Abstract
Abstract 2809
TP53 gene mutations, frequent in AML and MDS with complex karyotype, have recently been found in about 20% of lower risk MDS with del 5q, where they possibly conferred resistance to lenalidomide (LEN), and a higher risk of AML progression (Jadersten, JCO, 2011). We assessed the incidence and prognostic value of TP53 mutations in 79 lower risk MDS with del 5q, treated or not with LEN, and analysed in early disease phase or after progression to higher risk MDS or AML.
IPSS low and int 1 (Lower) risk MDS with del 5q were analysed at diagnosis or onset of LEN (“early phase”) and/or after progression to IPSS high or int 2 (higher) risk MDS or AML. LEN was administered at 5 or 10 mg/d during 16 weeks, and continued in erythroid responders until relapse or disease progression.
TP53 mutations were detected by the functional FASAY technique, assessing the transcriptional activity of p53 by co-transfecting an open gap repair plasmid with the product of amplification of TP53 from patients in yeasts whose growth is dependent on p53 functionality. The detection limit of this technique is around 10–15% (Flaman, PNAS 1995). Mutations found by FASAY were confirmed by direct sequencing, using Sanger method and /or (more recently) high sensitivity (1%) Next Generation Sequencing (NGS) by pyrosequencing (GS Junior System-Roche, with the IRON II plate design).
79 lower risk MDS with del 5q from 6 French centers of the GFM were analyzed, including 62 at diagnosis or onset of LEN (“early phase”), and 17 after progression to higher risk MDS or AML (5 of the latter were also retrospectively analysed on early phase samples).
Overall, 28 (35%) of the 79 patients had TP53 mutation, including 16 (26%) of the 62 pts analyzed at early phase and 12 (70%) of the 17 evaluated after higher risk MDS or AML progression (p= 0.001).
The 62 early phase pts had marrow blasts <5% and 5–9% in 91 and 9% of the cases, isolated del 5q, del 5q+1 and del5q+>1 (complex karyotype) in 84, 14 and 2% of the cases, and IPSS low and int 1 in 80 and 20% of the cases, respectively. No significant difference was found between mutated and non mutated cases for baseline characteristics including gender, age, WHO classification, cytogenetic complexity and IPSS. In the 5 pts analysed after progression where early phase samples were available, who all had received LEN, 4 had TP53 mutation at progression. In all of them, TP53 mutation was already detectable during early phase. However, the percentage of mutated colonies found by FASAY increased with progression, from 18 to 75%, 26 to 55%, 12 to 87% and 13 to 23%, respectively, showing an increase of the size of the mutated clone at progression.
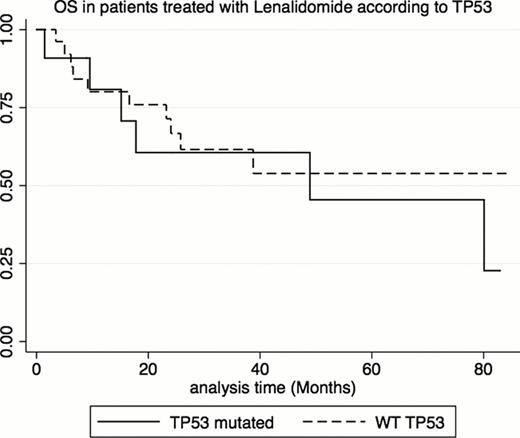
Among the 43 pts analyzed in early phase who received LEN (we excluded the 5 pts analysed after progression where early phase samples were available, to avoid bias), 36 (84 %) had isolated del 5q, 6 (14%) del 5q+1, and 1 (2%) had complex karyotype. IPSS was low in 73% and int-1 in 27%. 12/43 (28%) had TP53 mutation. 63% of the 43 pts achieved erythroid response, and 9 (47%) of the 19 pts evaluable at erythroid response achieved cytogenetic response. Erythroid response was seen in 45% mutated vs 71% non mutated cases (p= 0.258). Cytogenetic response was seen in 1/8(12%) mutated vs 8/11 (73%) non mutated cases (p=0.020). In those 43 pts who received LEN, the cumulative incidence (CI) of AML evolution, with death as a competitive event, did not significantly differ between patients with or without TP53 mutation (3 year CI of 35% vs 30%, p=0.33). Finally, in those pts, TP53 mutational status had no significant impact on OS (median 49 months in mutated pts vs not reached in non mutated pts, p=0.48, figure 1).
We confirm the presence of TP53 mutations in about 25 % of lower risk MDS with del 5q analysed in early disease phase. TP53 mutations, in those patients, were not correlated with other baseline parameters. When treated with LEN, mutated cases had similar hematological response, lower cytogenetic response but no significant difference in progression to higher risk MDS or AML and survival compared to non mutated cases. The high incidence of TP 53 mutations at progression to higher risk MDS/AML (70%), and the increase in the TP53 mutated clone size observed during progression in pts with a baseline mutation support the pathophysiological importance of TP53 mutations in disease progression in lower risk MDS with del 5q.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal