Abstract
Abstract 4184
Chronic graft-versus-host disease (cGVHD) risk score by Arora et al (Blood 2011) was successfully demonstrated to stratify patients with cGVHD according to their transplantation outcomes. In this risk score model, the following variables were included: recipient age, donor type, sex mismatch, GVHD prophylaxis, prior acute GVHD, time from HSCT to cGVHD, disease status before HSCT, platelet count at cGVHD diagnosis, serum bilirubin at cGVHD onset and performance status at diagnosis of cGVHD. However, this risk score system needs to be validated in an independent cohort.
A total of 425 consecutive patients who survived beyond 100 days following allogeneic hematopoietic stem cell transplantation (HSCT) at the Princess Margaret Hospital from Jan 1996 to Oct 2007, were reviewed retrospectively and evaluated for the cGVHD risk score[J1].
Out of 425 patients, 317 patients developed cGVHD according to the NIH consensus criteria of GVHD. Ten patients were removed from the analysis due to missing variables. Long-term transplant outcomes of the remaining 307 patients were evaluated using the cGVHD risk score system. First, overall survival (OS) according to the risk group (RG) were 82.5±11.3 (RG1), 76.4±3.4 (RG2), 69.4±6.5 (RG3), and 27.3±13.4 (RG4) (p<0.001), while non-relapse mortality (NRM) were 10.0±9.5 (RG1), 10.4±2.4 (RG2), 21.4±5.8 (RG3), and 69.3±14.7 (RG4) (p<0.001). Significantly lower OS and higher NRM was noted in RG4. However, there is no statistical difference of the transplant outcomes among 3 groups of RG1, RG2 and RG3 for OS and NRM.
Next, in order to improve a stratification power of cGVHD risk score model, two other clinical variables were incorporated into the model, absolute lymphocyte count (ALC) and eosinophil count (EOS) at the onset of cGVHD. The patients with lower (ALC, <1.0·109/L) and lower eosinophil counts (EOS, <0.5·109/L) at the onset of cGVHD were associated with inferior OS and higher risk of NRM. In a multivariate analysis, lower ALC was confirmed to be an independent variable predicting OS (HR 1.94, 95% CI 1.14–3.28, p=0.014) and NRM (HR 2.87, 95% CI 1.35–6.08, p=0.006). Similarly, EOS was also confirmed to be an independent variable predicting OS (HR 3.27, 95% CI 1.28–8.38, p=0.014).
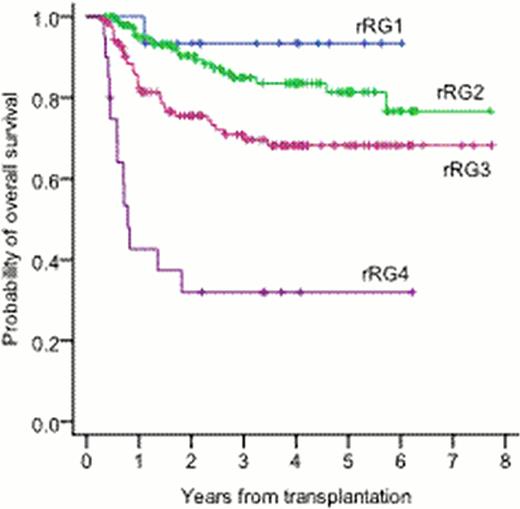
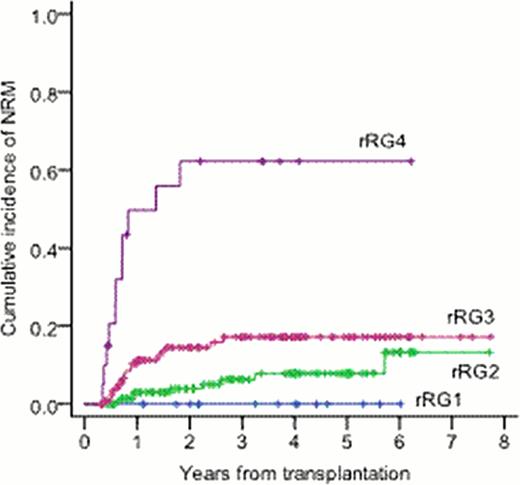
Accordingly, these two variables (i.e. ALC and EOS) were tested in a revised cGVHD risk score model and patients were stratified into revised 4 groups: rRG1 (score 0–3), rRG2 (score 4–6), rRG3 (score 7–9), rRG4 (score °Ã10). Overall survival (OS) according to the revised risk group (rRG) were 93.3±6.4 (rRG1), 81.4±4.1 (rRG2), 68.2±4.6 (rRG3), and 32.0±1.7 (rRG4) (p<0.001). Non-relapse mortality (NRM) were 0.0 (rRG1), 7.9±2.8 (rRG2), 17.2±3.8 (rRG3), and 62.2±11.8 (rRG4) (p<0.001). The revised cGVHD-risk score appears to better discriminatepatients according to their transplant outcomes (particularly OS and NRM).
The original cGVHD risk score model has been successfully validated to stratify transplant patients according to their risk of cGVHD[J2]. In addition, revised cGVHD risk score model including ALC and EOS at cGVHD onset improved prognostic stratification of the patients according to their transplantation outcomes.
Five-year overall survival and NRM by Revised cGVHD risk score including ALC and Eosinophil counts at cGVHD onset
Five-year overall survival and NRM by Revised cGVHD risk score including ALC and Eosinophil counts at cGVHD onset
| Revised risk group . | Overall risk score . | No pts (%) . | OS (%,± SE) . | NRM (%,± SEM) . |
|---|---|---|---|---|
| rRG1 | 0-3 | 15 (4.9) | 93.3 ± 6.4 | 0.0 |
| rRG2 | 4-6 | 145 (47.2) | 81.4 ± 4.1 | 7.9 ± 2.8 |
| rRG3 | 7-9 | 127 (41.4) | 68.2 ± 4.6 | 17.2 ± 3.8 |
| rRG4 | °Ã10 | 20 (6.5) | 32.0 ± 10.7 | 62.2 ± 11.8 |
| Revised risk group . | Overall risk score . | No pts (%) . | OS (%,± SE) . | NRM (%,± SEM) . |
|---|---|---|---|---|
| rRG1 | 0-3 | 15 (4.9) | 93.3 ± 6.4 | 0.0 |
| rRG2 | 4-6 | 145 (47.2) | 81.4 ± 4.1 | 7.9 ± 2.8 |
| rRG3 | 7-9 | 127 (41.4) | 68.2 ± 4.6 | 17.2 ± 3.8 |
| rRG4 | °Ã10 | 20 (6.5) | 32.0 ± 10.7 | 62.2 ± 11.8 |
Abbreviations: RG, risk group, OS, overall survival, NRM, non-relapse mortality.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal