Abstract
Abstract 587
In allogeneic stem cell transplantation, the donor-recipient gender combination plays a role in outcome. In large retrospective registry studies, acute and chronic graft–versus -host-disease (GVHD) were more frequent and treatment related mortality (TRM) higher in male recipients with a female donor than in other donor-recipient gender combinations. These were attributed to female donor T cells specific for male minor histocompatibility antigens encoded by Y-chromosome genes. We speculated that quantitative rather than qualitative cell composition differences between grafts harvested from male and female donors may have a role in the difference in patients' outcome.
We investigated the CD34 and CD3 cell composition of grafts derived from G-CSF mobilized peripheral blood grafts (male donors, n=408, female donors, n=217) and their relation to various transplantation outcomes in 641 allogeneic transplantation recipients from three tertiary medical centers between the years 2001 and 2012. The median age of this cohort was 52 years (range, 17–76); 44% were in CR/PR at transplantation. The donor was an HLA-matched sibling in 57% and 4% had a 1 allele mismatched donor. Cord blood and haplo-identical transplantations were not included in the analysis. Myeloablative conditioning was used in 59% of the transplants. CD34 and CD3 graft composition were measured by multicolor flow cytometry analyses and expressed as infused cells/kg of actual recipient weight. Cox regression analysis was used to model the impact of CD34 and CD3 levels on time-to-event endpoints. CD34 and CD3 doses were divided according to quartiles.
Male and female donor grafts differed significantly in CD34 and CD3 cell content. Compared with male donors, grafts derived from females had a higher mean CD3/kg cell content (4.0 ±1.9*108 vs. 3.3±1.6*108, p<0.001), a lower mean CD34/kg cell content (6.9±2.3*106 vs. 8.1±2.3*106, p<0.001) and a higher CD3/CD34 ratio (66.8 ±47.9 vs. 45.7±30.5, p<0.001).
Univariate analysis for grade 2–4 acute GVHD identified female donor to male recipient, unrelated donor and allele mismatch as factors associated with a higher risk for GVHD. However when adjusted to CD3 dose, only grafts derived from unrelated donors (p=.04) and allele mismatch (p=.006) remained statistically significant.
Among all patients, there was no association between higher CD34/kg or CD3/kg graft counts and the incidence of acute GVHD, chronic GVHD, relapse rate, non-relapse mortality and overall survival.
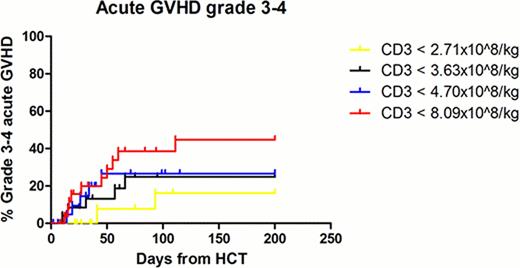
However, among male recipients given female allografts, the incidence of grade 3–4 acute GVHD in patients given higher doses of CD3 in the upper quartile was statistically significantly higher than patients receiving lower doses of CD3, namely 39% vs. 16% (p=.04), Figure. Differences were more prominent in patients given allografts from unrelated females. The incidence of grade 2–4 acute GVHD in patients given higher doses of CD3 in the upper quartile was 65%, and 50% in the 3 lower quartiles (p=.27). Of note, patients in the upper quartile had a higher non-relapse mortality (58% vs. 33% p=.05), a higher incidence of chronic GVHD (89% vs. 47%, p=.03) and a lower disease relapse rate (23% vs. 40%, p=.42). Overall survival was comparable.
These correlations were not observed when other donor-recipient gender combinations were analyzed.
Male and female donor grafts differ significantly in CD34 and CD3 cell composition. Grafts derived from female donors have a higher mean CD3 and a lower mean CD34 cell content compared with grafts derived from male donors.
CD3 dose independently impacts transplantation outcomes in male patients given female allografts, explaining some of the adverse outcomes in this subgroup compared with other donor-recipient gender combinations.
Finally, in this subgroup, escalation of CD3 dose in patients with high risk diseases and de-escalation of CD3 dose in patients with low risk diseases should be considered.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal