Abstract
Abstract 2970
Evaluating real life outcomes in Multiple Myeloma (MM) pts in order to understand treatment outcome in clinical practice is very important. The introduction of novel agents (Bortezomib, Thalidomide, Lenalidomide) has been shown to increase overall survival (OS). Can MM be regarded as a chronic disease, defined as a similar OS as a matched normal population at diagnosis, after the introduction of novel agents?
All pts diagnosed with MM since earliest Jan 2000 until latest Jun 2011 from 6 university clinics, 3 regional centers and 4 local hospitals in Sweden were included. Near complete response (nCR) was defined as an immeasurable M-protein in the blood and urine by standard electrophoresis. Partial response (PR) was defined as a 50% reduction in M-protein, no response (NR) as less than 50% reduction and progress was considered when the increase was ≥ 25%. The Swedish population (n = 9 340 682 in 2009) was used to select a gender and 5-yrs age strata matched cohort based on 2008–2010 observed death rates.
In the total MM population n=1 843, 201 (11%) pts were excluded due to non treatment demanding disease setting the study population to n=1 642. The median follow up of pts still alive was 30 months. The median age was 70 yrs and 45% women. The most common subtype was IgG (59%) followed by IgA (22%), BJ (15%) and Other (4%). High dose treatment (HDT) was given to 517 (32%) pts. The median number of given treatment lines in both the HDT and the non-HDT population was two but the number of pts receiving more treatment lines were declining rapidly.
The response distribution for the HDT population nCR/PR/NR was 47/41/12% in 1st line (induction and high-dose melphalan) and 25/42/33% in 2nd line. In the non-HDT population the response distribution was 14/42/44% in 1st line and 11/31/58% in 2nd line. Non-HDT pts receiving novel agents in 1st line had significantly higher nCR rates compared to pts receiving older drugs, 22% vs. 12% as well as pts receiving novel agents in 2nd line with nCR rates of 16% vs. 6%.
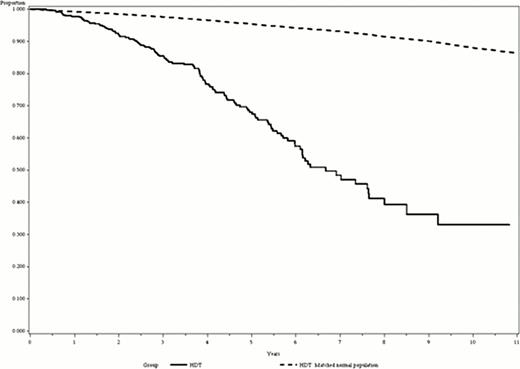
In the HDT population the median time to progression/time to next treatment (TTP/TTNT) was 21.0/29.7 months in 1st line and 8.1/12.7 in 2nd line. In the non-HDT population the median TTP/TTNT was 11.0/16.8 months in 1st line and 7.3/11.4 in 2nd line. There was a significantly increased TTP/TTNT in 1st and 2nd line depending on the increased depth of the response for both the HDT and non-HDT populations. The median OS for HDT pts was 6.7 yrs 95% CI[6.1;7.6] and correlated with 1st line response (nCR 7.6, PR 6.1 and NR 6.2 yrs). When comparing HDT pts to the matched normal population the 1-year survival was 97% vs. 99%, 3-year survival 86% vs. 98% and 5-year survival 66% vs. 95%.
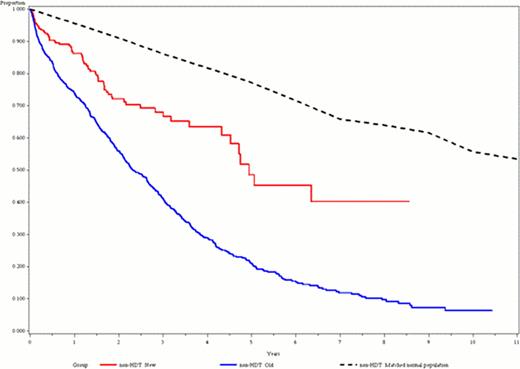
The median OS for non-HDT pts (n=1080) was 2.7 yrs 95% CI[2.5;3.0] and increased with better response in 1st line; nCR 3.4, PR 3.0 and NR 1.9 yrs. Kaplan-Mayer analysis showed that the use of novel agents in 1st line (n=316, median age 72.1 yrs) predicted a significantly longer OS compared to conventional treatment (n=764, median age 75.4), median 4.9 vs 2.3 yrs. When comparing pts that received at least two lines of treatment, pts treated with novel agents in 1st line followed by novel agents in 2nd had not reached the median survival but had a lower CI of 6.3 yrs, novel agents in 1st line followed by old agents in 2nd line had a median OS of 4.3 yrs old agents in 1st line followed by novel agents in 2nd line had a median of OS 3.3 yrs and old agents in 1st line followed by old agents in 2nd line had a median of OS 3.0 yrs. Compared to the matched normal population non-HDT pts receiving novel agents in both 1st and 2nd line the 1-year survival was 90 % vs. 96%, 3-year survival 71% vs. 86% and 5-year survival 67% vs. 77%.
The number of pts receiving 2nd and 3rd line treatment declined rapidly. Non-HDT pts treated with novel agents in 1st line had a superior response and OS compared to the group treated with standard chemotherapy. Pts treated with novel agents in 2nd line as well seem to have a further improved survival compared to other alternatives. In comparison to a normal population, matched for gender and age at diagnosis, the survival is still shorter. However, if novel agents were used in an optimal treatment sequence the survival could potentially be higher. There is still a need for further development in MM treatment before one can call it a chronic disease.
Non-HDT pts receiving old or novel agents in 1st line compared to a matched normal population.
Non-HDT pts receiving old or novel agents in 1st line compared to a matched normal population.
Liwing:Janssen-Cilag: Employment, Equity Ownership. Mellqvist:Janssen, Celgene: Honoraria. Näsman:Janssen-Cilag: Consultancy. Aschan:Janssen-Cilag: Employment, Equity Ownership.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal