In this issue of Blood, Rego and colleagues describe the exciting accomplishments of the International Consortium on Acute Promyelocytic Leukemia (IC-APL), an initiative of the International Members Committee of the American Society of Hematology (ASH).1 The purpose of this initiative is to create a network of institutions in developing countries that will work in partnership with cooperative groups in the United States and Europe in order to close the gap in quality of care and outcomes in acute promyelocytic leukemia (APL) between developed and developing countries.
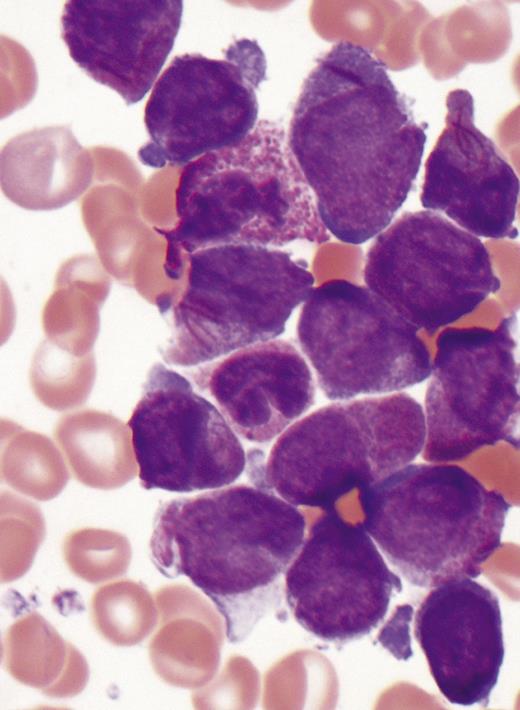
Acute promyelocytic leukemia. Image courtesy of Michael W. Beaty, Department of Pathology, Wake Forest School of Medicine.
Acute promyelocytic leukemia. Image courtesy of Michael W. Beaty, Department of Pathology, Wake Forest School of Medicine.
Those of us who have the opportunity and responsibility of caring for patients with leukemia have been fortunate to participate in disease-altering advances for 2 types of leukemia. The development of imatinib and its successor tyrosine kinase inhibitors dramatically improved the lives of patients with chronic myeloid leukemia, achieving long-term responses and survival with substantially less toxicity. Although the developments of all-trans retinoic acid (ATRA) and arsenic trioxide (ATO) have not been the products of targeted drug design, the results have been no less impressive, rendering a highly fatal cancer highly curable. As with all highly curable cancers, the emphasis shifts to dissemination of the highly effective treatment approaches to broader patient populations and to limiting complications, especially long-term complications, by decreasing exposure to toxic treatments.
Based on reports from China of high response rates in patients with relapsed and untreated APL, ATRA was soon tested in randomized phase 3 trials for untreated patients in the United States and Europe. The initial North American Leukemia Intergroup APL trial demonstrated the value of ATRA in both induction and maintenance.2 Concurrent ATRA and chemotherapy was shown by the European APL Group to be superior to sequential ATRA followed by chemotherapy as induction therapy.3 During this period, other European groups developed an effective ATRA plus idarubicin induction regimen, eliminating cytarabine.4 Rego et al describe the process for more rapid recognition and diagnosis of APL, followed by implementation of a similar treatment protocol with specified supportive care and follow-up in Brazil, Mexico, Chile, and Uruguay. The resulting outcomes show dramatic improvements over historical controls and are similar to those achieved in developed countries.1 Most importantly, they demonstrate the feasibility of moving current and future advances into diverse geographic, cultural, and socioeconomic settings.
Fortunately, additional advances are here, and more are on the way. Again, based on initial data from China, ATO has been established as a very effective treatment of relapsed APL and is the most active single agent for treatment of APL. In a randomized phase 3 trial by the North American Leukemia Intergroup, we demonstrated the effectiveness of ATO as initial consolidation therapy for patients in first remission; all recognized prognostic factors for disease-free survival were negated by the addition of ATO.5 Phase 2 studies have shown similar outcomes with incorporation of ATO into frontline therapy as consolidation and/or induction, with further decreases in chemotherapy exposure. Gore et al used ATRA plus daunorubicin induction followed by a single course of consolidation with cytarabine, daunorubicin, and ATO,6 and Ravandi et al developed a treatment regimen with no traditional chemotherapy.7 Mathews et al8 and Ghavamzadeh et al9 described promising results using single-agent ATO.
At the December 2012 annual meeting of the American Society of Hematology, Lo-Coco and colleagues presented results of a randomized phase 3 trial that compared ATRA plus ATO with ATRA plus idarubicin in low- and intermediate-risk patients.10 At the same meeting Zhu et al reported results of the Chinese APL Cooperative Group randomized phase 3 trial that compared a new oral arsenic preparation with the current intravenous ATO as induction therapy for patients with untreated APL.11 Both trials were designed as noninferiority studies and both met endpoints with excellent outcomes, including response, disease-free survival, survival, and tolerance. While we await full peer-reviewed publications of these studies, both highlight continued progress.
There remain important questions to be answered regarding APL. How do we avoid the 5% to 7% early deaths, primarily in patients presenting with high-risk disease (white blood cell counts > 10 × 109/L), that have persisted in multiple clinical trials? Perhaps the current US Intergroup trial for high-risk patients will show improvement with the early addition of gemtuzumab ozogamicin to ATRA and ATO. However, the phase 2 trial on which the study is based had an early death rate of 8%.7 How do we optimally manage the APL differentiation syndrome? How much, if any, chemotherapy is needed? If needed, then for what subgroup(s)? Is maintenance still needed in patients treated with ATO during induction and/or consolidation? Can we develop an arsenic preparation that maintains the current efficacy but can be delivered more conveniently to patients and with a high degree of compliance? Can we successfully disseminate current and future advances to colleagues in both developed and developing countries?
The present is very good for our patients with APL, and the future is even brighter. Let us hope that we will all have the wisdom to recognize progress, the open minds to embrace it, and the commitment of Rego and colleagues needed for implementation.
Conflict-of-interest disclosure: Dr Powell has served on an advisory board for Teva Pharmaceuticals.