Abstract
Abstract 1995
The number of cord blood transplants (CBT) is rapidly increasing with suggestion of outcomes comparable to those obtained after unrelated donor transplantation (URD). We conducted, a retrospective analysis comparing post-transplant outcomes between myeloablative CBT and myeloablative URD at our Institution.
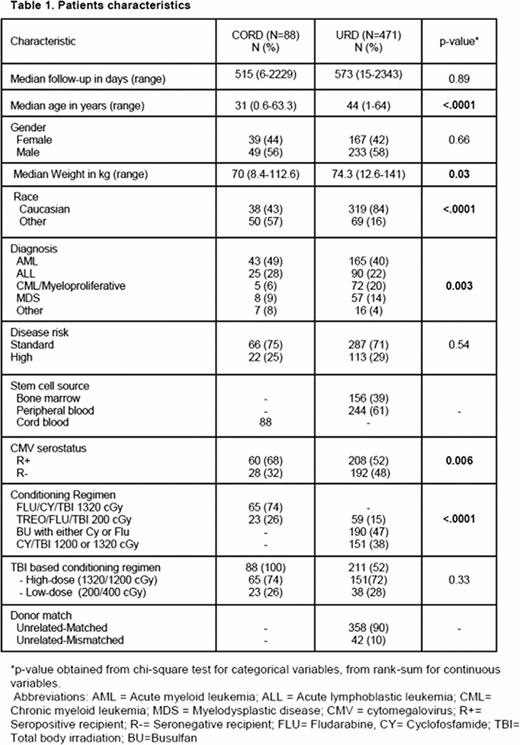
Between January 2006 and December 2011 a total of 488 patients received either a CBT (n=88) or URD (n=400). Of these 400, 358 (90%) received a 10/10 HLA-matched (MURD) and 42 (10%) a ≤9/10 HLA-mismatched (MMURD) graft. All patients received a double CB graft except for 12 patients (13%) who received a single CB unit. In addition, 25 (28%) patients received an ex vivo expanded graft as part of either a single or double CBT. Mycophenolate mofetil and cyclosporine were used for graft-versus-host disease (GVHD) prophylaxis in all CBT recipients, while FK506 + methotrexate was preferentially used among URD patients (n=339, 84%). Conditioning regimens for both groups are summarized in Table 1. Time-to-event outcomes were compared between groups using Cox regression, and logistic regression was used for acute GvHD. All models were adjusted for age, disease risk and CMV serostatus.
Patient characteristics are shown in Table 1. Differences between groups included higher median age in URD recipients and a higher proportion of non-caucasian and CMV seropositivity in CB recipients. Disease risk was similar between the 2 groups. Peripheral blood stem cells (PBSC) was used for the majority of URD grafts (61%). The median time to neutrophil [URD 19 days vs CBT 23 days; hazard ratio (HR) 1.91 (1.46–2.51, p<0.0001)] and platelet recovery [URD 19 days vs CBT 45 days; HR=2.76 (2.05–3.71, p<0.0001)] was significantly shorter for URD recipients. In multivariate analysis, the risk of mortality was similar in URD vs CBT (HR=1.11 (0.71–1.73, p=0.64)). When HLA-match status was considered in the URD group, the risk of death was higher in the MMURD group compared to CBT, although the difference was not statistically significant (HR=1.37 (0.83–2.26, p=0.22)). The risk of relapse was suggestively higher in the URD group overall relative to CBT (HR=1.90 (0.94–3.84, p=0.07)), and this difference was enhanced when HLA matching and source of stem cells in URD were considered. In particular, recipients of unrelated (matched or mismatched) PBSC had a higher risk of relapse relative to CBT (HR=2.33 (1.11–4.91, p=0.03)), as did the MMURD (BM or PBSC) group (HR=2.34 (1.07–5.11, p=0.03)). Furthermore, unrelated recipients of matched or mismatched PBSC each had a higher risk of relapse relative to CBT (matched PBSC: HR=2.44 (1.11–5.38, p=0.03); mismatched PBSC: HR=3.89 (1.63–9.30, p=0.002)). The combined results for mortality and relapse led to an increased risk of relapse-free survival (RFS) failure (earliest of relapse or death) for patients receiving PBSC from a mismatched URD (HR=1.88 (1.08–3.27, p=0.03)); the risk of failure was also increased for PBSC recipients from a matched URD, but the difference was not statistically significant (HR=1.42 (0.87–2.32, p=0.16)). The risk of non-relapse mortality (NRM) was similar between URD and CBT (HR=0.89 (0.52–1.53, p=0.67)), and while there was less chronic GvHD in the URD group, the difference was not statistically significant, and this slight reduction was largely due to the effect in BM recipients (URD BM vs CBT, HR=0.59 (0.35–0.98, p=0.04); URD PBSC vs CBT, HR=1.01 (0.62–1.66, p=0.95)). The risks of grades 2–4 and 3–4 acute GvHD were similar between URD and CBT groups (odds ratio (OR) 1.10 (0.57–2.11, p=0.78)), and (OR=0.70 (0.38–1.31, p=0.26)), respectively.
Our data suggest that OS, RFS and NRM after CBT are not inferior to those observed after URD transplantation, and OS and RFS might be higher when the URD group is restricted to recipients of PBSC, particularly those who are mismatched with their unrelated donor. Relapse occurred less frequently for CBT recipients especially when compared to MMURD or URD with PBSC. The retrospective nature of this study and the heterogeneity of the population do not allow us to draw definitive conclusions, however, our results reinforce the need for a randomized study to definitively address these comparisons.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal