Abstract
Abstract 3271
Hemophagocytic Lymphohistiocytosis (HLH) is a rare and potentially life-threatening disorder in adults. Patients (pts) with fever of unknown origin, lymphadenopathy, deteriorating performance status, encephalopathy and elevated systemic inflammatory parameters frequently show no clear cut diagnostic criteria specific for HLH. Among adults, late onset of inherited HLH is possible, but acquired HLH triggered by infection, neoplasia or autoimmune disease is more frequent than in pediatrics. Due to the variability of clinical presentation, large-scale unreporting can be assumed. We therefore commenced a German registry for HLH pts, aiming to sensitize clinicians and to establish an HLH network as starting point for research and clinical guideline activities.
We performed a retrospective multicenter case study in Germany. Diagnostic criteria were derived from the pediatric revised HLH-04 protocol. Treatment and outcome parameters were evaluated.
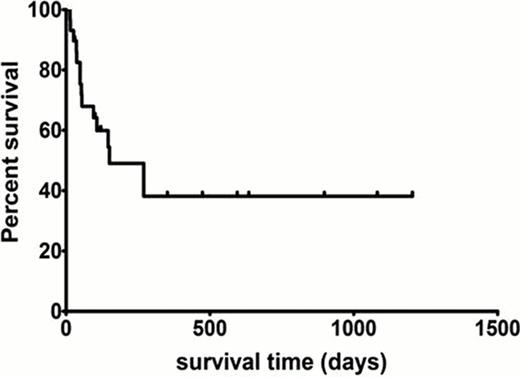
In 29 adult pts registered so far, median age was 46 years (18–81), 13 pts were female. HLH in 10 pts (34%) was malignancy-associated (aggressive B-cell lymphoma, n=6; B-CLL n=1; AML n=2; melanoma n=1), infection-associated (IHLH) in 13 pts (45%), 2 pts (7%) had connective tissue disease (CTD), in 1 pt HLH developed after therapeutic plasma exchange for TTP and in 3 pts (10%) the cause could not be determined. The main pathogen in IHLH pts was EBV (9/29, 31%) followed by other viruses (CMV n=1; HSV n=1; VZV n=1; Parvovirus B19 n=1). Of the 13 IHLH pts, 4 pts showed an EBV-reactivation post-allogeneic stem cell transplantation (SCT) for acute leukemia (n=3) and severe aplastic anemia (n=1) and 1 pt a systemic VZV infection after autologous peripheral blood SCT for aggressive B-cell NHL. 2 pts showed an EBV- and a lymphoma-triggered HLH respectively during late pregnancy. In 2 pts with EBV-associated HLH sequencing revealed mutations in XIAP and XLP-1 genes. The median time from onset of symptoms to diagnosis was 14 days (range 1–60 days). Most pts received polyvalent immunoglobulin (20/29, 69%) and HLH-04 based therapy, including steroids (14/29, 48%), cyclosporine (6/29, 21%), and etoposide (10/29, 34%). 5 pts (17%) received rituximab and 3 pts (10%) R-CHOP for lymphoma. 2 pts each (7%) received alemtuzumab and cyclophosphamide. One patient underwent allogeneic SCT but died. With a median follow up of 413 days (range, 54–1204 days), 12 pts (41.3%) survived. 2 pts were lost to follow-up. Median survival after diagnosis was 151 days (range, 14–1204+ days).
Adult pts with HLH in our cohort showed a heterogeneous clinical syndrome most frequently triggered by EBV. HLH represents a final common pathway of an aberrantly activated immune system responding to a variety of triggers. If not recognized and treated early, HLH in adults has a very poor prognosis. Clinical registries need to include adult HLH pts in order to facilitate basic and clinical research to improve outcome of this frequently fatal immune response syndrome.
Clinical and laboratory findings in adult HLH pts (n = 29)
| . | N(%) . | Median . | Range . |
|---|---|---|---|
| Clinical findings . | . | . | . |
| Fever | 29 (100.0) | – | – |
| Splenomegaly | 23/27 (85.2) | – | – |
| Neurological abnormalities | 4 (15.3) | – | – |
| Laboratory findings | |||
| Hemoglobin (g/dL; RR 12.0–15.7) | 29 (100) | 7.8 | 6.6–13.8 |
| Platelet count (/nl; RR 150–350) | 29 (100) | 32 | 9–245 |
| Neutrophil count (/nl; RR 1.8–7.7) | 29 (100) | 1.3 | 0.08–11.6 |
| Triglycerides (mmol/L; RR 0.83–2.3) | 25 (86.2) | 5.31 | 2.24–14.4 |
| Fibrinogen (g/L; RR 1.8–3.5) | 29 (100) | 1.6 | 0.13–3.8 |
| Ferritin (μg/L; RR 13–150) | 29 (100) | 45,553 | 479–523,673 |
| Ferritin >10,000 μg/L | 23 (79.3) | – | – |
| sIL2-R (U/ml; RR <1000) | 20 (68.9) | 6,791 | 1,194–24,032 |
| Low NK-cell count (FACS) | 11/18 (61%) | – | – |
| Morphologically proven hemophagocytosis | 19 (65.5) | – | – |
| . | N(%) . | Median . | Range . |
|---|---|---|---|
| Clinical findings . | . | . | . |
| Fever | 29 (100.0) | – | – |
| Splenomegaly | 23/27 (85.2) | – | – |
| Neurological abnormalities | 4 (15.3) | – | – |
| Laboratory findings | |||
| Hemoglobin (g/dL; RR 12.0–15.7) | 29 (100) | 7.8 | 6.6–13.8 |
| Platelet count (/nl; RR 150–350) | 29 (100) | 32 | 9–245 |
| Neutrophil count (/nl; RR 1.8–7.7) | 29 (100) | 1.3 | 0.08–11.6 |
| Triglycerides (mmol/L; RR 0.83–2.3) | 25 (86.2) | 5.31 | 2.24–14.4 |
| Fibrinogen (g/L; RR 1.8–3.5) | 29 (100) | 1.6 | 0.13–3.8 |
| Ferritin (μg/L; RR 13–150) | 29 (100) | 45,553 | 479–523,673 |
| Ferritin >10,000 μg/L | 23 (79.3) | – | – |
| sIL2-R (U/ml; RR <1000) | 20 (68.9) | 6,791 | 1,194–24,032 |
| Low NK-cell count (FACS) | 11/18 (61%) | – | – |
| Morphologically proven hemophagocytosis | 19 (65.5) | – | – |
RR, reference range; sIL2-R, soluble interleukin-2 receptor.
Overall survival of adult HLH pts (n=29)
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal