Abstract
Abstract 818
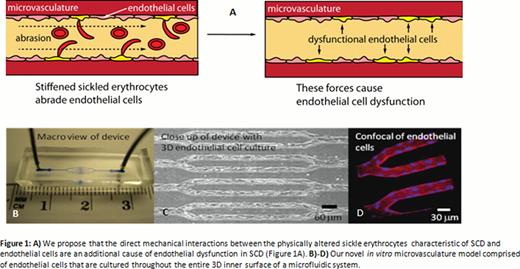
Endothelial dysfunction is a major component of sickle cell disease (SCD) pathophysiology. Interestingly, previous cardiovascular research has definitively shown that endothelial cells biologically respond to mechanical forces and aberrations in these forces cause endothelial dysfunction via pro-inflammatory pathways that are also involved in SCD. While endothelial dysfunction in SCD has been well characterized biologically, little research has focused on the direct biophysical effects of SCD blood on endothelium. As endothelial cells are in constant contact with flowing “stiffened” sickle erythrocytes, we propose that the direct mechanical interactions between the physically altered sickle erythrocytes and endothelial cells are an additional cause of endothelial dysfunction in SCD (Figure 1A).
Endothelial dysfunction in SCD is thought to be caused by the downstream effects of vaso-occlusion and/or hemolysis. Our laboratory has recently developed and published a description of an in vitro microvasculature model comprised of endothelial cells that are cultured throughout the entire 3D inner surface of a microfluidic system designed for investigating cellular interactions in hematologic diseases (Tsai, et al, JCI, 2012), (Figure 1B-D). This microvasculature-on-a-chip recapitulates an ensemble of physiological processes and biophysical properties, including adhesion molecule expression, blood cell-endothelial cell interactions, cell deformability, cell size/shape, microvascular geometry, hemodynamics, and oxygen levels (Myers et al. JoVE, 2012), all of which may contribute to endothelial dysfunction in SCD. We hypothesize that the mechanical interactions between sickle erythrocytes and endothelial cells alone are sufficientto cause endothelial dysfunction in our microvasculature-on-a-chip.
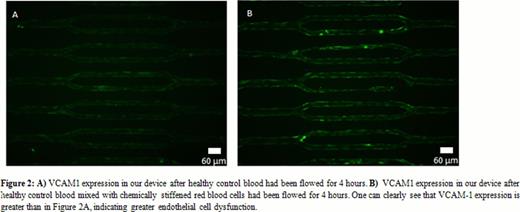
To test our hypothesis, we flowed different suspensions of healthy red blood cells (RBCs), and stiffened RBCs, through our microvasculature on a chip cultured with HUVECs. We suspended fresh human RBCs in media at a low hematocrit recapitulating the anemic conditions typically seen in SCD patients as a control. The experimental conditions used the same solution as the control, but also contained glutaraldehyde-stiffened RBCs, which are of the same stiffness as irreversibly sickled cells (ISCs), at approximately the same concentrations as ISCs in SCD patients. The stiffened RBC suspension was washed multiple times to eliminate all traces of glutaraldehyde and to ensure that any endothelial cell dysfunction in our system was due to mechanical effects between the endothelium and RBCs. After 4 hours of perfusion, the number of occlusions in our microsystem was counted and the cells were fixed and stained for Vascular Cell Adhesion Molecule 1 (VCAM-1). VCAM-1 been shown to be a marker of endothelial cell dysfunction and is a biomarker for severe vasculopathy in SCD (Dworkis, Am J Hematol, 2011). Immunofluorescence staining in our microsystem confirmed that VCAM1 is upregulated (Figure 2) in HUVECs when exposed to flowing stiffened RBCs compared to control RBCs. VCAM-1 upregulation appears to be diffuse throughout the length of the device. After experimentation, endothelial cells in our system can be isolated for further RT-PCR or microarray analysis. As such, ongoing work involves investigating and quantifying the expression of other pro-inflammatory molecules to elucidate the underlying mechanisms of this biomechanical process involving RBCs and endothelial cells. Additional experiments complementary experiments using endothelial cells from other anatomic areas, SCD patient samples, and murine SCD models are also underway.
Our data indicates that purely physical interactions between endothelial cells and stiffened RBCs are sufficient to cause some degree of endothelial dysfunction, even in the absence of vaso-occlusion, ischemia, or oxidative stress due to hemolysis. As sickle RBCs and ISCs are constantly circulating in the blood of SCD patients, our results have profound implications for SCD pathophysiology and may help explain why SCD patients develop chronic diffuse vasculopathy over time.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal