Abstract
Enhanced erythropoietic drive and iron deficiency both influence iron homeostasis through the suppression of the iron regulatory hormone hepcidin. Hypoxia also suppresses hepcidin through a mechanism that is unknown. We measured iron indices and plasma hepcidin levels in healthy volunteers during a 7-day sojourn to high altitude (4340 m above sea level), with and without prior intravenous iron loading. Without prior iron loading, a rapid reduction in plasma hepcidin was observed that was almost complete by the second day at altitude. This occurred before any index of iron availability had changed. Prior iron loading delayed the decrease in hepcidin until after the transferrin saturation, but not the ferritin concentration, had normalized. We conclude that hepcidin suppression by the hypoxia of high altitude is not driven by a reduction in iron stores.
Introduction
Dietary iron absorption was shown in the 1950s to be under the dual regulation of body iron stores and the prevailing rate of erythropoiesis, giving rise to the concept of the “store regulator” and the “erythroid regulator” in iron homeostasis.1,2 The downstream mediator of both regulators was later shown to be the iron-regulatory hormone hepcidin,3 which opposes iron absorption and recycling by binding and internalizing the cellular iron exporter ferroportin.4
The molecular mechanisms of hepcidin regulation are not completely understood. Oral iron loading stimulates hepcidin production in healthy humans.5,6 This may result in part from the binding of serum holotransferrin to transferrin receptor 1 in the liver, releasing the non-classical MHC class 1 molecule hereditary hemochromatosis protein (HFE) to interact with a holotransferrin-transferrin receptor 2 (TfR2) complex that up-regulates hepcidin expression.7-9 There is also evidence of a role for the membrane-bound protein hemojuvelin in the response to iron loading,5,10 and mutations in HFE, TfR2, or hemojuvelin can all cause hemochromatosis via inadequate hepcidin production.11 The signal linking erythropoiesis to hepcidin suppression remains unknown. Candidates include erythropoietin (EPO) itself, soluble transferrin receptor (sTfR), and growth differentiation factor-15 (GDF15), which is released by maturing erythroblasts and reduces hepcidin mRNA expression in cultured hepatocytes.12 Excessive serum GDF15 appears to underlie the paradoxical iron overload seen in patients with β-thalassemia.12
It is now known that hepcidin expression is also suppressed by hypoxia, but the mechanism is controversial. In mice, hypoxia-inducible factor was reported to regulate hepcidin expression via direct transcriptional suppression,13 but this finding has not been replicated in isolated hepatocytes.14 Hypoxia-inducible factor may, however, contribute to hepcidin suppression indirectly via effects on the breakdown of hemojuvelin.15,16
In vivo, hypoxia could also suppress hepcidin indirectly through erythropoiesis and enhanced iron use. Recently, a decrease in hepcidin was reported in healthy volunteers ascending gradually to high altitude.17 In this study, the authors observed a strong correlation between serum ferritin and hepcidin at each time point, and from this observation concluded that iron itself, or the kinetics of iron use in response to hypoxia, may be a signal for hepcidin down-regulation.
In the present study, we tested the hypothesis that the suppression of hepcidin by hypoxia arises through a reduction in iron availability. First, the changes in hepcidin and iron status on exposure to high altitude were examined at a greater temporal resolution than had been achieved in the previous report.17 Volunteers were transported from sea level to high altitude within an 8-hour period, and blood samples were taken daily during the first 3 days at high altitude. Secondly, a further group of volunteers underwent iron loading before travel to high altitude, to determine whether this would abrogate the reduction in hepcidin with hypoxia.
Methods
This study conformed to the principles of the Declaration of Helsinki and was approved by the Oxford Tropical Research Ethics Committee (Oxford, United Kingdom) and the Universidad Peruana Cayetano Heredia Research Ethics Committee (Lima, Peru). Participants provided written, informed consent.
Iron loading before ascent to high altitude
Twenty-four healthy male volunteers who lived at sea level (age 32 ± 10 years, mean ± SD) were recruited in Lima, Peru, where baseline (0 hours) blood tests were performed. On the morning of day 1, volunteers were randomized to receive an intravenous infusion of either iron(III) sucrose (200 mg in 100 mL over the course of 30 minutes; Vifor Inc) or saline placebo (100 mL over the course of 30 minutes). Within 2 hours of infusion, volunteers began the 8-hour ascent by road to Cerro de Pasco (4340 m). Blood tests were repeated on arrival, and on the mornings of days 2, 3, and 7.
Hematologic indices of iron homeostasis
At each time point, hematocrit was assessed by microcentrifugation. Serum for measurement of transferrin saturation and ferritin concentration was stored at 4°C and analyzed within 72 hours. Serum was stored at −20°C for erythropoietin ELISA (Medlab, Lima, Peru). Plasma was stored at −20°C for hepcidin ELISA (Bachem) and sTfR, GDF15, and IL-6 ELISA (R&D Systems). Hepcidin and IL-6 values for one volunteer at one time point (day7) were excluded from analysis because this volunteer developed a severe upper respiratory tract infection, which is known to enhance hepcidin expression.17,18
Statistical analysis
Contrasts between iron infusion and placebo were drawn by the use of repeated-measures ANOVA, unless otherwise indicated. Specific time points within and between groups were compared with the use of paired and unpaired Student t tests, respectively. Differences were considered significant if P < .05. Values are presented as mean ± SEM.
Results and discussion
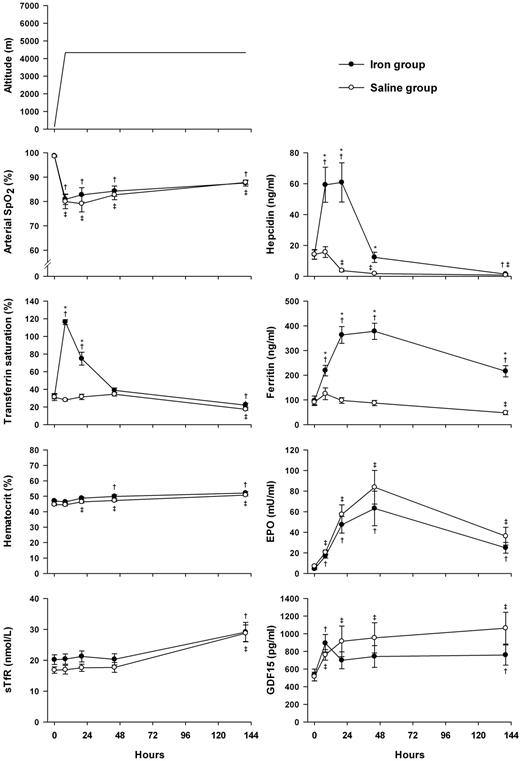
Baseline characteristics of volunteers in the iron and saline groups are summarized in Table 1. The groups were well-matched and all participants were iron-replete at baseline. Figure 1 shows that in volunteers given a placebo infusion before ascent, hepcidin decreased by the first morning at altitude (P < .01). This decrease occurred substantially (> 24 hours) before any change in transferrin saturation, serum ferritin concentration, or sTfR concentration, suggesting that it did not require the development of iron deficiency. The decrease in hepcidin was temporally associated with significant increases in EPO and GDF15 levels (P < .01 in each case), but further studies will be required to establish whether the association was causative in either case. Notably, there was no significant correlation between changes in hepcidin and those of GDF15 or EPO at any time point, and plasma levels of GDF15 were approximately 100-fold lower than those of patients with β-thalassemia, and 10-fold lower than those shown to suppress hepcidin in vitro.12 Plasma sTfR was stable for the first 48 hours at altitude, but elevated by day 7 (P < .01). This result is in keeping with the observation that sTfR is primarily an index of erythropoietic activity in iron-replete subjects.19,20
Baseline characteristics of study participants
| . | Iron group (n = 12) . | Saline group (n = 12) . |
|---|---|---|
| Age, y | 32 ± 11 | 33 ± 9 |
| Height, cm | 166 ± 4 | 166 ± 6 |
| Weight, kg | 73 ± 13 | 72 ± 9 |
| End-tidal PO2, mmHg | 104 ± 8 | 106 ± 4 |
| Arterial oxygen saturation, % | 99 ± 1 | 99 ± 1 |
| Hematocrit, % | 47 ± 2 | 45 ± 2 |
| Ferritin, ng/mL | 96 ± 69 | 90 ± 34 |
| Transferrin saturation, % | 32 ± 9 | 31 ± 14 |
| Hepcidin, ng/mL | 14 ± 11 | 14 ± 11 |
| Growth differentiation factor-15, pg/mL | 532 ± 230 | 515 ± 177 |
| Erythropoietin, mU/mL | 4.4 ± 1.9 | 7.0 ± 4.2 |
| Soluble transferrin receptor, nmol/L | 20 ± 5 | 17 ± 4 |
| . | Iron group (n = 12) . | Saline group (n = 12) . |
|---|---|---|
| Age, y | 32 ± 11 | 33 ± 9 |
| Height, cm | 166 ± 4 | 166 ± 6 |
| Weight, kg | 73 ± 13 | 72 ± 9 |
| End-tidal PO2, mmHg | 104 ± 8 | 106 ± 4 |
| Arterial oxygen saturation, % | 99 ± 1 | 99 ± 1 |
| Hematocrit, % | 47 ± 2 | 45 ± 2 |
| Ferritin, ng/mL | 96 ± 69 | 90 ± 34 |
| Transferrin saturation, % | 32 ± 9 | 31 ± 14 |
| Hepcidin, ng/mL | 14 ± 11 | 14 ± 11 |
| Growth differentiation factor-15, pg/mL | 532 ± 230 | 515 ± 177 |
| Erythropoietin, mU/mL | 4.4 ± 1.9 | 7.0 ± 4.2 |
| Soluble transferrin receptor, nmol/L | 20 ± 5 | 17 ± 4 |
Values are mean ± SD.
PO2 indicates partial pressure of oxygen.
Changes in arterial oxygen saturation (arterial SpO2, measured by pulse oximetry), hematologic markers of iron homeostasis, serum EPO, plasma sTfR, and GDF15 after a rapid ascent to high altitude. Baseline (0 hours) measurements were made in Lima, Peru (133 m above sea level), after which volunteers received an intravenous infusion of either 200 mg of iron sucrose (closed symbols, n = 12) or saline (open symbols, n = 12) and then ascended rapidly to high altitude (4340 m). *Significant difference between the change from baseline in the iron group, compared with the saline group (unpaired Student t test, P < .01). †,‡Significant change from baseline within the iron or saline group, respectively (paired Student t test, P < .05). Note that initial apparent “oversaturation” of transferrin (calculated transferrin saturation > 100%) can occur with intravenous administration of iron, reflecting the transient excess of serum iron. Symbols represent mean ± SEM.
Changes in arterial oxygen saturation (arterial SpO2, measured by pulse oximetry), hematologic markers of iron homeostasis, serum EPO, plasma sTfR, and GDF15 after a rapid ascent to high altitude. Baseline (0 hours) measurements were made in Lima, Peru (133 m above sea level), after which volunteers received an intravenous infusion of either 200 mg of iron sucrose (closed symbols, n = 12) or saline (open symbols, n = 12) and then ascended rapidly to high altitude (4340 m). *Significant difference between the change from baseline in the iron group, compared with the saline group (unpaired Student t test, P < .01). †,‡Significant change from baseline within the iron or saline group, respectively (paired Student t test, P < .05). Note that initial apparent “oversaturation” of transferrin (calculated transferrin saturation > 100%) can occur with intravenous administration of iron, reflecting the transient excess of serum iron. Symbols represent mean ± SEM.
Intravenous iron loading induced a rapid, but transient, increase in transferrin saturation together with a more gradual, but persistent, increase in serum ferritin. The variation in hepcidin over time appeared very similar to that for transferrin saturation, but it was dissociated from the variation in ferritin over time. Of note, plasma hepcidin concentration in the group that received iron was markedly suppressed by day 7, compared with baseline (P < .01), despite a mean ferritin > 200 ng/mL. Iron loading had no significant effect on EPO, sTfR, or GDF15 levels at altitude, compared with saline (P > .2).
Inflammation can induce hepcidin expression via IL-6 production.18,21 In the current study, plasma IL-6 was above the normal range for only 1 of 119 samples analyzed. The IL-6 concentration was below the lowest assay standard value in 79% of samples from volunteers receiving iron, and 69% of samples from those receiving saline (P > .2, χ2 test).
Taken together, these findings demonstrate that the suppression of hepcidin by hypoxia is too fast to be generated by a reduction in iron availability, suggesting that erythropoiesis and/or hypoxia per se are the major physiologic regulators in this setting. Iron loading can overcome the suppression of hepcidin by hypoxia during the period for which transferrin saturation remains elevated, but not during the entire period for which ferritin remains elevated. This finding is consistent with the notion that transferrin saturation is the major signal linking iron availability to hepcidin up-regulation,5,8,9 but intrahepatic iron has also been reported to enhance hepcidin expression directly.22,23 The latter phenomenon could explain the slightly higher hepcidin levels after 48 hours in the iron-loaded group, compared with the saline group, despite similar transferrin saturations.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 USC section 1734.
Acknowledgments
The authors thank the volunteers who took part in the study.
This research was supported by the Wellcome Trust and the Higher Education Funding Council for England.
Wellcome Trust
Authorship
Contribution: N.P.T., S.L., T.G.S., F.L.-V., K.L.D., D.R.M., and P.A.R. designed the research; N.P.T., S.L., T.G.S., C.P., A.H.N., and M.R.-C. performed experiments; and N.P.T., S.L., T.G.S., D.R.M., and P.A.R. analyzed and interpreted the data and wrote the paper.
Conflict-of-interest disclosure: The authors declare no competing financial interests.
Correspondence: Professor Peter Robbins, Department of Physiology, Anatomy & Genetics, University of Oxford, Oxford OX1 3PT, United Kingdom; e-mail: peter.robbins@dpag.ox.ac.uk.
References
Author notes
N.P.T., S.L., and T.G.S. contributed equally to this work.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal