Abstract
Abstract 4521
Continuity of care (COC) is acknowledged as a core quality measure in HIV, heart failure and family medicine. Allogeneic hematopoietic stem cell transplantation (Allo-HCT) is complex therapeutic option where is the selection of patient, donor, conditioning and immune-suppression plays a pivotal role in overall survival (OS) outcome. Although the team concept is an integral part of care in Allo-HCT, there is little literature known about the impact of personnel COC (care from the same provider) on OS.
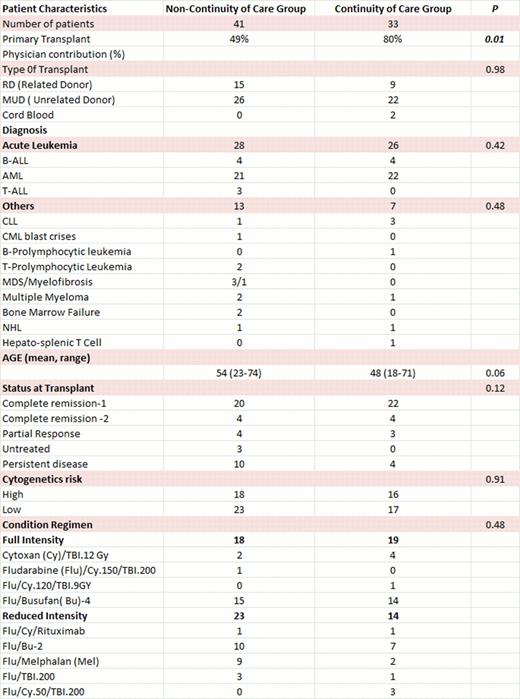
Between July 2009 and May 2012, 74 consecutive Allo-HCT were performed at our center. The patient's clinical care for the first consecutive 41 patients was shared between the physicians independent of primary transplant physician (Non- COC group). To assess the impact of COC on OS after Allo-HCT, the subsequent 33 patients (COC group) were followed by their transplant physician both as in-patient and outpatient. Physician's contribution into the care of each individual patient was calculated from physicians billing visits. Patient characteristics of COC & Non-COC groups are shown in table I. Graft vs. host disease (GVHD) prophylaxis was Tacrolimus/MTX or Cyclosporine/Mycophenolate with the addition of Thymoglobulin for MUD and mismatched RD.
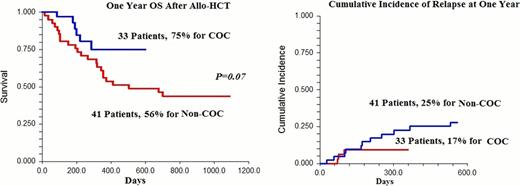
The average contribution of the primary transplant physician into their patients care during year one post-transplant was 49% vs. 80% for Non-COC and COC groups respectively (P=0.01). There was no difference in patient characteristics between COC and Non-COC groups except for older patients in Non-COC. With median duration of follow up of 815 days for Non-COC and 320 days for COC groups, the 1- year OS was 56% vs. 75% respectively (P=0.07). Similarly, there was a trend toward improved DFS for COC (1-year DFS of 68% vs. 48%, P=0.11). On Univariate analysis, Age (≤ 55, P=0.26), Donor source (MUD vs. RD, p=0.65), diagnosis (acute leukemia vs. other, p=0.18), status at transplant (P= 0.23), cytogenetic risk (p=0.79) and conditioning (FIC vs. RIC, p=0.62) were not predictive of improved OS. Both cumulative incidence of relapse and treatment related mortality (TRM) at 1-year were lower in COC compared to Non-COC groups; 9.5% vs. 25% and 17% vs. 25% respectively. The cumulative incidence of grade II –IV acute GVHD (aGVHD) at day 100 and day 180 was 64% & 64% for Non-COC vs. 46% & 72% for COC respectively. There was more patients with grade III/IV aGVHD; 13/41 (32%) in Non-COC compared to 6/33(18%) in COC, however this difference was not statistically significant (p=0.27). Additionally, there was no difference in OS in patients with grade III/IV aGVHD in Non-COC (13 patients) vs. COC (6 patients), P=0.85. In contrast, Patients without grade III/IV aGVHD had a statistical OS advantage in favor of COC (27 patients) vs. Non-COC (28 patients) with one year OS of 90% vs. 68% respectively, P=0.05. Cumulative incidence of chronic GVHD at one year was 77% for COC and 48% for Non-COC patients, P=0.02.
Physician-Patient continuity of care may favorably impact OS in Allo-HCT for hematological malignancy. The reason for lower relapse and TRM in COC group is unclear but could be attributed to older patients and differences in aGVHD management in Non-COC group. In this small study, COC did not impact OS in patients with severe aGVHD but may result in OS advantage in Allo-HCT patients without grade III/IV aGVHD. Larger studies are needed to address the impact of COC on outcomes after Allo-HCT.
Khaled:Celgene and Takeda Pharmacutical: Honoraria, Speakers Bureau. Solh:Celgene: Speakers Bureau.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal