Abstract
Abstract 1545
The diagnosis of peripheral T-cell lymphoma (PTCL) is difficult and accurate diagnosis and subclassification relies on correlating histologic, immunophenotypic, molecular genetic, and clinical data. Evidence-based guidelines for the appropriate diagnostic work-up of PTCL are lacking. The objective of this study was to evaluate a large series of PTCLs by experienced hematopathologists with a tiered approach to immunohistochemistry (IHC) and molecular genetic characterization to document overall diagnostic accuracy and clinical relevance using this approach.
7 experienced hematopathologists from 5 institutions reviewed 374 cases of peripheral T and NK cell lymphomas (referred to collectively as PTCL). 6 cases of cutaneous T-cell lymphoma were excluded after final review in addition to 29 non-PTCL cases submitted as control cases to mimic diagnostic practice during the review. Cases received tier 0, 1 and 2 diagnoses by 3 independent pathologists, based on review of hematoxylin and eosin (HE) stain with basic demographic data, panel 1 IHC (CD3, CD5, CD10, CD20, CD21, CD30, CD45, PAX5), and panel 2 IHC (CD2, CD4, CD7, CD8, CD23, PD1, CD56, EBER, ALK, TIA1, TCRg, TCRbF1), respectively. A tier 2b diagnosis was then rendered after gene rearrangement data were available. A final consensus diagnosis was rendered after discussion of each case by the 3 reviewers with all available clinical data. Overall survival (OS) was assessed using Kaplan-Meier (KM) curves and Cox proportional hazards models.
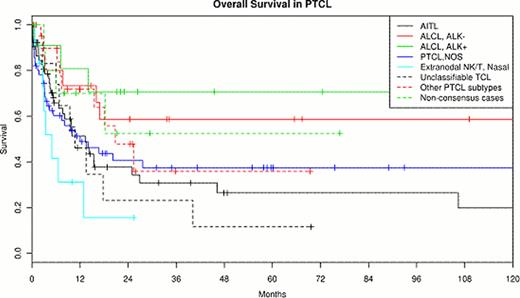
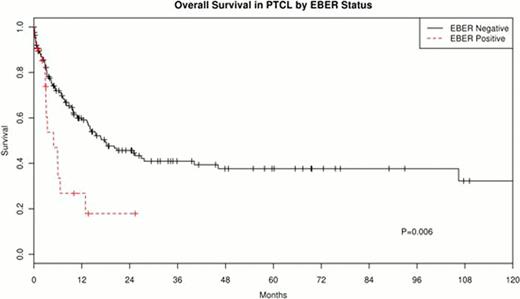
1122 individual diagnoses leading to 339 final consensus PTCL diagnoses were rendered. 341 (91%) cases had complete phenotypic data and 241 had gene rearrangement data. There was no bias of missing data according to final diagnosis subtype. Reviewer diagnoses using specific WHO subclassification were 16.3%, 36.9%, 82.7%, and 85.9% for tier 0, 1, 2, and 2b, demonstrating a significant increase in diagnostic certainty after a complete IHC panel. Gene rearrangement only contributed to a change in diagnosis in 51/650 (8%) individual reviews. Across all 374 cases, a small number of cases (n=28, 7.5%) showed no agreement among the 3 independent reviewers after tier 2b and required debate. These generally represented refinement of the subclassification of a PTCL. The most common disagreements were between PTCL, not otherwise specified (nos) vs. unclassifiable T-cell lymphoma, and PTCL, nos vs. angioimmunoblastic T-cell lymphoma (AITL). Currently, OS data was available in 198 cases and 52% have died (median age follow-up of 15 months for those still alive, range 0–160 mo). Figure 1 shows the KM survival curves for types with more than 10 cases. Of note, unclassifiable PTCL cases had poor OS, comparable to PTCL nos; a trend was seen for CD30+ ALK- ALCL to have a longer OS compared to PTCL nos (HR=0.5, 95% CI: 0.21–1.19, P=.09). EBER positivity in tumor cells was associated with poor OS in the cohort of all PTCL patients (HR=2.32, 95% CI: 1.28–4.23, p=0.006, Figure 2); the association was similar when nasal NK/T-cell lymphoma cases were excluded (HR=2.50, 95% CI: 1.00–6.26, p=0.05). Trends for poor prognosis were also seen for TIA-1 expression in PTCL, nos (HR=1.9, 95% CI 0.91–3.96, P=.09) and PD1 expression in AITL (HR=6.25, 95% CI 0.85–46.09, P=.07). Clinical data collection is still ongoing and will be updated.
We demonstrate the diagnostic accuracy among experienced hematopathologists of a defined IHC panel, showing an overall ability to reach consensus diagnosis of 93% in PTCL cases. The resulting consensus diagnostic subtypes showed expected outcomes relative to other large series of PTCLs, and EBER positivity is a poor prognostic marker among T and NK cell lymphomas. A tiered approach to IHC is recommended when a PTCL is under differential diagnostic consideration since the first tier can often resolve the main question of whether a lesion is reactive or lymphoma. This can lead to more efficient use of the expanded tier 2 panel that will enable diagnosis and specific subclassification of PTCL. Gene rearrangement studies are not required in the great majority of cases. This evidence-based approach to the diagnosis of PTCL should inform practicing pathologists, clinical trial design, and policy makers regarding required ancillary studies in this group of diseases.
Hsi:Allos: Research Funding. Said:Allos: Research Funding. Macon:Allos: Research Funding. Rodig:Allos: Research Funding. Gascoyne:Seattle Genetics: Research Funding. Ondrejka:Allos: Research Funding. Dorfman:Allos: Research Funding. Maurer:Allos: Research Funding. Dogan:Allos: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal