Abstract
Abstract 217
The most widely used myeloablative preparative regimens for allogeneic hematopoietic cell transplantation (HCT) in myeloid malignancies consist of cyclophosphamide in combination with total body irradiation (Cy/TBI) or with orally or intravenously (IV) administered busulfan (BuCy). The relative advantages and shortcomings of these regimens have been debated for more than 25 years, but definitive conclusions regarding their comparative effectiveness and limitations are lacking.
Using data from the CIBMTR we retrospectively analyzed all patients who underwent first allo-HCT from a human leukocyte antigen (HLA)-matched sibling or adult unrelated donor from 2000 through 2006 for Chronic Myeloid Leukemia in first chronic phase or Acute Myeloid Leukemia (AML) in first complete remission following preparation with Cy/TBI or BuCy. Information regarding Bu pharmacokinetics was not collected during the period of study.
2284 patients aged 2 to 64 (median 34) years are included: 997 patients received Cy/TBI, 890 oral BuCy and 397 IV BuCy. In univariate analysis of the entire cohort, there were no significant differences in neutrophil recovery, chronic graft versus host disease (GVHD) or relapse between the groups. Platelet recovery occurred more rapidly (P=.002), grades 2–4 acute GVHD and transplant-related mortality (TRM) at 3 years were less frequent, and leukemia-free survival (LFS) and overall survival (OS) at 3 years were superior following IV or oral Bu compared to TBI (P<.001 for all comparisons).
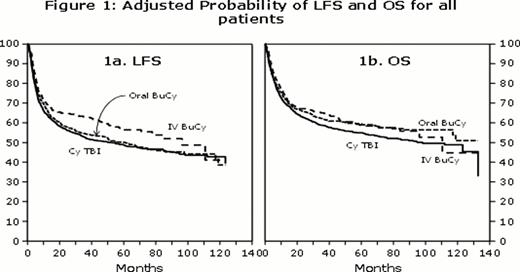
In multivariate analysis (adjusted for patient-related (age, gender, and Karnofsky performance score at transplant), disease-related (disease, time from diagnosis to transplant, and cytogenetic risk groups for AML), and HCT-related variables (donor-recipient gender and CMV match, donor and graft type, year of transplant, GVHD prophylaxis, and planned use of growth factors post-HCT)), the lower incidence of grades 2–4 acute GVHD with oral Bu vs. TBI (relative risk [RR] 0.85; 95% confidence intervals [CI] 0.73–0.99), and IV Bu vs. TBI (RR 0.76; 95% CI 0.64–0.91) remained significant. The incidences of chronic GVHD, TRM, and relapse within the first year post HCT did not differ between groups, however, relapse beyond the first year occurred significantly less frequently in those receiving IV(RR 0.39; 95% CI 0.21–0.73), but not oral Bu (RR 1.36; 95% CI 0.99–1.86) compared to TBI. OS was similar among the three groups. However, LFS was superior in patients receiving IV (RR 0.78; 95% CI 0.65–0.93), but not oral Bu (RR 0.97; 95% CI 0.84–1.12), compared to TBI (Figures 1).
Multivariate analysis (adjusted for same set of variables listed above) restricted to AML patients only (median age 35, range 2–64 years) revealed less TRM in those receiving oral (n=473; RR 0.75; 95% CI 0.57–0.98) or IV (n=272; RR 0.67; 95% CI 0.49–0.92) Bu compared to those receiving TBI (n=646). Relapse within first year post HCT did not differ between the groups, however, relapse beyond first year occurred significantly less frequently in patients receiving IV (RR 0.26; 95% CI 0.10–0.65), but not oral Bu (RR 1.26; 95% CI 0.84–1.90), compared to TBI. LFS was superior in AML patients receiving IV (RR 0.74; 95% CI 0.59–0.92), but not oral Bu (RR 0.88; 95% CI 0.74–1.06) compared to TBI. OS was superior among AML patients receiving oral (RR 0.80; 95% CI 0.67–0.97) or IV (RR 0.73; 95% CI 0.58–0.91) Bu compared to TBI. Survival was not significantly different between oral and IV Bu (RR 1.10; 95% CI 0.86–1.42) patients (Figures 2).
This large retrospective comparison of preparative regimens by the CIBMTR demonstrates a lower incidence of grades 2–4 acute GVHD in patients receiving Cy plus oral or IV Bu compared to TBI. Among the entire cohort, late relapses occurred less often and LFS was superior in patients receiving IV, but not oral Bu, compared with TBI.
Among nearly 1400 AML patients, there were fewer late relapses and LFS was superior following IV, but not oral, Bu compared to TBI. TRM occurred less frequently and survival was superior in patients receiving either oral or IV Bu compared to TBI. This large multi-institutional retrospective analysis demonstrates that in patients with AML in first CR, in combination with Cy, Bu is associated with a significantly lower incidence of TRM and superior survival than TBI.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.


This feature is available to Subscribers Only
Sign In or Create an Account Close Modal