Key Points
Apc regulates the function of HSCs/HPCs largely through a β-catenin–mediated pathway.
Multiple downstream targets of Apc may be involved in the regulation of HSC self-renewal.
Emerging evidence suggests that adenomatous polyposis coli (Apc) plays a critical role in the maintenance of hematopoietic stem/progenitor cells (HSCs/HPCs). The molecular pathways responsible for the function of Apc in HSCs/HPCs remain unclear. By genetic approach, we demonstrated that inactivation of β-catenin rescued the exhaustion of Apc-deficient HSCs/HPCs, thereby preventing bone marrow failure in Apc-deficient mice. β-catenin loss inhibited the excessive proliferation and apoptosis of Apc-deficient HSCs/HPCs, as well as their defects in myeloid and erythroid differentiation. In addition, loss of β-catenin reversed the down-regulation of Cdkn1a, Cdkn1b, and Mcl1 induced by Apc ablation in Lin−Sca+c-Kit+. In assays of long-term stem cell function, the HSCs with deficiency of both Apc and β-catenin displayed a significantly enhanced self-renewal capacity compared with β-catenin–deficient and control HSCs. Our findings suggest that Apc regulates the survival, proliferation, and differentiation of HSCs/HPCs largely through a β-catenin–mediated pathway. They also indicate that multiple downstream targets of Apc including β-catenin may coordinately regulate HSC self-renewal.
Introduction
Adenomatous polyposis coli (APC) was identified as a tumor suppressor involved in the initiation and progression of colorectal cancer.1 APC has been implicated in self-renewal and differentiation of embryonic stem cells2 and adult stem cells in various tissues.3 Loss of Apc leads to expansion of the intestinal stem cell compartment.3 However, Apc is required for survival of neural crest cells that are a multipotent stem cell population.4 Similarly, we found that loss of Apc leads to depletion of hematopoietic stem cells (HSCs) in vivo.5 Accumulating evidence suggests that Apc is a key player in the regulation of HSCs and hematopoietic progenitor cells (HPCs).6,-8
In the current model of APC function, APC negatively regulates the Wnt/β-catenin pathway by controlling the turnover of β-catenin.3 Loss of APC leads to accumulation of intracellular β-catenin and translocation of β-catenin to the nucleus, consequently activating cell cycle regulators such as c-myc and cyclin D1.9,10 However, increasing evidence suggests that APC is involved in multiple signaling pathways and different cellular processes independently of Wnt/β-catenin signaling. In 293T and SW280 cells, APC enhances GSK3β activity, whereas repression of APC up-regulates mammalian target of rapamycin (mTOR) signaling.11 Recently, Rai et al12 showed that loss of APC resulted in hypomethylation of key intestinal cell fating genes by up-regulation of the DNA demethylase system, indicating that in intestinal cells APC controls DNA methylation dynamics. APC also plays a role in cell migration and adhesion by regulating microtubule and actin cytoskeletons.13,14 Regulation of spindle assembly and chromosome segregation by APC contributes to its role in maintaining mitotic fidelity.15 APC shuttles between the cytoplasm and the nucleus,16 and it was shown that it regulates DNA replication in response to stress and DNA damage. Moreover, it was reported that APC regulates the phosphorylation of the replication protein A subunit RPA32 and of histone H2AX in response to DNA damage treatment.17,-19
Previously, we were the first group to demonstrate that Apc is essential for the maintenance of HSCs/HPCs in vivo.5 In this study, we extended our efforts to determine which pathways are crucial for the function of Apc in HSCs/HPCs. Our findings provide new insights into the function of Apc in HSCs/HPCs.
Methods
Generation of Apc- and β-catenin–deficient mice
Apcfl/fl Mx1-cre mice5 were crossed with β-cateninfl/fl transgenic mice (The Jackson Laboratory) to obtain Mx1-CreApcfl/flβ-cateninfl/fl, Mx1-CreApcfl/fl, Mx1-Creβ-cateninfl/flβ-cateninfl/fl, and Apcfl/flβ-cateninfl/fl mice. Deletion of Apc or β-catenin was induced by 3 intraperitoneal (IP) injections of 6 to 10 μg polyI–polyC (pI-pC; GE Healthcare) per gram of body weight every second day for a total of 3 injections.5 The deletion of Apc and β-catenin was confirmed by polymerase chain reaction (PCR) analysis. All animal research was approved by the University of Illinois at Chicago Institutional Animal Care and Use Committee.
Flow cytometric analysis
Flow cytometric analyses of subsets of HPCs and HSCs have been described in our previous studies.5,7 Dead cells were excluded by 4,6 diamidino-2-phenylindole staining. Fluorescence-activated cell sorter analysis was performed using a CyAn ADP flow cytometer (Beckman Coulter). For the detection of apoptosis, bone marrow (BM) cells were stained with antibody conjugates, Annexin V, and 4,6 diamidino-2-phenylindole (BD Biosciences). All data were analyzed by FlowJo software (TreeStar, Inc).
Administration of rapamycin
Rapamycin (LC Laboratories) was dissolved in absolute ethanol at 10 mg/mL and diluted in 5% Tween-80 (Sigma-Aldrich) and 5% PEG-400 (Hampton Research) before injection, and was administered by IP injection at 4 μg/g rapamycin every other day.20 The mice received rapamycin 18 days before pI-pC, and the treatment continued until they became moribund.
Cell cycle analysis
For 5-bromo-2′-deoxyuridine (BrdU) labeling, mice were injected IP with 100 µL of 10 mg/mL BrdU (Sigma) 24 hours before euthanizing them. According to the BrdU flow kit instruction manual (BD Bioscience), the BM cells were stained with fluorochrome-conjugated antibodies, followed by fixation and permeabilization with Cytofix/Cytoperm (BD Biosciences), treatment with DNaseI (Sigma), and staining with anti-BrdU antibody (eBioscience). The cells were analyzed by flow cytometry using a CyAn ADP flow cytometer.
Statistical analysis
All data are mean ± standard deviation. All analyses were performed using two-tailed t tests assuming equal variance, and P < .05 was considered significant.
Results
Depletion of β-catenin rescues BM failure induced by Apc loss
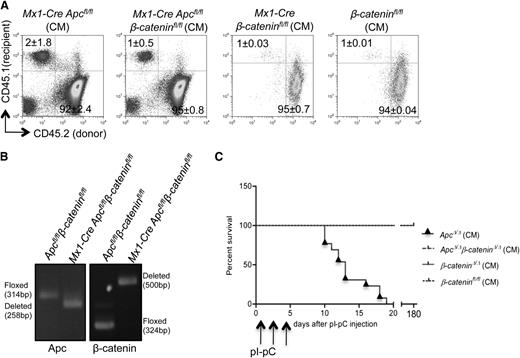
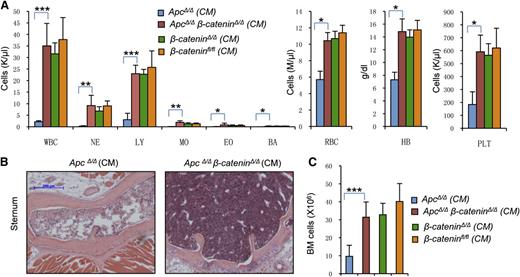
Whether β-catenin or additional downstream pathways are required for Apc function in hematopoiesis is still unclear. Loss of function of Apc leads to development of BM failure in mice.5 Therefore, we first determined whether β-catenin loss rescues BM failure following Apc ablation in the mouse. We generated conditional knockout mice including Mx1-Cre Apcfl/flβ-cateninfl/fl, Mx1-Cre Apcfl/fl, Mx1-Cre β-cateninfl/fl, and β-cateninfl/fl mice. In these mice, excision of Apc or β-catenin can be induced by injection of the interferon-α inducer pI pC. Because Mx1-Cre is expressed in multiple tissues, pI-pC injection in primary mice induced Apc or β-catenin deletion in multiple tissues, leading to lethality in a short period of time due to severe nonhematopoietic effects.5,21 Therefore, we transplanted the BM cells from these primary mice into wild-type syngeneic recipients to generate chimeric mice (CM). As shown in Figure 1A, all donor HSCs/HPCs from primary Mx1-Cre Apcfl/flβ-cateninfl/fl (referred to as ApcΔ/Δβ-cateninΔ/Δ after induction), Mx1-Cre Apcfl/fl (referred to as ApcΔ/Δ after induction), Mx1-Cre β-cateninfl/fl (referred to as β-cateninΔ/Δ after induction), and β-cateninfl/fl mice had comparable engraftment in recipient mice, in which the majority of peripheral blood (PB) cells (92%-97%) were derived from donor HSCs/HPCs (CD45.2+). The ablation of Apc or β-catenin in the HSC-enriched LSK (Lin−Sca+c-Kit+) compartment from Mx1-Cre Apcfl/flβ-cateninfl/fl mice was induced by injection of pI-pC and was confirmed by PCR analysis, which demonstrated the excision in the majority of LSKs (Figure 1B). The absence of Apc and β-catenin proteins in Lin− BM cells from the same mice was confirmed by western blot analysis (supplemental Figure 1A on the Blood website). Consistent with our previous results, all ApcΔ/Δ CM mice succumbed to BM failure within the first 3 weeks after pI-pC injection (Figure 1C), whereas all the ApcΔ/Δβ-cateninΔ/Δ, β-cateninΔ/Δ, and β-cateninfl/fl CM survived into the sixth month (Figure 1C). The Mx1-Cre Apcfl/flβ-cateninfl/fl and control CM mice exhibited normal hematological parameters before and after pI-pC treatment (Figure 2A). In contrast, the Mx1-Cre Apcfl/fl CM with normal hematological counts before the pI-pC injection displayed a significant decrease in the number of white blood cells, platelets, red blood cells, and lymphocytes after Cre induction (Figure 2A). As shown in Figure 2B-C, the BM cellularity is also decreased significantly in ApcΔ/Δ CM mice, whereas the ApcΔ/Δβ-cateninΔ/Δ CM mice had a normal BM cellularity. To determine whether the ApcΔ/Δβ-cateninΔ/Δ CM mice developed a disease with a long latency, we monitored a group of Mx1-Cre Apcfl/fβ-cateninfl/fl CM mice with or without pI-pC injection up to 6 months. The ApcΔ/Δβ-cateninΔ/Δ CM mice displayed a normal complete blood count (CBC) compared with Mx1-Cre Apcfl/flβ-cateninfl/fl CM mice (supplemental Figure 1B). These data suggest that loss of β-catenin prevents the BM failure induced by Apc ablation.
Loss of β-catenin rescues Apc-deficient mice. (A) Comparison of engraftment efficiency of CD45.2 Mx1-Cre Apcfl/fl, Mx1-Cre Apcfl/flβ-cateninfl/fl, Mx1-Cre β-cateninfl/fl, or β-cateninfl/fl BM cells in wild-type recipient mice (CD45.1) by flow cytometric analysis of peripheral blood (PB) at 6 weeks after transplantation (mean ± standard deviation, n = 4-6). (B) Analysis of deletion of Apc or β-catenin as determined by PCR analysis of genomic DNA from BM LSKs 7 days after the last injection of pI-pC. (C) Kaplan-Meier survival curve of recipient mice reconstituted with BM cells from Mx1-Cre Apcfl/fl, Mx1-Cre Apcfl/flβ-cateninfl/fl (n = 13), Mx1-Cre β-cateninfl/fl, or β-cateninfl/f (n = 5-10) mice after 3 doses of pI-pC injection. Arrowheads indicate pI-pC injections.
Loss of β-catenin rescues Apc-deficient mice. (A) Comparison of engraftment efficiency of CD45.2 Mx1-Cre Apcfl/fl, Mx1-Cre Apcfl/flβ-cateninfl/fl, Mx1-Cre β-cateninfl/fl, or β-cateninfl/fl BM cells in wild-type recipient mice (CD45.1) by flow cytometric analysis of peripheral blood (PB) at 6 weeks after transplantation (mean ± standard deviation, n = 4-6). (B) Analysis of deletion of Apc or β-catenin as determined by PCR analysis of genomic DNA from BM LSKs 7 days after the last injection of pI-pC. (C) Kaplan-Meier survival curve of recipient mice reconstituted with BM cells from Mx1-Cre Apcfl/fl, Mx1-Cre Apcfl/flβ-cateninfl/fl (n = 13), Mx1-Cre β-cateninfl/fl, or β-cateninfl/f (n = 5-10) mice after 3 doses of pI-pC injection. Arrowheads indicate pI-pC injections.
Loss of β-catenin prevents development of BM failure in Apc-deficient mice. (A) The number of white blood cells (WBC), neutrophils (NE), lymphocytes (LY), monocytes (MO), eosinophils (EO), basophils (BA), red blood cells (RBC), platelets (PLT), and hemoglobin (Hb) levels in PB from ApcΔ/Δ, ApcΔ/Δβ-cateninΔ/Δ, β-cateninΔ/Δ, or β-cateninfl/fl chimeric mice (CM) 7-13 days after last pI-pC injection (n = 5). (B) Representative histological analysis of hematoxylin and eosin–stained sternum from ApcΔ/Δ CM and ApcΔ/Δβ-cateninΔ/Δ CM 13 days after induction. (C) Numbers of total BM cells in ApcΔ/Δ, ApcΔ/Δβ-cateninΔ/Δ, β-cateninΔ/Δ, or β-cateninfl/fl CM 7-15 days after induction (mean ± standard deviation, n = 5-10). *P < .05; **P < .01; ***P < .001.
Loss of β-catenin prevents development of BM failure in Apc-deficient mice. (A) The number of white blood cells (WBC), neutrophils (NE), lymphocytes (LY), monocytes (MO), eosinophils (EO), basophils (BA), red blood cells (RBC), platelets (PLT), and hemoglobin (Hb) levels in PB from ApcΔ/Δ, ApcΔ/Δβ-cateninΔ/Δ, β-cateninΔ/Δ, or β-cateninfl/fl chimeric mice (CM) 7-13 days after last pI-pC injection (n = 5). (B) Representative histological analysis of hematoxylin and eosin–stained sternum from ApcΔ/Δ CM and ApcΔ/Δβ-cateninΔ/Δ CM 13 days after induction. (C) Numbers of total BM cells in ApcΔ/Δ, ApcΔ/Δβ-cateninΔ/Δ, β-cateninΔ/Δ, or β-cateninfl/fl CM 7-15 days after induction (mean ± standard deviation, n = 5-10). *P < .05; **P < .01; ***P < .001.
Excision of β-catenin rescues the depletion of myeloid progenitor cells and reverses the blockage of myeloid lineage differentiation induced by Apc loss
CBC analysis of PB in ApcΔ/Δβ-cateninΔ/Δ CM mice suggests that loss of β-catenin reverses the inhibition of myeloid and erythroid differentiation induced by Apc ablation. To confirm this hypothesis, we examined the myeloid and erythroid compartments in Mx1-Cre Apcfl/flβ-cateninfl/fl CM and Mx1-Cre Apcfl/fl CM 2 to 3 weeks after pI-pC injection by flow cytometric analysis. We observed a significant increase of Mac-1+Gr-1+ mature myeloid cells in the BM (Figure 3A, left) and spleen (supplemental Figure 2A) in ApcΔ/Δβ-cateninΔ/Δ CM compared with ApcΔ/Δ CM, whereas the ApcΔ/Δβ-cateninΔ/Δ, β-cateninΔ/Δ, and control CM exhibited similar frequency of Mac-1+Gr-1+ cells in BM and spleen at 5 weeks after pI-pC treatment (Figure 3A, right; supplemental Figure 2A), indicating that the myeloid differentiation returned to normal level in ApcΔ/Δβ-cateninΔ/Δ CM. Loss of Apc resulted in ineffective erythropoiesis due to a blockage of maturation at the proerythroblast (R1, Ter119lowCD71hi) and basophilic erythroblast (R2, Ter119hiCD71hi) early stages.5 The frequency of R1 and R2 erythroblasts in ApcΔ/Δβ-cateninΔ/Δ CM was significantly reduced in the BM (Figure 3B, left) and spleen (supplemental Figure 2B) compared with ApcΔ/Δ CM. However, 5 weeks after induction, the distribution of these subsets of erythroblasts in BM and spleen of ApcΔ/Δβ-cateninΔ/Δ mice was normal compared with β-cateninΔ/Δ and control CM (Figure 3B; supplemental Figure 2C). A group of mice were analyzed 6 months after depletion of Apc and β-catenin. In agreement with CBC analysis of PB in these mice (supplemental Figure 1), the distribution of mature myeloid and red cells in ApcΔ/Δβ-cateninΔ/Δ CM is comparable to that of control mice (supplemental Figure 3), suggesting that these mice had normal terminal myelopoiesis and erythropoiesis with long latency. Consistent with previously reported studies,21 we found that loss of β-catenin does not affect myeloid and erythroid differentiation in vivo.
β-catenin deletion reverses myeloid and erythroid cell differentiation blockage and exhaustion induced by Apc loss. (A-B) Histograms represent the frequency of Mac-1+Gr+ (A) myeloid cells and (B) erythroblasts in BM from ApcΔ/Δ and ApcΔ/Δβ-cateninΔ/Δ CM (left, 2 weeks after induction) or ApcΔ/Δβ-cateninΔ/Δ, β-cateninΔ/Δ, and β-cateninfl/fl (right, 5 weeks after induction). Mean ± standard deviation (SD); n = 4. (C) In vitro colony-forming unit (CFU) assays. The number of BM CFC, CFU-granulocyte-erythroid-monocyte-megakaryocyte, CFU-granulocyte-macrophage, CFU-granulocyte, CFU-megakaryocyte, and burst-forming unit-erythroid was examined in Mx1-Cre Apcfl/fl, Mx1-Cre Apcfl/flβ-cateninfl/fl, Mx1-Cre β-cateninfl/fl, and β-cateninfl/fl mice 5 days after induction (mean ± SD, n = 3). (D) Representative histograms are shown for the frequency of subpopulations of myeloid progenitor cells in ApcΔ/Δ and ApcΔ/Δβ-cateninΔ/Δ CM 2 weeks after induction. (E-F) Absolute number of myeloid progenitor cells in BM from (E) ApcΔ/Δ and ApcΔ/Δβ-cateninΔ/Δ CM (mean ± SD; n = 6-7) 2 weeks after induction or (F) BM from ApcΔ/Δβ-cateninΔ/Δ, β-cateninΔ/Δ, and β-cateninfl/fl (mean ± SD; n = 3) 5 weeks after induction. *P < .05; **P < .01; ***P < .001.
β-catenin deletion reverses myeloid and erythroid cell differentiation blockage and exhaustion induced by Apc loss. (A-B) Histograms represent the frequency of Mac-1+Gr+ (A) myeloid cells and (B) erythroblasts in BM from ApcΔ/Δ and ApcΔ/Δβ-cateninΔ/Δ CM (left, 2 weeks after induction) or ApcΔ/Δβ-cateninΔ/Δ, β-cateninΔ/Δ, and β-cateninfl/fl (right, 5 weeks after induction). Mean ± standard deviation (SD); n = 4. (C) In vitro colony-forming unit (CFU) assays. The number of BM CFC, CFU-granulocyte-erythroid-monocyte-megakaryocyte, CFU-granulocyte-macrophage, CFU-granulocyte, CFU-megakaryocyte, and burst-forming unit-erythroid was examined in Mx1-Cre Apcfl/fl, Mx1-Cre Apcfl/flβ-cateninfl/fl, Mx1-Cre β-cateninfl/fl, and β-cateninfl/fl mice 5 days after induction (mean ± SD, n = 3). (D) Representative histograms are shown for the frequency of subpopulations of myeloid progenitor cells in ApcΔ/Δ and ApcΔ/Δβ-cateninΔ/Δ CM 2 weeks after induction. (E-F) Absolute number of myeloid progenitor cells in BM from (E) ApcΔ/Δ and ApcΔ/Δβ-cateninΔ/Δ CM (mean ± SD; n = 6-7) 2 weeks after induction or (F) BM from ApcΔ/Δβ-cateninΔ/Δ, β-cateninΔ/Δ, and β-cateninfl/fl (mean ± SD; n = 3) 5 weeks after induction. *P < .05; **P < .01; ***P < .001.
To determine the effect of β-catenin loss on Apc-deficient HPCs, we performed in vitro colony-forming unit assays to evaluate the frequency of myeloid progenitors in the BM from primary Mx1-Cre Apcfl/fβ-cateninfl/fl, Mx1-Cre Apcfl/fl, Mx1-Cre β-cateninfl/fl, and β-cateninfl/fl mice. The BM cells were harvested 5 days after pI-pC injection, and an equal number of cells were plated in methyl-cellulose medium containing stem cell factor, interleukin 3, and interleukin 6. The ApcΔ/Δ BM cells gave rise to fewer colony-forming units and colony-forming unit-granulocyte-erythroid-monocyte-megakaryocyte, colony-forming unit-granulocyte-macrophage, colony-forming unit granulocyte, colony-forming unit megakaryocyte and burst-forming unit-erythroid colonies, whereas the ApcΔ/Δβ-cateninΔ/Δ, β-cateninΔ/Δ, and β-cateninfl/fl BM cells formed similar numbers of these colonies (Figure 3C). Next, we characterized by flow cytometric analysis the subpopulations of myeloid progenitors in the CM at 2 or 5 weeks after pI-pC injection. Two weeks after induction, the frequency of common myeloid progenitors (Lin−Sca-1−IL-7R−c-kit+ FcγRII/IIIlow CD34hi), and granulocyte-monocyte progenitors (Lin−Sca-1−IL-7R−c-kit+ FcγRII/IIIhi CD34hi) myeloid progenitors was dramatically reduced, whereas the frequency of megakaryocyte-erythroid progenitors (Lin−Sca-1−IL-7R−c-kit+ FcγRII/IIIlowCD34low) in ApcΔ/Δ CM was increased; however, the total number of myeloid progenitors in the three subsets was significantly lower in ApcΔ/Δ CM than in ApcΔ/Δβ-cateninΔ/Δ CM (Figure 3D-E). Although at 5 weeks after induction the number of HPCs and common myeloid progenitors was slightly lower in ApcΔ/Δβ-cateninΔ/Δ CM than in β-cateninΔ/Δ and control CM (Figure 3F), at 6 months after induction, the number of all subsets of myeloid progenitors was normal in ApcΔ/Δβ-cateninΔ/Δ CM compared with Mx1-Cre Apcfl/flβ-cateninfl/fl CM without induction (supplemental Figure 4). Collectively, these results indicate that the effect of Apc loss on survival of myeloid progenitors and on myeloid and erythroid differentiation could be reversed by ablation of β-catenin.
Loss of β-catenin prevents rapid exhaustion of Apc-deficient HSCs
The observation that β-catenin ablation prevented Apc-deficient mice from developing BM failure suggests that the defects of Apc-deficient HSCs could be partially rescued by β-catenin ablation. Therefore, we examined the HSC compartment in ApcΔ/Δβ-cateninΔ/Δ and ApcΔ/Δ CM. The frequency and total number of LSKs and LT-HSCs (Lin-Sca+c-Kit+CD48−CD150+) were increased in ApcΔ/Δβ-cateninΔ/Δ CM compared with ApcΔ/Δ CM at 10 to 14 days after induction of Apc and β-catenin deletion (Figure 4A-B). As expected, all ApcΔ/Δ CM died within 3 weeks after pI-pC injection. To determine whether the loss of both Apc and β-catenin alters the number of phenotypic HSCs, we further examined the HSCs in ApcΔ/Δβ-cateninΔ/Δ, β-cateninΔ/Δ, and control CM 5 weeks after pI-pC injection. The ApcΔ/Δβ-cateninΔ/Δ CM had frequency and total number of HSCs comparable to β-cateninΔ/Δ and control CM (Figure 4C), indicating that β-catenin ablation inhibits the exhaustion of Apc-deficient HSCs in the short term. To rule out the possibility that loss of β-catenin failed to prevent the depletion of Apc-deficient HSCs in the long term, we next examined the HSCs in Mx1-Cre Apcfl/flβ-cateninfl/fl CM not treated with pI-pC or 6 months after induction of Apc and β-catenin deletion. We found that both LSK cells and LT-HSCs were significantly expanded in ApcΔ/Δβ-cateninΔ/Δ mice after induction compared with the noninduced controls (Figure 4D). Together, these data suggest that inactivation of β-catenin prevents exhaustion of Apc-deficient HSCs in both the short and long term.
Loss of β-catenin prevents rapid exhaustion of Apc-deficient HSCs in vivo. (A) Flow cytometric analysis of the frequency of stem cell-enriched population (Lin-c-Kit+Sca+ [LSK]) and HSCs (LSK CD150+CD48−) in BM from representative ApcΔ/Δ and ApcΔ/Δβ-cateninΔ/Δ mice 10-14 days after induction. (B-D) The histograms depict the total number of HSCs in BM (B) from ApcΔ/Δand ApcΔ/Δβ-cateninΔ/Δ mice 10-14 days after induction (mean ± standard deviation [SD], n = 5-8), (C) from ApcΔ/Δβ-cateninΔ/Δ, β-cateninΔ/Δ, and β-cateninfl/fl mice 5 weeks after induction (mean ± SD, n = 3), and (D) from ApcΔ/Δβ-cateninΔ/Δ (6 months after induction) and Mx1-Cre Apcfl/flβ-cateninfl/fl (mean ± SD, n = 2-4). *P < .05; ***P < .001.
Loss of β-catenin prevents rapid exhaustion of Apc-deficient HSCs in vivo. (A) Flow cytometric analysis of the frequency of stem cell-enriched population (Lin-c-Kit+Sca+ [LSK]) and HSCs (LSK CD150+CD48−) in BM from representative ApcΔ/Δ and ApcΔ/Δβ-cateninΔ/Δ mice 10-14 days after induction. (B-D) The histograms depict the total number of HSCs in BM (B) from ApcΔ/Δand ApcΔ/Δβ-cateninΔ/Δ mice 10-14 days after induction (mean ± standard deviation [SD], n = 5-8), (C) from ApcΔ/Δβ-cateninΔ/Δ, β-cateninΔ/Δ, and β-cateninfl/fl mice 5 weeks after induction (mean ± SD, n = 3), and (D) from ApcΔ/Δβ-cateninΔ/Δ (6 months after induction) and Mx1-Cre Apcfl/flβ-cateninfl/fl (mean ± SD, n = 2-4). *P < .05; ***P < .001.
Loss of β-catenin inhibits proliferation and apoptosis of HSCs/HPCs induced by Apc ablation
To determine whether β-catenin ablation prevents the exhaustion of Apc-deficient HPCs and LSKs by suppressing proliferation or apoptosis of the cells, we analyzed the cell cycle and apoptosis rate of HPCs/LSKs in the CM. We found that 4 days after induction, the fraction of Apc–β-catenin–deficient LSKs and HPCs in S phase was reduced significantly (Figure 5A). As shown in our previous study,5 loss of Apc leads to the accumulation of cells in the G2/M phase in LSKs but not HPCs. Here, we found that inactivation of β-catenin also released the blockage of the G2/M phase in LSKs (Figure 5A). At 5 weeks and 6 months after induction, flow cytometric analysis of LSKs and HPCs (Figure 5B; supplemental Figure 5) indicated that Apc–β-catenin–deficient LSKs and HPCs had normal S and G2/M phases similar to the LSKs and HPCs of control CM. In addition, we found that 2 weeks after induction, Apc–β-catenin–deficient LSKs and HPCs displayed a significant decrease of apoptosis compared with Apc-deficient HPCs/LSKs (Figure 5C). Nonetheless, the frequency of apoptosis in LSKs and HPCs in Apc–β-catenin–deficient CM and control CM was comparable 5 weeks and 6 months after induction (Figure 5D; supplemental Figure 6). Therefore, these data indicate that β-catenin ablation inhibits proliferation and apoptosis of Apc-deficient HPCs/LSKs in vivo.
Loss of β-catenin suppresses elevated proliferation and apoptosis in Apc-deficient HPCs and LSKs in vivo. (A) Analysis of cell cycle status of LSKs and HPCs in BM from Mx1-Cre Apcfl/fland Mx1-Cre Apcfl/flβ-cateninfl/fl mice 4 days after pI-pC injection. BrdU was injected into mice 24 hours before analysis (mean ± standard deviation [SD]; n = 3-4). (B) Histograms depict the mean distribution of cell cycle phases of HPCs and LSKs in BM from ApcΔ/Δβ-cateninΔ/Δ, β-cateninΔ/Δ, and β-cateninfl/fl 5 weeks after induction (mean ± SD; n = 3-4). (C) Analysis of frequency of apoptosis in HPCs and LSKs in BM from Mx1-Cre Apcfl/fl and Mx1-Cre Apcfl/flβ-cateninfl/fl mice 2 weeks after pI-pC injection (mean ± SD; n = 3-4). (D) Histograms depict the mean frequency of apoptosis of HPCs and LSKs from ApcΔ/Δβ-cateninΔ/Δ, β-cateninΔ/Δ, and β-cateninfl/fl 5 weeks after induction (mean ± SD; n = 3-4). *P < .05; **P < .01; ***P < .001. (E) Analysis of gene expression in Apcfl/fl, Apc-deficient, β-catenin–deficient, and Apc–β-catenin–deficient LSKs by quantitative PCR. The LSKs were isolated from the mice 4 days after induction. Cdkn1a, Cdkn1b, and Mcl1 are expressed at comparable levels in LSKs from β-cateninΔ/Δ and ApcΔ/Δβ-cateninΔ/Δ. Gene expression is normalized initially to actin expression. In β-catenin–deficient and Apc–β-catenin–deficient LSKs, values represent fold changes in gene expression relative to Cdkn1a in β-catenin–deficient LSKs (mean ± SD of 3 mice), whereas in Apcfl/fland Apc-deficient LSKs, values indicate the fold changes in gene expression relative to Cdkn1a in Apfl/fl LSKs (mean ± SD of 3-6 mice). *P < .05.
Loss of β-catenin suppresses elevated proliferation and apoptosis in Apc-deficient HPCs and LSKs in vivo. (A) Analysis of cell cycle status of LSKs and HPCs in BM from Mx1-Cre Apcfl/fland Mx1-Cre Apcfl/flβ-cateninfl/fl mice 4 days after pI-pC injection. BrdU was injected into mice 24 hours before analysis (mean ± standard deviation [SD]; n = 3-4). (B) Histograms depict the mean distribution of cell cycle phases of HPCs and LSKs in BM from ApcΔ/Δβ-cateninΔ/Δ, β-cateninΔ/Δ, and β-cateninfl/fl 5 weeks after induction (mean ± SD; n = 3-4). (C) Analysis of frequency of apoptosis in HPCs and LSKs in BM from Mx1-Cre Apcfl/fl and Mx1-Cre Apcfl/flβ-cateninfl/fl mice 2 weeks after pI-pC injection (mean ± SD; n = 3-4). (D) Histograms depict the mean frequency of apoptosis of HPCs and LSKs from ApcΔ/Δβ-cateninΔ/Δ, β-cateninΔ/Δ, and β-cateninfl/fl 5 weeks after induction (mean ± SD; n = 3-4). *P < .05; **P < .01; ***P < .001. (E) Analysis of gene expression in Apcfl/fl, Apc-deficient, β-catenin–deficient, and Apc–β-catenin–deficient LSKs by quantitative PCR. The LSKs were isolated from the mice 4 days after induction. Cdkn1a, Cdkn1b, and Mcl1 are expressed at comparable levels in LSKs from β-cateninΔ/Δ and ApcΔ/Δβ-cateninΔ/Δ. Gene expression is normalized initially to actin expression. In β-catenin–deficient and Apc–β-catenin–deficient LSKs, values represent fold changes in gene expression relative to Cdkn1a in β-catenin–deficient LSKs (mean ± SD of 3 mice), whereas in Apcfl/fland Apc-deficient LSKs, values indicate the fold changes in gene expression relative to Cdkn1a in Apfl/fl LSKs (mean ± SD of 3-6 mice). *P < .05.
Our previous studies suggested that the down-regulation of Mcl1, Cdkn1a, and Cdkn1b following Apc loss in HSCs/HPCs could contribute to the up-regulation of proliferation and to the reduced survival of Apc-deficient HSCs/HPCs,5 because these genes are critical for the maintenance of HSCs/HPCs. Cdkn1a regulates HSC cell cycling and self-renewal,22 whereas Cdkn1b controls HPC proliferation and pool size.23 Nonetheless, Mcl1 is essential for survival of HSCs.24 To determine whether deregulation of Mcl1, Cdkn1a, and Cdkn1b in Apc-deficient LSKs is mediated by β-catenin, we analyzed the expression of these genes by quantitative reverse transcriptase-PCR in LSK cells isolated from Apcfl/fl, ApcΔ/Δ, ApcΔ/Δβ-cateninΔ/Δ, and β-cateninΔ/Δ cells 4 days after induction (Figure 5E). Compared with control Apcfl/fl LSKs, Cdkn1a, Cdkn1b, and Mcl1 were down-regulated significantly in ApcΔ/Δ LSKs, whereas the expression of these genes was similar in LSKs isolated from ApcΔ/Δβ-cateninΔ/Δ and β-cateninΔ/Δ mice. These results indicate that the regulation of these genes by Apc depends on β-catenin, thereby supporting our observation that β-catenin is a critical mediator of Apc function in proliferation and survival of HSCs/HPCs. In addition, we found that Cdkn1b was expressed at a significantly lower level than Cdkn1a in both ApcΔ/Δβ-cateninΔ/Δ and β-cateninΔ/Δ mice, but both genes were expressed at a comparable level in Apcfl/fl mice, suggesting that Cdkn1b is regulated by β-catenin in LSKs.
After loss of Apc and β-catenin, long-term HSCs display enhanced self-renewal compared with control HSCs
According to the results described above, loss of both Apc and β-catenin resulted in a slight expansion of phenotypic HSCs. This finding prompted us to ask whether loss of both genes could affect the function of HSCs. Therefore, to follow stem cell repopulating activity, we performed a competitive repopulation assay (Figure 6A). This assay allows a direct and sensitive comparison of the reconstitution capacity of stem cells. Two months after induction of Apc and β-catenin deletion, we transplanted the same number of BM cells from ApcΔ/Δβ-cateninΔ/Δ, Mx1-Cre β-cateninΔ/Δ, or β-cateninΔ/Δ CM (CD45.2; transplanted mice) along with equal number of wild-type competitive BM cells (CD45.1CD45.2) from the primary mice into lethally irradiated syngeneic recipients (CD45.1). The frequency of donor-derived myeloid cells (Mac-1+), B cells (B220+), and T cells (CD3+) in PB cells, reflecting the repopulation capacity of donor HSCs/HPCs, was analyzed every month after transplantation. It was reported that the HSC repopulating capacity drops significantly after each round of transplantation due to significant stress during BM transplantation.25,26 For the first round of transplantation, the ApcΔ/Δβ-cateninΔ/Δ, β-cateninΔ/Δ, and β-cateninfl/fl HSCs were isolated directly from the recipient mice and have undergone a round of transplantation, whereas the wild-type competitor cells were isolated from primary mice. Thus, they had a significantly lower capacity to repopulate mature hematopoietic cells than the wild-type competitor cells (Figure 6B). However, the ApcΔ/Δβ-cateninΔ/Δ HSCs/HPCs displayed a significantly greater contribution to multiple lineages, including myeloid, B, and T cells, than β-cateninΔ/Δ and β-cateninfl/fl HSCs/HPCs. At 3 months after the first transplantation, the ratio of ApcΔ/Δβ-cateninΔ/Δ-derived total PB cells vs competitor-derived PB cells was increased 8- to 10-fold compared with β-cateninΔ/Δ and control-derived PB cells (Figure 6C-D). The BM cells from these mice were transplanted into secondary recipients. The fold change in production of mature PB cells from ApcΔ/Δβ-cateninΔ/Δ HSCs vs β-cateninΔ/Δ and β-cateninfl/fl increased (Figure 6C-D) at 1 month after transplantation compared with the fold change at 3 months after transplantation in the first transplantation. However, in the secondary transplantation, ApcΔ/Δβ-cateninΔ/Δ HSCs gradually lost their repopulation capacity at 2 and 4 months after transplantation, although their repopulation capacity was still much higher than β-cateninΔ/Δ and β-cateninfl/fl HSCs. The ApcΔ/Δβ-cateninΔ/Δ HSCs had an engraftment bias toward myeloid cell differentiation at the expense of T-cell differentiation relative to β-cateninΔ/Δ and control HSCs/HPCs (Figure 6E). Five months after the first transplantation, we analyzed the HSCs/HPCs and mature cells in the BM. We found that the contribution of ApcΔ/Δβ-cateninΔ/Δ HSCs/HPCs to mature myeloid, B, and T cells was significantly greater than that of β-cateninΔ/Δ and β-cateninfl/fl HSCs (supplemental Figure 7). In addition, further analysis of the ratio of donor cells from CM and wild-type competitors in HPCs and stem-cell enriched LSKs and CD34-LSK cell populations revealed that ApcΔ/Δβ-cateninΔ/Δ HSCs generated more primitive BM cells than β-cateninΔ/Δ and β-cateninfl/fl HSCs did (Figure 6F-G). To confirm these results, we repeated the competitive repopulation assay with donor BM cells isolated directly from primary ApcΔ/Δβ-cateninΔ/Δ, β-cateninΔ/Δ, and β-cateninfl/fl 1 week after 3 doses of pI-pC. As shown in supplemental Figure 8, at 1 and 2 months after transplantation, the repopulation capacity of ApcΔ/Δβ-cateninΔ/Δ, β-cateninΔ/Δ, and β-cateninfl/fl HSCs from primary mice was comparable, but 4 months after transplantation, the ApcΔ/Δβ-cateninΔ/Δ HSCs displayed a significantly higher repopulation capacity than β-cateninΔ/Δ and β-cateninfl/fl HSCs. Because HSCs from primary mice have not been exposed to the transplantation-induced stress, the increase in repopulation capacity of ApcΔ/Δβ-cateninΔ/Δ HSCs vs β-cateninΔ/Δ and β-cateninfl/fl HSCs from primary mice was less dramatic than they were from recipient mice. Together, these results suggest that HSCs with loss of both Apc and β-catenin have an enhanced repopulation capacity compared with the control HSCs.
HSCs with loss of both Apc and β-catenin show an enhanced repopulation capacity. (A) Diagram for the experimental design. CM were generated by transplanting an equal number of wild-type CD45.1+CD45.2+ BM cells (from primary mice) and CD45.2+ BM cells from Mx1-Cre Apcfl/flβ-cateninfl/fl, Mx1-Cre β-cateninfl/fl, or β-cateninfl/fl transplanted mice 2 months after induction. These transplanted mice have undergone 1 round of transplantation. (B) Flow cytometric analysis of CD45.2+CD45.1− (donor cells) and CD45.1+CD45.2+ (competitor cells) PB cells from representative CM 1 month after transplantation. The numbers indicate the percentage of cells in each population. (C) Histogram shows the relative ratio of CD45.2+CD45.1− vs CD45.1+CD45.2+ PB cells in CM examined at 1 to 3 months after the first transplantation (left) and at 1, 2, and 4 months after secondary transplantation (right; mean ± standard deviation [SD], n = 4-5). (D) The ratio of CD45.2+CD45.1− vs CD45.1+CD45.2+ in myeloid cells, B cells, and T cells in PB from first and second recipient mice were analyzed (mean ± SD, n = 4-5). The significant differences between the cells from ApcΔ/Δβ-cateninΔ/Δ and β-cateninΔ/Δ are indicated. (E) Lineage differentiation in the recipient mice transplanted with BM cells from Mx1-Cre Apcfl/flβ-cateninfl/fl, Mx1-Cre β-cateninfl/fl, or β-cateninfl/fl CM. Histogram shows percentage of donor-derived (CD45.2+CD45.1−) myeloid cells (Gr1+Mac+), B cells (B220+), and T cells (CD3+) in PB analyzed 2 and 4 months after the secondary transplantation (mean ± SD, n = 3-5). (F) Flow cytometric analysis of CD45.2+CD45.1− and CD45.1+CD45.2+ cells in LSK (lin−Sca-1+c-Kit+) and HSC (LSKCD34−) stem cell–enriched population in representative recipient mice. (G) The ratio of CD45.2+CD45.1− and CD45.1+CD45.2+ cells in total BM cells, Lin− cells, HPCs (lin-Sca-1−c-Kit+ cells), LSKs, and HSCs from the recipients 5 months after the first transplantation is shown (mean ± SD, n = 3). The significant differences between ApcΔ/Δβ-cateninΔ/Δ and β-cateninΔ/Δ or β-cateninfl/fl are indicated. *P < .05; **P < .01; ***P < .001.
HSCs with loss of both Apc and β-catenin show an enhanced repopulation capacity. (A) Diagram for the experimental design. CM were generated by transplanting an equal number of wild-type CD45.1+CD45.2+ BM cells (from primary mice) and CD45.2+ BM cells from Mx1-Cre Apcfl/flβ-cateninfl/fl, Mx1-Cre β-cateninfl/fl, or β-cateninfl/fl transplanted mice 2 months after induction. These transplanted mice have undergone 1 round of transplantation. (B) Flow cytometric analysis of CD45.2+CD45.1− (donor cells) and CD45.1+CD45.2+ (competitor cells) PB cells from representative CM 1 month after transplantation. The numbers indicate the percentage of cells in each population. (C) Histogram shows the relative ratio of CD45.2+CD45.1− vs CD45.1+CD45.2+ PB cells in CM examined at 1 to 3 months after the first transplantation (left) and at 1, 2, and 4 months after secondary transplantation (right; mean ± standard deviation [SD], n = 4-5). (D) The ratio of CD45.2+CD45.1− vs CD45.1+CD45.2+ in myeloid cells, B cells, and T cells in PB from first and second recipient mice were analyzed (mean ± SD, n = 4-5). The significant differences between the cells from ApcΔ/Δβ-cateninΔ/Δ and β-cateninΔ/Δ are indicated. (E) Lineage differentiation in the recipient mice transplanted with BM cells from Mx1-Cre Apcfl/flβ-cateninfl/fl, Mx1-Cre β-cateninfl/fl, or β-cateninfl/fl CM. Histogram shows percentage of donor-derived (CD45.2+CD45.1−) myeloid cells (Gr1+Mac+), B cells (B220+), and T cells (CD3+) in PB analyzed 2 and 4 months after the secondary transplantation (mean ± SD, n = 3-5). (F) Flow cytometric analysis of CD45.2+CD45.1− and CD45.1+CD45.2+ cells in LSK (lin−Sca-1+c-Kit+) and HSC (LSKCD34−) stem cell–enriched population in representative recipient mice. (G) The ratio of CD45.2+CD45.1− and CD45.1+CD45.2+ cells in total BM cells, Lin− cells, HPCs (lin-Sca-1−c-Kit+ cells), LSKs, and HSCs from the recipients 5 months after the first transplantation is shown (mean ± SD, n = 3). The significant differences between ApcΔ/Δβ-cateninΔ/Δ and β-cateninΔ/Δ or β-cateninfl/fl are indicated. *P < .05; **P < .01; ***P < .001.
Recently, Apc was shown to regulate directly GSK3 function. Loss of Apc reduced the phosphorylation of glycogen synthase, a direct GSK3 substrate, and activated the mTOR pathway in 293T cells.11 To determine whether loss of Apc also activates the mTOR pathway in hematopoietic cells, thereby contributing to depletion of Apc-deficient HSCs, we performed a western blot analysis of phosphorylated S6, a marker of mTOR activation, in Apc, Apc–β-catenin–deficient, and control BM and Lin− cells. Surprisingly, loss of Apc or both Apc and β-catenin had little effect on the expression and phosphorylation of S6 in BM and Lin− cells (supplemental Figure 9), indicating that loss of Apc probably does not activate the mTOR pathway in BM and Lin− cells. To rule out the possibility that loss of Apc could activate mTOR signaling in more primitive BM cells, we treated the Mx1-Cre Apcfl/fl mice with the mTOR inhibitor rapamycin. Similar to ApcΔ/Δ mice without rapamycin treatment, the rapamycin-treated ApcΔ/Δ mice became moribund due to BM failure within 2 to 3 weeks after Apc ablation, as revealed by significantly lower hematological parameters than normal controls (data not shown). Thus, inhibition of mTOR by rapamycin did not prevent ApcΔ/Δ mice from developing BM failure resulting from HSC exhaustion.
Discussion
We and others have previously demonstrated that Apc is a critical regulator of HSC/HPC function and that it plays a role in the pathogenesis of myeloid malignancies.5,,-8 However, the mechanisms responsible for the function of Apc in HSCs/HPCs remain obscure. In this study, we used a genetic approach to address the question of whether the function of Apc in HSCs/HPCs is solely or partially mediated by β-catenin.
Previous studies have shown that inhibition of Apc resulted in G2/M growth arrest, whereas overexpression of Apc led to arrest in G1/S phase in different cell types.27,,,,-32 However, the molecular mechanism underlying the role of Apc in cell cycle is poorly understood. Topoisomerase IIα binds Apc and has been implicated in mediating Apc-regulated G2/M cell cycle transition.32 It was also suggested that Apc controls G1/S transition possibly through β-catenin– and hDLG-dependent pathways.28,29 In HSCs/HPCs, we find that, although the loss of Apc leads to an increase of LSKs in both S phase and G2/M phase, it only affects the S phase of HPCs. We also showed that loss of β-catenin reduced the accumulation of Apc-deficient LSKs in both S phase and G2/M phase to a normal level, indicating that in hematopoietic primitive cells, Apc regulates both the S phase and G2/M transition of the cell cycle largely through the Wnt/β-catenin signaling. In addition, loss of β-catenin reverses the down-regulation of Cdkn1a and Cndk1b induced by Apc ablation in LSKs. Notably, constitutively active β-catenin was previously reported to inhibit Cdkn1a in LSKs.33 Thus, it is likely that the function of Apc in controlling the cell cycle of HSCs/HPCs may rely on β-catenin–mediated modulation of activity of the cyclin-CDK complex.
Apc is considered a negative regulator of apoptosis during neural cell development. It prevents neuronal apoptosis during retinal development in Drosophila.34 Apc ablation in the mouse results in apoptosis of a subset of neural crest derivatives.4 In agreement, we found that loss of Apc induces apoptosis in LSKs/HPCs. There are, however, controversies about the role of β-catenin in survival of HSCs/HPCs. Scheller et al35 showed that constitutively active β-catenin does not enhance apoptosis of LSKs. In contrast, recent studies revealed that activated β-catenin induces apoptosis in HSCs and HPCs.36,37 Of note, constitutively activated β-catenin also increases apoptotic death in crypt epithelial cells.38 In this study, we find that loss of β-catenin inhibits apoptosis induced by Apc ablation in LSKs and HPCs. In addition, loss of β-catenin suppresses down-regulation of the survival factor Mcl1 in Apc-deficient LSKs. Collectively, our data suggest that Apc is required to promote cell survival in different developmental contexts, and they also indicate that Apc regulates survival of HSCs/HPCs through the Wnt/β-catenin pathway.
In addition to regulating Wnt/β-catenin signaling, Apc was recently reported to negatively regulate mTOR in 293T cells and colorectal carcinoma cells.11,39 Of note, the mTOR signaling plays an important role in the maintenance of HSCs. Activation of mTOR induced by inactivation of Tsc1, Pten, or Gsk3β leads to deletion repression of HSCs, similar to the effects of to Apc ablation.20,40,-42 However, we found that loss of Apc does not activate the mTOR pathway in BM and Lin− cells and that the mTOR inhibitor rapamycin does not prevent Apc-deficient mice from developing BM failure.
Most importantly, in this study, we found that the loss of Apc in the absence of β-catenin enhances HSC repopulation. In agreement with previous studies,21,43 we show that Cre-mediated deletion of β-catenin has no effect on HSC function. Our findings indicate that multiple downstream targets of Apc including β-catenin contribute to Apc function in HSC self-renewal. Notably, Apc has multiple functions independent of Wnt/β-catenin signaling.13,14,44 Apc has been implicated in the regulation of asymmetric division of germ stem cell in Drosophila testes by controlling the orientation of spindle and centrosome.45 Whether loss of Apc in the mouse leads to asymmetric division of HSCs toward self-renewal as opposed to differentiation remains to be determined. DNA methylation plays a critical role in HSC self-renewal, as revealed by inactivation of DNA methyltransferase enzymes including Dnmt1, Dnmt3a, or Dnmt3b in HSCs.46,,-49 Dnmt1-null HSCs show premature exhaustion,46,47 whereas Dnmt3a-null HSCs display enhanced self-renewal and decreased differentiation capacity.49 Interestingly, a novel role of Apc in the regulation of DNA demethylase activity was identified recently by Rai et al.12 Additional studies are required to determine whether Apc affects function of HSC self-renewal by controlling DNA methylation dynamics in HSCs. Whether β-catenin can cross talk with additional pathway(s) activated by Apc loss is still unknown. One possibility is that β-catenin negatively regulates this pathway. After deletion of β-catenin, this pathway is activated by Apc loss and promotes HSC repopulation.
Although there are probably other pathways in addition to the Wnt/β-catenin pathway contributing to the regulation of HSC self-renewal by Apc, it seems more likely that activated Wnt/β-catenin signaling following Apc loss has dominant effects on the function of HSCs. Our studies provide genetic evidence suggesting that disruption of self-renewal capacity of HSCs following Apc loss is attributed to β-catenin–mediated up-regulation of proliferation and apoptosis in HSCs.
The online version of this article contains a data supplement.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 USC section 1734.
Acknowledgments
The authors thank the staff at the University of Illinois at Chicago flow core facility for assistance in cell sorting.
This work was supported by National Institutes of Health Cancer Institute grant RO1 CA140979 (to Z.Q.).
Authorship
Contribution: W.L., Y.H., M.M., and A.S. performed research; Z.Q. and W.L. designed research and performed data analysis; L.Y. contributed new reagents/analytic tools; and Z.Q., W.L., and A.S. wrote the paper.
Conflict-of-interest disclosure: The authors declare no competing financial interests.
Correspondence: Zhijian Qian, Department of Medicine and the Cancer Research Center, University of Illinois at Chicago, 909 S. Wolcott Ave, COMRB Room 5051 M/C704, Chicago, IL 60612; e-mail: zjqian@uic.edu.


![Figure 4. Loss of β-catenin prevents rapid exhaustion of Apc-deficient HSCs in vivo. (A) Flow cytometric analysis of the frequency of stem cell-enriched population (Lin-c-Kit+Sca+ [LSK]) and HSCs (LSK CD150+CD48−) in BM from representative ApcΔ/Δ and ApcΔ/Δβ-cateninΔ/Δ mice 10-14 days after induction. (B-D) The histograms depict the total number of HSCs in BM (B) from ApcΔ/Δ and ApcΔ/Δβ-cateninΔ/Δ mice 10-14 days after induction (mean ± standard deviation [SD], n = 5-8), (C) from ApcΔ/Δβ-cateninΔ/Δ, β-cateninΔ/Δ, and β-cateninfl/fl mice 5 weeks after induction (mean ± SD, n = 3), and (D) from ApcΔ/Δβ-cateninΔ/Δ (6 months after induction) and Mx1-Cre Apcfl/flβ-cateninfl/fl (mean ± SD, n = 2-4). *P < .05; ***P < .001.](https://ash.silverchair-cdn.com/ash/content_public/journal/blood/121/20/10.1182_blood-2012-12-473470/2/m_4063f4.jpeg?Expires=1765067649&Signature=tKCUOc-fOlBIvz3IOd8rqpIcuiSbsDELfTOSg9MW5~mxllq-hz0~y0TEb-zfzS6n0VRdr9nakH-XaMWo95apTyPNwoRXCmXWDBCef6WolzxMjO-hqK~3jjvbxd6HQ2Nvqc1PCAlYjodFHfc8rYpSS6A~eLmWyDgdzIS1qEnoDWKohfstG-V3o5AlmTfLA0oSogbuh9J9YFSmujQHutynzRDB64CsWP0VqQwzxHiBMMxrt0FtZtcejhwSixRw7Hl6el4whT-8HoshswNVjiBLy2uBT92sqYnBtOkLEkmqHjxsLrU62~HQ04ulDnSMYC-vuSE~Gasao0dagLN5qJL3uQ__&Key-Pair-Id=APKAIE5G5CRDK6RD3PGA)
![Figure 5. Loss of β-catenin suppresses elevated proliferation and apoptosis in Apc-deficient HPCs and LSKs in vivo. (A) Analysis of cell cycle status of LSKs and HPCs in BM from Mx1-Cre Apcfl/fl and Mx1-Cre Apcfl/flβ-cateninfl/fl mice 4 days after pI-pC injection. BrdU was injected into mice 24 hours before analysis (mean ± standard deviation [SD]; n = 3-4). (B) Histograms depict the mean distribution of cell cycle phases of HPCs and LSKs in BM from ApcΔ/Δβ-cateninΔ/Δ, β-cateninΔ/Δ, and β-cateninfl/fl 5 weeks after induction (mean ± SD; n = 3-4). (C) Analysis of frequency of apoptosis in HPCs and LSKs in BM from Mx1-Cre Apcfl/fl and Mx1-Cre Apcfl/flβ-cateninfl/fl mice 2 weeks after pI-pC injection (mean ± SD; n = 3-4). (D) Histograms depict the mean frequency of apoptosis of HPCs and LSKs from ApcΔ/Δβ-cateninΔ/Δ, β-cateninΔ/Δ, and β-cateninfl/fl 5 weeks after induction (mean ± SD; n = 3-4). *P < .05; **P < .01; ***P < .001. (E) Analysis of gene expression in Apc fl/fl, Apc-deficient, β-catenin–deficient, and Apc–β-catenin–deficient LSKs by quantitative PCR. The LSKs were isolated from the mice 4 days after induction. Cdkn1a, Cdkn1b, and Mcl1 are expressed at comparable levels in LSKs from β-cateninΔ/Δ and ApcΔ/Δβ-cateninΔ/Δ. Gene expression is normalized initially to actin expression. In β-catenin–deficient and Apc–β-catenin–deficient LSKs, values represent fold changes in gene expression relative to Cdkn1a in β-catenin–deficient LSKs (mean ± SD of 3 mice), whereas in Apcfl/fl and Apc-deficient LSKs, values indicate the fold changes in gene expression relative to Cdkn1a in Ap fl/fl LSKs (mean ± SD of 3-6 mice). *P < .05.](https://ash.silverchair-cdn.com/ash/content_public/journal/blood/121/20/10.1182_blood-2012-12-473470/2/m_4063f5.jpeg?Expires=1765067649&Signature=IouxdvU5F0mRBApPTN-t-99hK~KO6Vg0dhcPUjeq5exRcMBp1LtdKftzVBiUlXFZh-fYUHtD43A00r-ApRFlyDUocQhMD2nU9JInpLD3KXsCiUY--759YjAvjcQZyouQGcJr8eijHxZZCqtIN6h9m0ALhDXgDSWNIS5705TCEWof9O9MHmVjjznXP9yIp8HJPfHUFKb~2LF~k4OmazN9sxXj9bZbdV-odabryLW8G0aqR4r3iivrsOTk~dVQPpRoWDM88xzLRDSKykPri2maNAJhn4tteChE89Z5~VjBjcO4NtV0f890ikxCkwTMLr-1uhz--OB~duKuj97AdCx-wA__&Key-Pair-Id=APKAIE5G5CRDK6RD3PGA)
![Figure 6. HSCs with loss of both Apc and β-catenin show an enhanced repopulation capacity. (A) Diagram for the experimental design. CM were generated by transplanting an equal number of wild-type CD45.1+CD45.2+ BM cells (from primary mice) and CD45.2+ BM cells from Mx1-Cre Apcfl/flβ-cateninfl/fl, Mx1-Cre β-cateninfl/fl, or β-cateninfl/fl transplanted mice 2 months after induction. These transplanted mice have undergone 1 round of transplantation. (B) Flow cytometric analysis of CD45.2+CD45.1− (donor cells) and CD45.1+CD45.2+ (competitor cells) PB cells from representative CM 1 month after transplantation. The numbers indicate the percentage of cells in each population. (C) Histogram shows the relative ratio of CD45.2+CD45.1− vs CD45.1+CD45.2+ PB cells in CM examined at 1 to 3 months after the first transplantation (left) and at 1, 2, and 4 months after secondary transplantation (right; mean ± standard deviation [SD], n = 4-5). (D) The ratio of CD45.2+CD45.1− vs CD45.1+CD45.2+ in myeloid cells, B cells, and T cells in PB from first and second recipient mice were analyzed (mean ± SD, n = 4-5). The significant differences between the cells from ApcΔ/Δβ-cateninΔ/Δ and β-cateninΔ/Δ are indicated. (E) Lineage differentiation in the recipient mice transplanted with BM cells from Mx1-Cre Apcfl/flβ-cateninfl/fl, Mx1-Cre β-cateninfl/fl, or β-cateninfl/fl CM. Histogram shows percentage of donor-derived (CD45.2+CD45.1−) myeloid cells (Gr1+Mac+), B cells (B220+), and T cells (CD3+) in PB analyzed 2 and 4 months after the secondary transplantation (mean ± SD, n = 3-5). (F) Flow cytometric analysis of CD45.2+CD45.1− and CD45.1+CD45.2+ cells in LSK (lin−Sca-1+c-Kit+) and HSC (LSKCD34−) stem cell–enriched population in representative recipient mice. (G) The ratio of CD45.2+CD45.1− and CD45.1+CD45.2+ cells in total BM cells, Lin− cells, HPCs (lin-Sca-1−c-Kit+ cells), LSKs, and HSCs from the recipients 5 months after the first transplantation is shown (mean ± SD, n = 3). The significant differences between ApcΔ/Δβ-cateninΔ/Δ and β-cateninΔ/Δ or β-cateninfl/fl are indicated. *P < .05; **P < .01; ***P < .001.](https://ash.silverchair-cdn.com/ash/content_public/journal/blood/121/20/10.1182_blood-2012-12-473470/2/m_4063f6.jpeg?Expires=1765067649&Signature=s0MOZ58zYh6K17wV7iaOhppx166yQ43rbvdLT-vZmzoqEu1RkvUDW2oxNrwzs7XyWuZbwNM1jNc9KHVGAlNdYvy7HojHLEjb07aExC8vN1Xg1Dt8Fgvxc9HkZ4dVf2d~AK5PK~Kh~MWrK6HN6oQCD0GZZv19OhI2DNL62zzq6Rj8BP1xVNB41HnnIF6C2ba7whUG8RIdCmhfLWhiBUThLSqS0Tffa~YXZ1u4kLAFlNWbjqYvMhAcVdJOjRgqvQYoPj3Xp6~t3LVO0iBrRy2kdTpmcrS2s8yFHuxqXU5gKjbkeZmvlSwjYxVo~xeggq1uUHp54ASCEyLZA3MBofo0cg__&Key-Pair-Id=APKAIE5G5CRDK6RD3PGA)
This feature is available to Subscribers Only
Sign In or Create an Account Close Modal