-induced permeability being attributed to the activation of endogenous host cell proteins. A recent paper has proposed a central role for an endogenous erythrocyte benzodiazopene receptor/voltage-dependent anion channel20 in forming the parasite-induced pathways. At the same time, there is evidence for the involvement of parasite-encoded proteins. After earlier observations of significant parasite-strain–specific differences in the electrophysiologic characteristics of parasite-induced ion conductances21,22 and the identification of parasite strains for which the infected erythrocyte has reduced permeability to various cytotoxic agents,10,11,23 Desai and colleagues have demonstrated a role for parasite-encoded “clag3” proteins in the formation of parasite-induced channels.24 Whether these proteins themselves form part of the channels is not yet clear.
Exposure of cells to arsenite is known both to induce oxidative stress and to perturb intracellular phosphorylation/dephosphorylation pathways.25 In a study of ferret erythrocytes, Flatman and Creanor demonstrated that treatment of these cells with arsenite resulted in the stimulation of an ion transporter, the Na+K+2Cl− cotransporter.26 In this work, we investigated the effect of arsenite treatment on the transport into human erythrocytes of the acidic amino acid, glutamate. Human erythrocytes have a low basal permeability to glutamate; however, the amino acid readily enters P falciparum–infected erythrocytes.1,2,27,28 Here we show that arsenite-treatment of (uninfected) human erythrocytes results in the activation of a high-affinity, Na+-dependent glutamate transport pathway, which has the functional characteristics of members of the “excitatory amino acid transporter” (EAAT) family.29,30 An analysis of the uptake of glutamate into P falciparum–infected erythrocytes revealed the presence of both low and high-affinity components. The implications of these results for our understanding of the malaria parasite-induced increase in the transport of amino acids across the infected erythrocyte membrane are discussed.
Methods
Cell culture
Human erythrocytes of blood groups O and A, Rh+, were obtained from either the Canberra branch of the Australian Red Cross Blood Service or the Marburg Blood Bank and infected with P falciparum (isolate 3D7). The infected erythrocytes were cultivated either under “shaking” conditions, in RPMI 1640 medium (PAA E15-840; supplemented with 0.5% wt/vol AlbuMax II (Invitrogen), 25mM HEPES (N-2-hydroxyethylpiperazine-N'-2-ethanesulfonic acid), 20mM glucose, 24 μg/mL gentamicin and 200μM hypoxanthine) at a hematocrit of 2%,31 or under “static” conditions in the same medium supplemented with 10% vol/vol human serum (from the Marburg Blood Bank).32 Experiments were carried out with trophozoite-stage P falciparum–infected erythrocytes (30-35 hours after invasion) enriched to 85%-95% parasitemia either using a VarioMACS separation unit (Miltenyi Biotec) as described elsewhere,6 or using the plasmagel method.33
Chemical treatment of uninfected erythrocytes
Uninfected erythrocytes were treated with several different chemical reagents. In each case the cells were incubated under the same culture conditions as parasitized erythrocytes for 24 hours before treatment.
Treatment of cells with arsenite was carried out as described by Flatman and Creanor with slight modifications.26 The cells were harvested from the culture, washed 3 times, and then resuspended in (glucose-free) Dulbecco PBS without Ca2+ or Mg2+ (PAA Laboratories). The washed erythrocytes were incubated at 37°C for 60 minutes with gentle agitation in Dulbecco PBS containing 1mM sodium-(meta)–arsenite or, in control experiments, sodium-arsenate-dibasic-heptahydrate (Sigma-Aldrich). The treated cells were then washed 3 times with Dulbecco PBS to remove the extracellular arsenite (or arsenate).
In one series of experiments, uninfected human erythrocytes were washed and resuspended in Dulbecco PBS, and then incubated with 3μM alphaxalone (5α-pregnan-3α-ol-11,20-dione; Sigma-Aldrich) for 10 minutes at 37°C under gentle agitation, and then washed 3 times with Dulbecco PBS to remove the alphaxalone.
Amino acid uptake measurements
The unidirectional influx of L-glutamate, D-aspartate, L-alanine, and D-glutamate into P falciparum–infected and uninfected erythrocytes was measured at 37°C using, L-[3H]-glutamate, D-[3H]-aspartate, L-[3H]-alanine (all from Perkin Elmer), and D-[3H]-glutamate (Hartmann Analytic), respectively.
In a typical influx experiment, uninfected erythrocytes, arsenite-treated uninfected erythrocytes and/or P falciparum–infected erythrocytes were suspended at a concentration of approximately 1 × 108 cells/mL in (glucose-free) Dulbecco PBS without Ca2+ or Mg2+, containing 37 × 103 Bq/mL (ie, 1 μCi/mL) of one of the radiolabeled amino acids. Unless specified otherwise, there were no unlabeled amino acids present in the extracellular medium; the final extracellular concentrations (as determined by the specific activities of each radiolabeled amino acid) were 20nM for L-glutamate, 78nM for D-aspartate, 21nM for D-glutamate, and 13nM for L-alanine. At predetermined time points, an aliquot of the suspension, containing approximately 2 × 107 cells was sampled and layered onto 500 μL of oil (dibutyl phthalate; Sigma-Aldrich) in a microcentrifuge tube, which was centrifuged immediately (18 000g, 2 minutes), thereby separating the cells from the extracellular medium. The supernatant solution above the oil was aspirated and the tubes were washed 3 times with water to remove residual radioactivity. After the final washing step, the oil was aspirated, the cell pellet was lysed by the addition of 500 μL of 0.1% wt/vol Triton X-100, and the protein was precipitated by the addition of 500 μL of 5% wt/vol trichloroacetic acid. The precipitated proteins were sedimented by centrifugation (12 000g for 10 minutes) and the supernatant solution was transferred to a vial for scintillation counting.
For those experiments in which full time courses are not shown, the initial rate of uptake of L-glutamate was estimated from the amount of L-[3H]-glutamate taken up for a period (10 minutes) that fell within the initial, approximately linear, portion of the L-[3H]-glutamate uptake time course.
To test the Na+-dependence of L-glutamate uptake, cells were washed 5 times, and then resuspended in a Na+-free solution containing either 150mM choline chloride, 150mM N-methyl-d-glucamine chloride, or 150mM KCl, together with 20mM sucrose and 10mM Tris-HCl (pH 7.4). Uptake into cells in these Na+-free media was compared with that in cells washed and resuspended in a solution containing 150mM NaCl, 20mM sucrose, and 10mM Tris-HCl (pH 7.4). At predetermined time points the cells were harvested and the samples were processed as previously described.
For the purpose of comparing the uptake of radiolabeled amino acids under different conditions uptake is expressed in terms of a distribution ratio (ie, the estimated concentration of radiolabel inside the cells relative to that in the extracellular solution). The estimation of the amount of radiolabel trapped in the extracellular space of the cell pellet, and the calculation of the distribution ratio, was performed as described elsewhere.6
Erythrocyte volume measurements
Erythrocyte volume estimates were made with a Scepter handheld automated cell counter (Milipore) fitted with a 40 μm Scepter sensor. Erythrocytes were suspended in PBS at 1 × 104 to 5 × 105 cells/mL. The Scepter provides a histogram of cell-volume distribution.
Measurement of extracellular Na+ concentration
In one experiment, the release of Na+ from P falciparum–infected erythrocytes into the Na+-free medium in which they had been suspended was monitored using ultra high pressure liquid chromatography (UHPLC; Dionex) linked to a charged aerosol detector (CAD; Dionex). The conditions were as described elsewhere34 and entailed using an Acclaim Trinity P1 column (3 μm, 2.1 × 150 mm; Dionex) run at 30°C with 60/40 vol/vol acetonitrile/20mM Ammonium acetate, pH 5, as the mobile phase. A 2 μL sample was injected and the flow rate was 0.5 mL/min. The CAD (Corona Ultra) was set to a gain of 100 pA with a medium filter and a nebulizer temperature of 30°C.
Protease treatment of intact red blood cells
The proteases trypsin and chymotrypsin were tested for their effects on the uptake of L-glutamate into uninfected erythrocytes treated with sodium arsenite. In a typical experiment, 5 × 108 arsenite–treated erythrocytes were washed 3 times with PBS, and then resuspended in PBS containing either trypsin or chymotrypsin at a concentration of 500 μg/mL. The suspension was incubated at 37°C for 30 minutes, under gentle agitation, and then the cells were washed 3 times in PBS to remove excess protease. The uptake of L-[3H]-glutamic acid into the cells was then measured as previously described.
In experiments in which erythrocytes were subjected to multiple rounds of arsenite and protease treatment, the erythrocytes were resuspended in approximately 10 mL RPMI 1640 at 37°C for at least 20 minutes after each round of arsenite/protease treatment to stabilize the treated cells.
Membrane preparation and immunoblotting
Uninfected erythrocytes and P falciparum–infected erythrocytes were lysed by 3 cycles of freezing and thawing in 5mM KH2PO4 containing a protease inhibitor cocktail (Calbiochem; set III, animal-free). The membrane fraction was sedimented by centrifugation of the lysate at 36 000g for 20 minutes at 4°C. Membrane proteins were solubilized in sodium dodecyl sulfate (SDS)–polyacrylamide gel electrophoresis (PAGE) sample buffer for 10 minutes at 95°C, separated on either a 5%-15% or 4%-12% SDS-PAGE, as specified, and then transferred to a nitrocellulose membrane.
Commercial antibodies were used for the detection of EAAT1-5. A rabbit polyclonal antibody against EAAT1 (SantaCruz), goat polyclonal antibodies against EAAT2, EAAT4, and EAAT5 (SantaCruz), and a mouse monoclonal antibody against EAAT3 (Invitrogen), were used, each at a dilution of 1:500. A rabbit polyclonal serum against spectrin was obtained from Sigma-Aldrich. Primary antibodies were detected with horseradish peroxidase-conjugated anti–goat (Sigma-Aldrich), anti–rabbit (Sigma-Aldrich) or anti–mouse immunoglobulin (Ig)G antibodies (Dako), at a dilution of 1:2000.
Localization of EAAT3 by immunofluorescence assay
Immunofluorescence assays (IFAs) were performed on uninfected erythrocytes and on trophozoite-stage P falciparum–infected erythrocytes as described elsewhere,35 using a monoclonal anti-EAAT3 (Invitrogen; 1:1000) and monoclonal anti–Band 3 antibody (Sigma-Aldrich; 1:1000). Images were acquired using a Zeiss Axio Observer Z1 inverse epifluorescence microscope system with appropriate filter sets, equiped with an AxioCam MRm camera and Axiovision 4 software. The objective lens used was a Plan Apochromat 100×/1.4 oil DIC (all from Zeiss). Images were processed using Aperture 2 (Apple).
Results
Arsenite-treatment stimulates the uptake of L-glutamate and D-aspartate into human erythrocytes
The mature human erythrocyte has a low permeability to the acidic amino acid L-glutamate.36 On treatment of human erythrocytes with arsenite there was a profound increase in the rate of uptake of this amino acid (Figure 1A). Arsenite therefore induces or activates one or more L-glutamate transport pathways in the erythrocyte membrane. Under the conditions of the experiment the rate of uptake of L-glutamate into arsenite-treated cells was similar to that into erythrocytes infected with the human malaria parasite, P falciparum (Figure 1A).
Time courses for the uptake of different amino acids. The data are from uninfected human erythrocytes (▴), arsenite-treated uninfected human erythrocytes (○), and P falciparum–infected human erythrocytes (●). The influx of L-[3H]-glutamate (A), D-[3H]-aspartate (B), D-[3H]-glutamate (C), and L-[3H]-alanine (D) was measured for a period of 20 minutes at 37°C. The cells were suspended in (glucose-free) PBS and in each case the radiolabeled compounds were the only extracellular amino acids present. The extracellular concentrations were 20nM for L-glutamate, 78nM for D-aspartate, 21nM for D-glutamate, and 13nM for L-alanine. The uptake data are expressed in terms of a distribution ratio (ie, the estimated concentration of radiolabel inside the cell relative to that in the extracellular solution). The data were averaged from 5 separate experiments performed on different days, on erythrocytes from different donors, and are shown ± SEM.
Time courses for the uptake of different amino acids. The data are from uninfected human erythrocytes (▴), arsenite-treated uninfected human erythrocytes (○), and P falciparum–infected human erythrocytes (●). The influx of L-[3H]-glutamate (A), D-[3H]-aspartate (B), D-[3H]-glutamate (C), and L-[3H]-alanine (D) was measured for a period of 20 minutes at 37°C. The cells were suspended in (glucose-free) PBS and in each case the radiolabeled compounds were the only extracellular amino acids present. The extracellular concentrations were 20nM for L-glutamate, 78nM for D-aspartate, 21nM for D-glutamate, and 13nM for L-alanine. The uptake data are expressed in terms of a distribution ratio (ie, the estimated concentration of radiolabel inside the cell relative to that in the extracellular solution). The data were averaged from 5 separate experiments performed on different days, on erythrocytes from different donors, and are shown ± SEM.
Similar results were obtained with another acidic amino acid, D-aspartate, which showed negligible uptake into normal human erythrocytes but which entered both arsenite-treated (uninfected) erythrocytes and P falciparum–infected erythrocytes at similar rates (Figure 1B).
By contrast, 2 other amino acids, D-glutamate and L-alanine, showed negligible uptake into both normal, uninfected human erythrocytes and arsenite-treated erythrocytes under the conditions of the experiment, although readily entering P falciparum–infected erythrocytes (Figures 1C-D, respectively).
Treatment of erythrocytes with arsenate, rather than arsenite, had no significant effect on the uptake of any of the amino acids tested (data not shown).
All of the results presented here were obtained using erythrocytes of blood group O, and in the case of the P falciparum–infected erythrocytes, using cultures maintained in media containing Albumax, with enrichment of infected cells carried out using a VarioMACS separation unit. Very similar results were obtained in experiments using erythrocytes of blood group A, and in the case of the infected erythrocytes, when the cultures were maintained in media containing 10% vol/vol human serum and enriched by the plasmagel method (data not shown).33
The previous finding by Flatman and Creanor that treatment of ferret erythrocytes with arsenite activates the Na+K+2Cl− cotransporter raises the possibility that a similar activation of this transporter in human erythrocytes might result in significant changes in ion content, and hence cell volume.26 To test this we compared the volume of erythrocytes incubated for 1 hour in PBS containing 1mM arsenite to that of erythrocytes incubated for the same period in the absence of arsenite. The initial mean erythrocyte volume was 73.3 ± 1.8 fl (n = 10). After 1 hour incubation, the mean cell volume of those cells exposed to arsenite was 67.2 ± 2.0 fl (n = 5), whereas that of cells incubated for the same period in the absence of arsenite was 67.4 ± 1.9 fl (n = 5). The arsenite treatment therefore had no significant effect on erythrocyte volume (P = .42; paired t test), and thus on total ion content. Nor was there any significant change in cell morphology as observed by light microscopy (not shown). It should be noted that in the course of the 1 hour incubation with arsenite, a small proportion (2.4 ± 0.6%; n = 5, P = .002) of the cells present underwent hemolysis.
Na+-dependence of the arsenite-induced uptake of L-glutamate
The data presented in Figure 1 show that arsenite-treatment of mature human erythrocytes activates one or more pathways that mediate the uptake of L-glutamate and D-aspartate, but not that of D-glutamate or L-alanine. These selective properties are typical of members of the well-characterized EAAT family.29,30 Members of this family transport glutamate in “symport” with Na+ across the membranes of a range of different cell types. The Na+-dependence of the influx of L-glutamate into arsenite-treated erythrocytes was therefore investigated by comparing uptake in cells suspended in a Na+-containing medium with that measured in cells suspended in solutions in which Na+ was replaced with the monovalent organic cation choline. As shown in Figure 2A, the arsenite-induced L-glutamate uptake showed a strong Na+-dependence, with removal of the extracellular Na+ causing an almost complete cessation of the uptake of radiolabeled amino acid, consistent with the involvement of an EAAT. By contrast, the uptake of L-glutamate into P falciparum–infected erythrocytes showed only a partial apparent Na+-dependence, with the initial rate of uptake of L-glutamate into parasitized erythrocytes undergoing a significant (33 ± 1%; n = 5; P = .03; paired t test) decrease on replacement of Na+ with choline in the extracellular medium (Figure 2B). Similar results were obtained in experiments in which Na+ was replaced with N-methyl-d-glucamine (results not shown). In a control experiment, the possibility that the leakage of Na+ from P falciparum–infected erythrocytes led to a significant increase in the extracellular [Na+] under the conditions of the experiment was investigated. Analysis of the Na+ content of the extracellular solution using UHPLC linked to a CAD revealed that under the conditions of the experiment (1 × 104P falciparum–infected erythrocytes suspended in Na+-free, choline-containing medium for 30 minutes), the extracellular Na+ concentration increased by < 20μM.
Sodium dependence of L-glutamate uptake. Time courses for the uptake of L-[3H]-glutamate into arsenite-treated (A) and P falciparum–infected (B) human erythrocytes (RBCs) in the presence or absence of extracellular Na+. The cells were suspended in a solution containing 20mM sucrose and 10mM Tris-HCl (pH 7.4) together with either 150mM sodium chloride (●) or 150mM choline chloride (○). The uptake data are expressed in terms of a distribution ratio (ie, the estimated concentration of radiolabel inside the cell relative to that in the extracellular solution). Symbols show data averaged from 5 independent experiments, ± SEM.
Sodium dependence of L-glutamate uptake. Time courses for the uptake of L-[3H]-glutamate into arsenite-treated (A) and P falciparum–infected (B) human erythrocytes (RBCs) in the presence or absence of extracellular Na+. The cells were suspended in a solution containing 20mM sucrose and 10mM Tris-HCl (pH 7.4) together with either 150mM sodium chloride (●) or 150mM choline chloride (○). The uptake data are expressed in terms of a distribution ratio (ie, the estimated concentration of radiolabel inside the cell relative to that in the extracellular solution). Symbols show data averaged from 5 independent experiments, ± SEM.
The Na+ concentration [Na+]-dependence of the influx of L-glutamate into arsenite-treated (uninfected) erythrocytes was investigated and the data are presented in Figure 3. L-glutamate influx showed an approximately hyperbolic dependence on [Na+], with a half-maximal effect at 11.7 ± 1.8 mM.
[Na+]-dependence of L-[3H]-glutamate into arsenite-treated (uninfected) human erythrocytes. The cells were suspended in a solution containing choline chloride + NaCl at a combined concentration of 150mM, together with 20mM sucrose and 10mM Tris-HCl (pH 7.4). Uptake of L-[3H]-glutamate was measured for 10 minutes at 37°C. The fitted line is a rectangular hyperbola (v = vmax [Na+]/(B + [Na+])) with B, the [Na+] at which uptake is half-maximal, 11.7 ± 1.8mM. The data were averaged from 5 independent experiments, ± SEM.
[Na+]-dependence of L-[3H]-glutamate into arsenite-treated (uninfected) human erythrocytes. The cells were suspended in a solution containing choline chloride + NaCl at a combined concentration of 150mM, together with 20mM sucrose and 10mM Tris-HCl (pH 7.4). Uptake of L-[3H]-glutamate was measured for 10 minutes at 37°C. The fitted line is a rectangular hyperbola (v = vmax [Na+]/(B + [Na+])) with B, the [Na+] at which uptake is half-maximal, 11.7 ± 1.8mM. The data were averaged from 5 independent experiments, ± SEM.
Kinetics of L-glutamate uptake
Figure 4A shows the effect of increasing concentrations of unlabeled L-glutamate on the uptake of L-[3H]-glutamate into arsenite-treated human erythrocytes, measured for 10 minutes. The cells were suspended in PBS. Unlabeled L-glutamate inhibited the uptake of L-[3H]-glutamate in a concentration-dependent manner, with the uptake of radiolabeled amino acid being reduced by 98 ± 1% (n = 3; P = .001; paired t test) in the presence of 10μM unlabeled L-glutamate. The data are consistent with arsenite activating a saturable, high-affinity transporter, for which the unlabeled L-glutamate competes with the radiolabeled substrate. In Figure 4A (inset), the data are presented in terms of the concentration-dependence of L-glutamate uptake. Fitting the Michaelis-Menten equation to the data yielded a Km of 55 ± 9nM and a Vmax of 17.2 ± 1.7 nmol/(1012 cells/hour).
Saturation of glutamate uptake. Effect of unlabeled L-glutamate on the uptake of L-[3H]-glutamate into (A) arsenite-treated uninfected human erythrocytes (RBCs) suspended in (glucose-free) PBS and (B-C) P falciparum–infected human erythrocytes suspended in the presence (B) and absence (C) of extracellular Na+ (with the extracellular solutions as described in Figure 2). In each case the uptake of L-[3H]-glutamate was measured for 10 minutes at 37°C, with the concentration of unlabeled L-glutamate in the extracellular solution ranging from 0 to 100μM. Uptake of L-[3H]-glutamate is expressed as a percentage of that measured in the absence of unlabeled L-glutamate in Na+-containing medium. The data are averaged from 3 independent experiments. (A) The inset shows the concentration-dependence of L-glutamate uptake, with the line drawn using the Michaelis-Menten equation (Km of 55 ± 9nM; Vmax of 17.2 ± 1.7 nmol/[1012 cells/hour]). The error bars indicate ± SEM. (B-C)The insets are Eadie-Hofstee plots of the data, which illustrate the fact that both in the presence (B) and absence (C) of extracellular Na+ there is one or more high-affinity component (dotted line) and 1 or more low-affinity component (dashed line) to the uptake of L-glutamate into P falciparum–infected erythrocytes. For clarity, the data are shown without error bars, with the exception of the inset in panel A.
Saturation of glutamate uptake. Effect of unlabeled L-glutamate on the uptake of L-[3H]-glutamate into (A) arsenite-treated uninfected human erythrocytes (RBCs) suspended in (glucose-free) PBS and (B-C) P falciparum–infected human erythrocytes suspended in the presence (B) and absence (C) of extracellular Na+ (with the extracellular solutions as described in Figure 2). In each case the uptake of L-[3H]-glutamate was measured for 10 minutes at 37°C, with the concentration of unlabeled L-glutamate in the extracellular solution ranging from 0 to 100μM. Uptake of L-[3H]-glutamate is expressed as a percentage of that measured in the absence of unlabeled L-glutamate in Na+-containing medium. The data are averaged from 3 independent experiments. (A) The inset shows the concentration-dependence of L-glutamate uptake, with the line drawn using the Michaelis-Menten equation (Km of 55 ± 9nM; Vmax of 17.2 ± 1.7 nmol/[1012 cells/hour]). The error bars indicate ± SEM. (B-C)The insets are Eadie-Hofstee plots of the data, which illustrate the fact that both in the presence (B) and absence (C) of extracellular Na+ there is one or more high-affinity component (dotted line) and 1 or more low-affinity component (dashed line) to the uptake of L-glutamate into P falciparum–infected erythrocytes. For clarity, the data are shown without error bars, with the exception of the inset in panel A.
A somewhat different pattern was observed in P falciparum–infected erythrocytes. Figure 4B shows the effect of increasing concentrations of unlabeled L-glutamate on the uptake of L-[3H]-glutamate (measured for 10 minutes) into P falciparum–infected erythrocytes suspended in a Na+-containing medium. As the concentration of unlabeled L-glutamate increased, there was as in the arsenite-treated cells, a decrease in the uptake of L-[3H]-glutamate. However the maximum decrease, observed at L-glutamate concentrations > 5 to 10 μM was ∼ 45% of the total uptake measured in the absence of unlabeled L-glutamate (contrasting with the 98% decrease seen for arsenite-treated cells under the same conditions); the remaining ∼ 55% of the uptake of radiolabel was largely unaffected by unlabeled L-glutamate, up to a concentration of 100μM.
As is illustrated in Figure 4C, when the experiment was repeated for P falciparum–infected erythrocytes suspended in a Na+-free solution, containing choline in place of Na+, the uptake of L-[3H]-glutamate measured for 10 minutes in the absence of unlabeled L-glutamate was lower than that measured in Na+-containing medium (consistent with the results shown in Figure 2B). On addition of unlabeled L-glutamate to infected cells in Na+-free medium the uptake of radiolabel again decreased. The maximum decrease, observed at L-glutamate concentrations > 5 to 10μM, was approximately 30% of the total uptake measured in the absence of unlabeled L-glutamate, with the remaining ∼ 70% of the uptake of radiolabel largely unaffected by unlabeled L-glutamate, up to a concentration of 100μM.
The insets of Figure 4B and C show Eadie-Hofstee plots of the data. These serve to illustrate the fact that both in the presence and absence of extracellular Na+ there are both high-affinity and low-affinity components to the uptake of L-glutamate into P falciparum–infected erythrocytes. Specifically, in both media, there is at least one high-affinity L-[3H]-glutamate uptake component (responsible for the decreased uptake of radiolabel seen as the concentration of unlabeled L-glutamate was increased up to 5-10μM) and at least 1 low-affinity L-[3H]-glutamate uptake components (responsible for the residual L-[3H]-glutamate uptake that remains in the presence of 10-100μM L-glutamate).
In the (unpaired) experiments illustrated in Figure 4B and C the magnitude of the low-affinity uptake of L-[3H]-glutamate into parasitized erythrocytes (as measured in the presence of > 10μM L-glutamate) was somewhat lower in cells suspended in Na+-free (choline) solution than in cells suspended in the Na+-containing medium. In paired experiments in which the (low-affinity) uptake of L-[3H]-glutamate into parasitized erythrocytes was measured in media containing 100μM L-glutamate, replacement of Na+ with choline in the extracellular medium resulted in a small (though not statistically significant) decrease (9%; P > .1; n = 3; paired t test) in glutamate uptake (data not shown). Addition of 100μM furosemide to parasitized cells suspended in Na+-containing medium in the presence of 100μM L-glutamate resulted in a 77 ± 3% reduction in the uptake of L-[3H]-glutamate measured for 10 minutes (P < .001; n = 3; paired t test; data not shown). The low-affinity L-glutamate uptake pathway is therefore largely Na+-independent, but furosemide-sensitive.
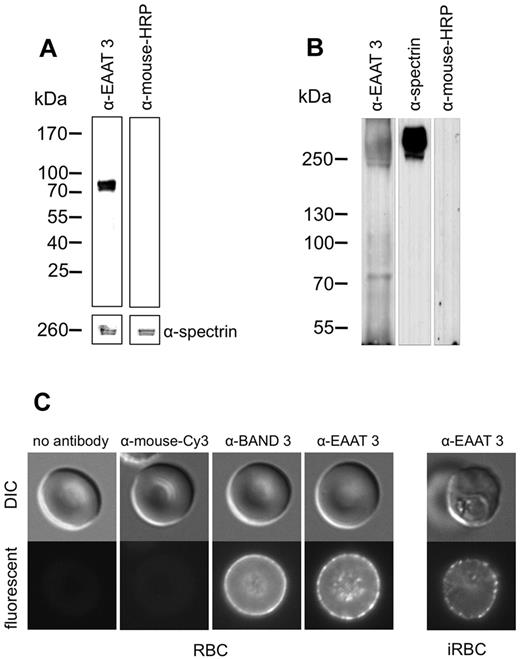
EAAT3 is detectable in the plasma membrane of human erythrocytes
The observation that arsenite-treatment of (uninfected) human erythrocytes induces a high-affinity, Na+-dependent L-[3H]-glutamate uptake pathway is consistent with arsenite activating one or more members of the EAAT family in the erythrocyte membrane. To our knowledge no member of this family has been shown to be present in the human erythrocyte. Antibodies against EAAT1-EAAT5 were tested for their ability to detect proteins in an erythrocyte membrane preparation. With only one of these, a monoclonal antibody against EAAT3, was a protein detected by immunoblotting. Figure 5A shows a Western blot, with a band at an estimated molecular mass of 72 kDa, close but not identical to that of EAAT3 (60 kDa). A similar discrepancy between the molecular mass of the protein as estimated from Western blots, and the actual molecular mass has been noted previously and may be because of the protein being heavily glycosylated.37 Similar reactions were obtained with membrane preparations of arsenite-treated uninfected erythrocytes and with P falciparum–infected erythrocytes (data not shown). In some Western blots there were, in addition to the 72 kDa band, immunoreactive bands at approximately 250 kDa (Figure 5B). These bands were distinct from those of human spectrin (Figure 5B). Similar higher molecular weight bands were also observed when using several other anti-EAAT3 antibodies (data not shown). It is probable that these bands represent oligomeric forms of EAAT3, as have been observed for other glutamate transporters.38
Detection of EAAT3 using Western blot and indirect immunofluorescence. (A-B) Western blots of the membrane fraction of uninfected human erythrocytes. For panel A approximately 2 × 107 cells were lysed and the membrane fraction was separated on a 5%-15% SDS-PAGE. The separated membrane proteins were blotted onto nitrocellulose and probed with a monoclonal antibody against EAAT3 (left lane). Spectrin served as a loading control. Incubation of the blot with the secondary (rabbit anti–mouse) antibody alone gave no detectable bands (right lane). For panel B approximately 5 × 107 cells were lysed and the membrane fraction was separated on a 4%-12% SDS-PAGE. The gel was processed as described for panel A. (C) IFA images showing punctate staining of the membrane of both uninfected (RBC) and P falciparum–infected (iRBC) human erythrocytes by the anti-EAAT3 monoclonal antibody. Uninfected erythrocytes (left panel) and erythrocytes infected with trophozoite stage parasites (right panel) were fixed and incubated either without antibody, with the secondary antibody alone, with an antibody against human band 3, or with an anti-EAAT3 monoclonal antibody. The cells were subsequently incubated with an anti–mouse antibody conjugated to the fluorescent dye Cy3 and analyzed by fluorescence microscopy.
Detection of EAAT3 using Western blot and indirect immunofluorescence. (A-B) Western blots of the membrane fraction of uninfected human erythrocytes. For panel A approximately 2 × 107 cells were lysed and the membrane fraction was separated on a 5%-15% SDS-PAGE. The separated membrane proteins were blotted onto nitrocellulose and probed with a monoclonal antibody against EAAT3 (left lane). Spectrin served as a loading control. Incubation of the blot with the secondary (rabbit anti–mouse) antibody alone gave no detectable bands (right lane). For panel B approximately 5 × 107 cells were lysed and the membrane fraction was separated on a 4%-12% SDS-PAGE. The gel was processed as described for panel A. (C) IFA images showing punctate staining of the membrane of both uninfected (RBC) and P falciparum–infected (iRBC) human erythrocytes by the anti-EAAT3 monoclonal antibody. Uninfected erythrocytes (left panel) and erythrocytes infected with trophozoite stage parasites (right panel) were fixed and incubated either without antibody, with the secondary antibody alone, with an antibody against human band 3, or with an anti-EAAT3 monoclonal antibody. The cells were subsequently incubated with an anti–mouse antibody conjugated to the fluorescent dye Cy3 and analyzed by fluorescence microscopy.
Indirect immunofluorescence assays using the antibody against EAAT3 revealed surface staining of normal uninfected erythrocytes, with the fluorescence pattern appearing more punctate than that observed using antiserum against band 3 (Figure 5C). A similar punctate staining was also observed for the surface of P falciparum–infected human erythrocytes (Figure 5C).
Activation of L-glutamate transport by alphaxalone and inhibition by cis-ACBD
A recent paper reports the activation of EAAT3 (expressed in Xenopus laevis oocytes) by alphaxalone, a neurosteroid anesthetic.39 As illustrated in Figure 6, treatment of human erythrocytes with alphaxalone (3μM for 10 minutes) induced a similar uptake of L-glutamate to that resulting from arsenite treatment.
Activation of glutamate uptake by alphaxalone and inhibition by cis-ACBD. Effect of the glutamate transport inhibitor cis-ACBD (100μM) on the uptake of L-[3H]-glutamate into uninfected human erythrocytes (black bars) treated with either 1mM arsenite (gray bars) or 3μM alphaxalone (white bars). Uptake was measured at 37°C for a period of 10 minutes. The data are averaged from 3 separate experiments performed on different days and are shown ± SEM.
Activation of glutamate uptake by alphaxalone and inhibition by cis-ACBD. Effect of the glutamate transport inhibitor cis-ACBD (100μM) on the uptake of L-[3H]-glutamate into uninfected human erythrocytes (black bars) treated with either 1mM arsenite (gray bars) or 3μM alphaxalone (white bars). Uptake was measured at 37°C for a period of 10 minutes. The data are averaged from 3 separate experiments performed on different days and are shown ± SEM.
Cis-ACBD (1-aminocyclobutane-1,3-dicarboxylate) is an L-glutamate analog that acts as an inhibitor of the transport of L-glutamate via members of the EAAT family.40 Cis-ACBD (100 μM) reduced the influx of L-glutamate into both arsenite-treated erythrocytes (P < .001; n = 3; paired t test) and alphaxalone-treated erythrocytes (P < .001; n = 3 paired t test; Figure 6). Furosemide also inhibited the uptake of L-glutamate into arsenite-treated erythrocytes (by 93 ± 3%; P < .001, n = 3, paired t test; data not shown).
Inhibition of the arsenite-induced influx of L-glutamate by cis-ACBD and by chymotrypsinization
In a previous study, it was demonstrated that the parasite-induced influx of some amino acids into P falciparum–infected erythrocytes is inhibited by treatment of the infected cells with the protease chymotrypsin, although remaining unaffected by trypsin.33 As shown in Figure 7A, the same was true of the arsenite-induced influx of L-glutamate into uninfected human erythrocytes. In cells treated first with arsenite, then subsequently treated with trypsin or chymotrypsin, chymotrypsinization reduced L-[3H]-glutamate transport by 78 ± 1% (± SEM; P < .001; n = 3; paired t test). By contrast, when the order of the treatments was reversed, with the cells first chymotrypsinized and then subsequently subjected to arsenite treatment, the arsenite-induced L-glutamate influx, although slightly (and not significantly; P > .05) reduced relative to that seen in nonchymotrypsinized cells, was significantly higher (P < .04; n = 3; paired t test) than that observed in cells that had been first treated with arsenite and then subjected to chymotrypsinization.
The effect of protease treatment on the uptake of L-[3H]-glutamate into arsenite-treated erythrocytes. (A) Uninfected human erythrocytes were incubated with 0.5 mg/mL trypsin or chymotrypsin for 30 minutes at 37°C either before (white bars) or after (gray bars) treatment with sodium arsenite. Cells treated with arsenite, but not with either protease, served as the control (black bars). After the treatments, the uptake of L-[3H]-glutamate was measured for 10 minutes at 37°C. L-[3H]-glutamate uptake is expressed in terms of a distribution ratio. (B) Erythrocytes were treated with sodium arsenite and an aliquot of the treated cells was taken for the purpose of measuring the uptake of L-[3H]-glutamate. The arsenite-treated cells cells were then treated with 0.5 mg/mL chymotrypsin for 30 minutes at 37°C and a second aliquot was taken for determining the uptake of L-[3H]-glutamate. The cells were then treated for a second time with arsenite, and an aliquot taken for the purpose of determining L-[3H]-glutamate uptake. They were then treated again with 0.5 mg/mL chymotrypsin and a further aliquot was taken for the determination of L-[3H]-glutamate uptake. A third and final treatment of the cells with arsenite was followed again by a determination of L-[3H]-glutamate uptake. All uptake measurements were made for 10 minutes at 37°C. L-[3H]-glutamate uptake is expressed in terms of a distribution ratio. All data were averaged from 3 independent experiments and are shown ± SEM.
The effect of protease treatment on the uptake of L-[3H]-glutamate into arsenite-treated erythrocytes. (A) Uninfected human erythrocytes were incubated with 0.5 mg/mL trypsin or chymotrypsin for 30 minutes at 37°C either before (white bars) or after (gray bars) treatment with sodium arsenite. Cells treated with arsenite, but not with either protease, served as the control (black bars). After the treatments, the uptake of L-[3H]-glutamate was measured for 10 minutes at 37°C. L-[3H]-glutamate uptake is expressed in terms of a distribution ratio. (B) Erythrocytes were treated with sodium arsenite and an aliquot of the treated cells was taken for the purpose of measuring the uptake of L-[3H]-glutamate. The arsenite-treated cells cells were then treated with 0.5 mg/mL chymotrypsin for 30 minutes at 37°C and a second aliquot was taken for determining the uptake of L-[3H]-glutamate. The cells were then treated for a second time with arsenite, and an aliquot taken for the purpose of determining L-[3H]-glutamate uptake. They were then treated again with 0.5 mg/mL chymotrypsin and a further aliquot was taken for the determination of L-[3H]-glutamate uptake. A third and final treatment of the cells with arsenite was followed again by a determination of L-[3H]-glutamate uptake. All uptake measurements were made for 10 minutes at 37°C. L-[3H]-glutamate uptake is expressed in terms of a distribution ratio. All data were averaged from 3 independent experiments and are shown ± SEM.
Trypsin-treatment had no significant effect on the arsenite induced influx of L-glutamate (P > .07; n = 3; paired t test), irrespective of whether the treatment was administered before or after exposure of the cells to arsenite (Figure 7A).
It was also shown in the previous study33 that after removal of chymotrypsin, uptake activity in P falciparum–infected erythrocytes was restored. Figure 7B shows the uptake of L-[3H]-glutamate into cells subjected to several rounds of arsenite-treatment followed by chymotrypsinization. In cells in which the arsenite-induced influx of L-[3H]-glutamate was reduced by chymotrypsinization, a second treatment with arsenite once again stimulated L-[3H]-glutamate influx (P < .001; n = 3; paired t test), albeit to a significantly lower level than that seen in the nonchymotrypsinized cells (P = .004; paired t test). A subsequent treatment of the cells with chymotrypsin once again reduced L-[3H]-glutamate influx. A third treatment with arsenite again stimulated L-[3H]-glutamate influx (P < .001; n = 3; paired t test), to a significantly lower level than was seen in response to the second arsenite treatment (P = .01; paired t test).
Discussion
Arsenite activates an EAAT in normal human erythrocytes
Although the mature human erythrocyte is known to have several amino acid transporters that mediate the influx and efflux of a range of different amino acids, it is not known to have a functional glutamate transporter, and glutamate is not transported to any significant extent across the membrane of normal human erythrocytes.36 This contrasts with the situation in canine erythrocytes, which have a functional Na+-dependent glutamate transporter.36,41 Novak et al42 reported the presence in rat erythrocytes of an EAAT, EAAC1 (which is the same protein as EAAT3); however, there was no evidence presented for the transporter being active.
In this study it was shown that treatment of human erythrocytes with arsenite activates a saturable, high-affinity, Na+-dependent glutamate transporter that is inhibited by the glutamate analog Cis-ACBD. The arsenite-treatment also induced the uptake of D-aspartate, but not that of either D-glutamate or L-alanine. These transport characteristics (high-affinity for L-glutamate, Na+-dependence, sensitivity to inhibition by Cis-ACBD, and permeability to L-glutamate and D-aspartate, but not to D-glutamate or L-alanine) are characteristic of members of the EAAT family of glutamate transporters. The function and physiologic roles of this class of transporters have been characterized in detail in epithelial cells and cells of the nervous system. They play a central role in the absorption of dietary anionic amino acids in the gut, in the reabsorption of anionic amino acids in the kidney proximal tubule, and in the uptake of anionic amino acids from the synaptic cleft after their release from glutamatergic neurons.29,30 What role, if any, an EAAT might have in the mature human erythrocyte, and whether, under what conditions, and by what mechanism it might be activated under physiologic conditions is not clear. Erythrocytes do not synthesize proteins; however, they do require a source of glutamate for the synthesis of the antioxidant tripeptide, glutathione, and it is possible that EAAT activation might play a role in the provision of glutamate under certain physiologic conditions. It is also possible that any EAAT present in the erythrocyte membrane plays a significant physiologic role in the (pre-erythrocytic) reticulocyte or earlier erythroid progenitor cells.
In this study Western blot analysis of erythrocyte membranes using antibodies against all 5 members of the EAAT family detected protein only in the case of EAAT3, and IFA analysis with this antibody, but not with antibodies to other EAAT members, revealed staining of the surface membrane of both uninfected and infected erythrocytes. Alphaxalone, shown previously to stimulate EAAT3 expressed in Xenopus laevis oocytes was shown to stimulate L-glutamate uptake in erythrocytes to the same extent as arsenite. On the basis of the results obtained here, EAAT3 is a candidate for the protein responsible for the high-affinity L-glutamate uptake transporter activated by arsenite treatment, although the possible involvement of other members of the family cannot be excluded.
How arsenite might induce the activation of the transporter remains to be established. The stimulation by arsenite of the Na+K+2Cl− cotransporter in ferret erythrocytes was postulated to be because of the stimulation of one or more kinases.26 Similarly, the stimulation of EAAT3 by alphaxalone in X laevis oocytes was attributed to a stimulation of protein kinase activity. The stimulation of L-glutamate uptake into human erythrocytes by arsenite (and alphaxalone) may be via a similar mechanism, though alternative explanations cannot be ruled out. For example arsenite-treatment is known to generate reactive oxygen species,43 and it is possible that this may play a role in its mode of action.
Chymotrypsinization of arsenite-treated cells resulted in the inhibition of the majority of the induced L-glutamate transport. In cells treated first with chymotrypsin, and then exposed to arsenite, the chymotrypsin had much less effect (Figure 7A). These data are consistent with the hypothesis that it is only when the transporter is in the active state that it is susceptible to inhibition by chymotrypsin. The finding that, in cells subjected to an initial round of arsenite-treatment, and then chymotrypsinization, a second arsenite treatment resulted in a significant increase in L-glutamate transport, and that after chymotrypsinization a third exposure to arsenite again resulted in increased L-glutamate transport, implies that the arsenite treatment activates only a fraction of the total pool of (normally quiescent) L-glutamate transporters present in the cell.
The uptake of L-glutamate into P falciparum–infected human erythrocytes
It has long been recognized that human erythrocytes infected with the malaria parasite, P falciparum, show increased permeability to a broad range of low molecular weight solutes, including L-glutamate.1,27,28 Much of the parasite-induced transport has been attributed to the presence in the parasitized erythrocyte membrane of broad-specificity (and low-affinity) anion-selective channels.3,16,18,44,45 A recent study provided evidence for the involvement of 2 parasite-encoded proteins in the formation of parasite-induced channels,24 and another proposed the involvement of an endogenous erythrocyte benzodiazopene receptor/voltage-dependent anion channel.20
As is clear from the data of Figure 4, the majority of the L-glutamate influx into P falciparum–infected human erythrocytes was via a low-affinity, Na+-independent and furosemide-sensitive pathway. The uptake of radiolabeled L-glutamate via this route was unaffected as the concentration of unlabeled L-glutamate was increased from the range 10 to 100μM. This pathway may be equated with the broad-specificity anion-selective channels induced by the parasite in the host cell membrane.45 However, as is also clear from Figure 4B and C, there is in addition to the low-affinity uptake component, one or more high-affinity components to the uptake of L-glutamate.
A significant part of the high-affinity uptake of L-glutamate by P falciparum–infected human erythrocytes was Na+-dependent; the magnitude of the saturable component of L-glutamate uptake was greater in cells suspended in Na+-containing medium than in cells suspended in a medium in which Na+ was replaced with choline. This raises the possibility that the Na+-glutamate transporter responsible for the uptake of L-glutamate into arsenite-treated erythrocytes is also active in the infected cells, providing a route for the high-affinity uptake of L-glutamate into the infected cell. Nevertheless the fact that there was a high-affinity L-glutamate uptake component observed in cells suspended in Na+-free media (in which the Na+-glutamate transporter cannot operate) indicates the contribution of at least one additional high-affinity process to the uptake of L-[3H]-glutamate measured for the 10 minute incubation period. Whether this reflects an additional high-affinity influx component, or perhaps a contribution of high affinity metabolic processes to the measured uptake of L-glutamate46 is not clear.
The question of whether, and if so how, the parasite might activate the same transporter that is activated by arsenite, and whether activation is via the same mechanism in both cases, perhaps involving the action of one or more protein kinases, is unclear. Egée and colleagues17 have presented evidence for the involvement of protein kinase A in the activation of anion channels in the plasma membrane of the parasitized erythrocyte,17,–19 raising the possibility that the same signaling mechanisms might play a role in the activation of an endogenous EAAT.
The physiologic significance of the possible activation by the parasite of a high-affinity glutamate transporter is also not clear. Glutamate is 1 of 5 amino acids originally identified as being essential (in the extracellular medium) to support the in vitro growth of P falciparum.47 However, subsequent analyses have revealed that parasites do grow well in medium containing isoleucine (and for some strains methionine) as the sole exogenous amino acid(s).48 This implies that the uptake of L-glutamate from the medium is not essential for parasite growth, at least under in vitro culture conditions. The observation that cultivation of parasitized erythrocytes in the presence of cis-ACBD does not compromise parasite growth is consistent with this (S. Bietz and K.L., unpublished data). Whether L-glutamate uptake plays a more important role under in vivo conditions is unknown.
In other cell types (eg, the cells of the nervous system) Na+-dependent glutamate transporters use the energy associated with the inward electrochemical Na+ gradient to mediate the uptake of L-glutamate against a large outward concentration gradient. In erythrocytes housing the mature asexual P falciparum trophozoite the concentration of Na+ in the erythrocyte cytosol is similar to that in the extracellular solution,4,49,,–52 and this in combination with the very low membrane potential across the infected erythrocyte membrane,52 means that an EAAT would have limited capacity to concentrate L-glutamate within the infected cell cytosol. Nevertheless, in the absence of a significant Na+ electrochemical gradient, such a transporter would still provide a high affinity (albeit nonconcentrative) route for the uptake of L-glutamate, as well as potentially contributing to the efflux of L-glutamate liberated via the degradation of hemoglobin within the parasite.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 USC section 1734.
Acknowledgments
The authors are grateful to the Canberra branch of the Australian Red Cross Blood Service for the provision of blood, and to Dr Simon Cobbold, Dr Jude Przyborski, and Dr Simone Külzer for helpful discussions.
This work was supported by grants to K.L. from the Deutsche Forschungsgemeinschaft (Li 402/11-2, Li 402/13-1), by a grant to K.K. from the Australian National Health and Medical Research Council (Project Grant No. 525428), and by grants to K.L. and K.K. from the Go8/DAAD Australia-Germany Joint Research Cooperation Scheme.
Authorship
Contribution: M.W. designed and performed experiments and analyzed data; E.R. performed experiments and analyzed data; S. Bietz and S. Baumeister performed experiments; and K.K. and K.L. supervised the study, analyzed data, and wrote the paper.
Conflict-of-interest disclosure: The authors declare no competing financial interests.
Correspondence: Klaus Lingelbach, Philipps-Universität Marburg, Faculty of Biology, Dept of Parasitology, 35043 Marburg, Germany; e-mail: lingelba@staff.uni-marburg.de; or Kiaran Kirk, The Australian National University, Research School of Biology, Canberra, 0200, Australia; e-mail: kiaran.kirk@anu.edu.au.

![Figure 1. Time courses for the uptake of different amino acids. The data are from uninfected human erythrocytes (▴), arsenite-treated uninfected human erythrocytes (○), and P falciparum–infected human erythrocytes (●). The influx of L-[3H]-glutamate (A), D-[3H]-aspartate (B), D-[3H]-glutamate (C), and L-[3H]-alanine (D) was measured for a period of 20 minutes at 37°C. The cells were suspended in (glucose-free) PBS and in each case the radiolabeled compounds were the only extracellular amino acids present. The extracellular concentrations were 20nM for L-glutamate, 78nM for D-aspartate, 21nM for D-glutamate, and 13nM for L-alanine. The uptake data are expressed in terms of a distribution ratio (ie, the estimated concentration of radiolabel inside the cell relative to that in the extracellular solution). The data were averaged from 5 separate experiments performed on different days, on erythrocytes from different donors, and are shown ± SEM.](https://ash.silverchair-cdn.com/ash/content_public/journal/blood/119/15/10.1182_blood-2011-10-386003/5/m_zh89991289450001.jpeg?Expires=1767709235&Signature=XvkrFkpPeGNrSWhjKm1cHxgs2Lc9lMVesegAbcV-Zh5zKg1hC3Bmd7dIQzHJy~F8PM-vxYhS0uJ2l2l2cwHZdTsmJLprMffhFavklLVPdael8fprp7ghL7P0xOywJIg2K-~p4yNRozxxjf1JLJfqlcVMvCpiBmQhBIgbiBVzhAurGmTgHXSQMDJ10d4ND~U-dvRfthrP5r614hGX9xsOjinyK5Cc2DdhbbRdpsCoRDQAhHnDPp30KAyfGTOVTCpSG9X~w-GF6nLqmWd7SHI1uMkEk~OQO1oDtK3loe7z8jyELboRl-BDO~KSoVy8vAZLhV93KxqQUcDeK3DX7rGJyA__&Key-Pair-Id=APKAIE5G5CRDK6RD3PGA)
![Figure 2. Sodium dependence of L-glutamate uptake. Time courses for the uptake of L-[3H]-glutamate into arsenite-treated (A) and P falciparum–infected (B) human erythrocytes (RBCs) in the presence or absence of extracellular Na+. The cells were suspended in a solution containing 20mM sucrose and 10mM Tris-HCl (pH 7.4) together with either 150mM sodium chloride (●) or 150mM choline chloride (○). The uptake data are expressed in terms of a distribution ratio (ie, the estimated concentration of radiolabel inside the cell relative to that in the extracellular solution). Symbols show data averaged from 5 independent experiments, ± SEM.](https://ash.silverchair-cdn.com/ash/content_public/journal/blood/119/15/10.1182_blood-2011-10-386003/5/m_zh89991289450002.jpeg?Expires=1767709235&Signature=vWt6Wp5VB9~hwu8VYFJKSxKtun7DdFvTCHwVPAtoOio2R81B8TN2gXMnJXkbtaRXa~aXkyw2CVZAmyJXyZmhWViz26h6PdXaG38ztG6~aDrvy-vtWdL98eculNjBbclskBJLRBT8x2RihUKz-mFw~L6ILMpaY8KxwcCSIZVtYG6gaapHg6LRpB-HbPiCY6mzi4Uy7DkZnFw09KnoK2yeknW~2YWFQYdUQ8lRElQFjJzGUnCjzgsuHoF~nfyy6pzwislZ-a4zdIqH-FAYXM3w4XQiA5tKlNWT3XG76TAuxCkHww7dMUBQZ5vQuNBlkMJwKGAuvMLKMXd5wh93KC8GUQ__&Key-Pair-Id=APKAIE5G5CRDK6RD3PGA)
![Figure 3. [Na+]-dependence of L-[3H]-glutamate into arsenite-treated (uninfected) human erythrocytes. The cells were suspended in a solution containing choline chloride + NaCl at a combined concentration of 150mM, together with 20mM sucrose and 10mM Tris-HCl (pH 7.4). Uptake of L-[3H]-glutamate was measured for 10 minutes at 37°C. The fitted line is a rectangular hyperbola (v = vmax [Na+]/(B + [Na+])) with B, the [Na+] at which uptake is half-maximal, 11.7 ± 1.8mM. The data were averaged from 5 independent experiments, ± SEM.](https://ash.silverchair-cdn.com/ash/content_public/journal/blood/119/15/10.1182_blood-2011-10-386003/5/m_zh89991289450003.jpeg?Expires=1767709235&Signature=JrlLwm~LFWSTfGeEb94XEIDXc6amEtnWwTI3SBuuuNNeUjV-hDajbYEniQbqra8HBB9ADrFFV8zEiMPQvAucW8HisQUl1CnjL64Tg5cPujViZY8HmHauZctrqm~cAY09E-YgywnUFlPZci68PcJ-j13k030-AdFAFzUIyo4fMyT~hdUvyr9MsSIYgZep5c9QhVZYZTI0Ggj7aT9hSrKDSYQx8SSRwuvdVJznN-yRs4otJsbYUhBuZWfFj6YRSc1zP62Pe5dCpAiS2azyo-OdVZqL30wkLlDbDvwHSSCMfzEd8xAjGdbaEgZH~Jepo0-4i3CM3tiuHVBlfj6-S438kQ__&Key-Pair-Id=APKAIE5G5CRDK6RD3PGA)
![Figure 4. Saturation of glutamate uptake. Effect of unlabeled L-glutamate on the uptake of L-[3H]-glutamate into (A) arsenite-treated uninfected human erythrocytes (RBCs) suspended in (glucose-free) PBS and (B-C) P falciparum–infected human erythrocytes suspended in the presence (B) and absence (C) of extracellular Na+ (with the extracellular solutions as described in Figure 2). In each case the uptake of L-[3H]-glutamate was measured for 10 minutes at 37°C, with the concentration of unlabeled L-glutamate in the extracellular solution ranging from 0 to 100μM. Uptake of L-[3H]-glutamate is expressed as a percentage of that measured in the absence of unlabeled L-glutamate in Na+-containing medium. The data are averaged from 3 independent experiments. (A) The inset shows the concentration-dependence of L-glutamate uptake, with the line drawn using the Michaelis-Menten equation (Km of 55 ± 9nM; Vmax of 17.2 ± 1.7 nmol/[1012 cells/hour]). The error bars indicate ± SEM. (B-C)The insets are Eadie-Hofstee plots of the data, which illustrate the fact that both in the presence (B) and absence (C) of extracellular Na+ there is one or more high-affinity component (dotted line) and 1 or more low-affinity component (dashed line) to the uptake of L-glutamate into P falciparum–infected erythrocytes. For clarity, the data are shown without error bars, with the exception of the inset in panel A.](https://ash.silverchair-cdn.com/ash/content_public/journal/blood/119/15/10.1182_blood-2011-10-386003/5/m_zh89991289450004.jpeg?Expires=1767709235&Signature=ZFYCk0iYcGJSoesTwpHTE0P2TaalgTbfmYLb2g0azeTw141Y2rbBixQNTPXpIzCb4WqWdXEqeThQwAtaffIVki0AdlBeR8ksn1qXGDvyOsiz0rOrkwmiVwn8YvvcnMaZ7ZtrjG1sfP-xlg4c7eibuql-e9bOkwqMsaDKdRAs5tdjnJmaiNoyJTb5fVwZOqZoY-vc698FuEJ6myWdz5GHF75TEyq-M5KiGitxbKvWmtADymXLEAnrZTsGED5NdI0Lr2YDunUf7HVx6bjAhiPkKP3hGj9V-M6--m2EAiUXUR3awMGOFG9ft6BTRsSGDLcFdWZ6PHridqBECa~6nHwFBg__&Key-Pair-Id=APKAIE5G5CRDK6RD3PGA)
![Figure 6. Activation of glutamate uptake by alphaxalone and inhibition by cis-ACBD. Effect of the glutamate transport inhibitor cis-ACBD (100μM) on the uptake of L-[3H]-glutamate into uninfected human erythrocytes (black bars) treated with either 1mM arsenite (gray bars) or 3μM alphaxalone (white bars). Uptake was measured at 37°C for a period of 10 minutes. The data are averaged from 3 separate experiments performed on different days and are shown ± SEM.](https://ash.silverchair-cdn.com/ash/content_public/journal/blood/119/15/10.1182_blood-2011-10-386003/5/m_zh89991289450006.jpeg?Expires=1767709235&Signature=0FtzyL9HHSI8R72OneiUg45u0e63nAXu1AXCc8YfXkF9oHQdEql5WYJRExd9wPzoyhwSSVzJr~5vsUXr2u5HhmWlEii1Vf2Idg7WmWtwkG64NbEx12mv4pvcJ9-ZqS3oh3N9O1mb8Qh1f9djz4UYKKAYik9MOXn4LmcBdHV5INHM47xe1xKVlmY~70KBUEd8mxZN0G1N-O-YMbhAa551hoA1~chwG1akWwHTKk7-56VhBwgokogc2OsUDlvymAeFKAoFXZeZhmi01LCVGwRR80wNkzfQQP~w2Y5NiZOFcK7I0euXpogcUdyXH1K3ZKhMex3xRyX1HA6LSzLbOxKhYA__&Key-Pair-Id=APKAIE5G5CRDK6RD3PGA)
![Figure 7. The effect of protease treatment on the uptake of L-[3H]-glutamate into arsenite-treated erythrocytes. (A) Uninfected human erythrocytes were incubated with 0.5 mg/mL trypsin or chymotrypsin for 30 minutes at 37°C either before (white bars) or after (gray bars) treatment with sodium arsenite. Cells treated with arsenite, but not with either protease, served as the control (black bars). After the treatments, the uptake of L-[3H]-glutamate was measured for 10 minutes at 37°C. L-[3H]-glutamate uptake is expressed in terms of a distribution ratio. (B) Erythrocytes were treated with sodium arsenite and an aliquot of the treated cells was taken for the purpose of measuring the uptake of L-[3H]-glutamate. The arsenite-treated cells cells were then treated with 0.5 mg/mL chymotrypsin for 30 minutes at 37°C and a second aliquot was taken for determining the uptake of L-[3H]-glutamate. The cells were then treated for a second time with arsenite, and an aliquot taken for the purpose of determining L-[3H]-glutamate uptake. They were then treated again with 0.5 mg/mL chymotrypsin and a further aliquot was taken for the determination of L-[3H]-glutamate uptake. A third and final treatment of the cells with arsenite was followed again by a determination of L-[3H]-glutamate uptake. All uptake measurements were made for 10 minutes at 37°C. L-[3H]-glutamate uptake is expressed in terms of a distribution ratio. All data were averaged from 3 independent experiments and are shown ± SEM.](https://ash.silverchair-cdn.com/ash/content_public/journal/blood/119/15/10.1182_blood-2011-10-386003/5/m_zh89991289450007.jpeg?Expires=1767709235&Signature=Jmz8KMKYpipI4-t4vLUoDU6SVgUojkBy~MCjdpDXFW4So4dfUerzBzqEJbWvCU1zL8GkuymIPqrE0EfKOvbY705IgNfRjRuZV9oKRW9TNDsx-kjJnaVq9vxBfrIxScP0tvQQcUNuVLgZVEGYdtUSDMAqMn~bydsvBfmoczW-o2qMrlU0Wtqzviy~xF9AQvpn4~4y~PP2RPLcWPoU7Te3P8MIAnptAU-~joaKzsb0AldTTt6C7e1v3~GTWm32bDLluDUuBcGb7lMSsap8kxe~eiv8ShgT8gbL4CZvrX12sEJWNt4gNAKv02CTqM8LpuX4XKOBLe9iEB1WUxuxYoKsrg__&Key-Pair-Id=APKAIE5G5CRDK6RD3PGA)