Key Points
Presents the data from a phase 2 clinical trial of panobinostat in patients with relapsed WM.
Establishes a role for histone deacetylase inhibitors as an active class of therapeutic agents in WM.
Abstract
The present study aimed to determine the safety and activity of the histone deacetylase inhibitor panobinostat in patients with relapsed/refractory Waldenström macroglobulinemia (WM). Eligibility criteria included patients with relapsed/refractory WM with any number of prior therapies. Patients received panobinostat at 30 mg 3 times a week; 12 of 36 (33%) patients were enrolled at 25 mg dose. A total of 36 patients received therapy. The median age was 62 years (range, 47-80) and the median number of prior therapies was 3 (range, 1-8). All of the patients had received prior rituximab. Minimal response (MR) or better was achieved in 47% of patients (90% confidence interval [CI], 33-62), with 22% partial remissions and 25% MR. In addition, 18 (50%) patients achieved stable disease and none showed progression while on therapy. The median time to first response was 1.8 months (range, 1.7-3.2). The median progression-free survival was 6.6 months(90% CI, 5.5-14.8). Grade 3 and 4 toxicities included thrombocytopenia (67%), neutropenia (36%), anemia (28%), leukopenia (22%), and fatigue (11%). We conclude that panobinostat is an active therapeutic agent in patients with relapsed/refractory WM. This study (www.clinicaltrials.gov identifier: NCT00936611) establishes a role for histone deacetylase inhibitors as an active class of therapeutic agents in WM.
Introduction
Waldenström macroglobulinemia (WM) is a low-grade lymphoplasmacytic lymphoma characterized by the presence of an IgM monoclonal protein in the serum.1-4 Patients typically present with symptoms related to cytopenias, mainly anemia or symptoms related to hyperviscosity.1-4 Many patients have an indolent disease with a median overall survival of 5 years; however, some patients with high-risk features have a 5-year survival of only 36%.2,3,5,6
Standard therapeutic agents currently used in the treatment of WM include alkylating agents, rituximab, nucleoside analogs, and stem cell transplantation. Many new agents have been investigated recently in WM, including bortezomib, lenalidomide, perifosine, everolimus, and bendamustine. However, most patients show disease relapse after treatment with these agents or have significant toxicities, including prolonged myelosuppression or neuropathy. Therefore, there is an urgent need to develop therapies that are beneficial for this unique population of patients.
Epigenetic alterations including methylation and histone acetylation are commonly deregulated in most cancers.7,8 Histone acetylation is regulated by a tight balance between histone deacetylase (HDAC) and histone acetyl transferases.9 This balance is disrupted in many malignancies, leading to increased expression of HDACs and a more open chromatin structure that induces activation of gene transcription.
We and others have shown previously that miRNAs are also deregulated in WM.10,11 Our data indicated that aberrant increased expression of miRNA-206 and reduced expression of miRNA-9* leads to activation of HDACs in WM. We also showed that HDACs and histone acetyl transferases are unbalanced in WM, with a decreased acetylated histone H3 and H4 and increased HDAC activity in primary tumor cells compared with their normal cellular counterparts. Using the novel cinnamic hydroxamic acid HDAC inhibitor panobinostat (LBH589; Novartis), we confirmed that this agent induces significant cytotoxicity in vitro and in vivo in WM cells.
Based on these promising preclinical studies, we designed the present phase 2 clinical trial of single-agent panobinostat to examine the response rate, toxicity, and progression-free survival (PFS) in patients with relapsed or relapsed/refractory WM.
Methods
Eligibility
Study participants were at least 18 years of age and had symptomatic disease requiring therapy according to the consensus recommendations for WM.12 Patients had a measurable monoclonal IgM concentration shown by serum electrophoresis, IgM protein twice the upper limit of normal shown by nephelometry, and evidence of lymphoplasmacytic cells in the BM. Patients who had at least 1 previous therapy for WM and were relapsed or refractory were eligible. Any number of prior therapies was permissible. Patients must have had symptomatic disease requiring therapy to be entered in the study. Eligibility criteria also included a serum concentration of aspartate transaminase or alanine aminotransferase < 3 times the upper limit of the normal range, a serum total bilirubin < 2 mg/dL, a measured creatinine < 3.5 times the upper limit of the normal range, a platelet count of ≥ 75 000/mL, and an absolute neutrophil count of ≥ 1.0 × 109/L. All patients gave written informed consent before entering the study, which was performed in accordance with the Declaration of Helsinki. Approval was obtained from the institutional review board at each of the participating centers. This trial is registered at www.clinicaltrials.gov as NCT00936611.
Study design and treatment
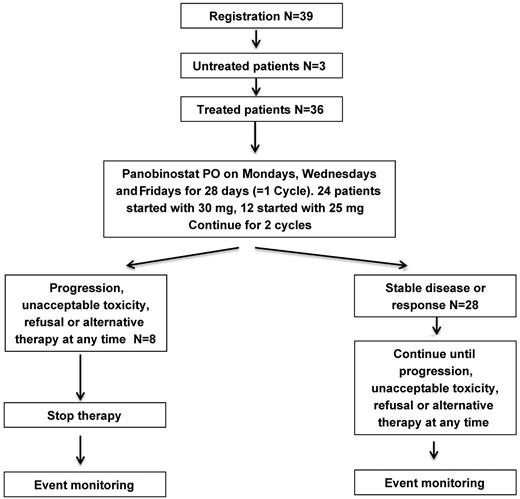
Patients received single-agent oral panobinostat 30 mg 3 days a week (Mondays, Wednesdays, and Fridays). A cycle was 28 days. Patients with progressive disease (PD) after 2 cycles were taken off of therapy. Patients with stable or responsive disease continued on therapy (see Figure 1 CONSORT diagram). Restaging with a BM biopsy and CT scans were performed at the end of cycle 6.
Dose modifications for attributable toxicities were allowed. Panobinostat could be reduced to 25 mg, 20 mg 3 times a week every week, or 20 mg 3 times a week every other week. No dose reescalation was allowed. Dexamethasone was not allowed on this protocol. The protocol was amended because of concerns of toxicity to allow a starting dose of 25 mg; 12 of 36 (33%) patients were given the 25-mg dose.
Efficacy and safety assessments
Tumor assessment was performed using the consensus panel recommendations.13 Patients were assessed every 28 days during the 6 cycles of therapy and every 3 months thereafter. Patients who came off therapy were monitored every 3 months until they progressed, were treated with another therapy, or died.
Response was calculated from the M spike measurement (or IgM measurement) of cycle 1 on day 1 before therapy. Response was determined based on the International Workshop on Waldenstrom's Macroglobulinemia response criteria,13 including CT scan and BM assessment. All responses were confirmed. Partial remission (PR) was assessed as a 50% reduction in pathologic lymph nodes. Adverse events were assessed at each visit and graded according to the National Cancer Institute Common Toxicity Criteria (Version 3.0) from the first dose until 30 days after the last dose of therapy.
Statistical analysis
The primary end point was the overall response rate (defined as minimal response [MR] or better) and secondary end points included safety, duration of response, time to progression (TTP), and PFS. This study used a 2-stage design (14 patients were eligible on the first stage, 3 responses were required to continue to the second stage with 23 eligible patients) with at least 11 MRs or better observed among the 37 eligible patients for the study drug to be considered promising. This study design has 0.93 probability of concluding that the drug is promising assuming true underlying MR or better response of 40% and less than 0.10 probability assuming a 20% promising rate. Patient baseline characteristics were summarized as number (%) of patients for categorical end points or median (range) of values for continuous end points. Exact 2-stage binomial 90% confidence intervals (CIs) were reported for response. Exact binomial 90% CIs were reported for toxicity percentages. Comparisons between groups were performed using the Fisher exact test for binary end points and the Wilcoxon rank-sum test for continuous end points. Median time to event end points was estimated using the Kaplan-Meier method. Duration of response was measured from response to first PD or death, censored at the date patients were last known to be event-free and alive for those who had not failed. TTP, PFS, and event-free survival (EFS) are measured from the time of treatment initiation to event (PD for TTP; PD or death for PFS; and PD, death, or nonprotocol therapy for EFS). Patients without event were censored at the date they were last known to be progression free for TTP and progression-free and alive for PFS and EFS. In addition, patients who started nonprotocol therapy before progression were censored at the date of nonprotocol therapy initiation for TTP and PFS and this was considered an event for EFS. All P values are 2-sided. Statistical analyses were performed using SAS Version 9.2 statistical software (SAS Institute).
Correlative studies
PBMCs were obtained from patients before therapy (at screening or on day 1 of cycle 1; n = 11 samples). In addition, samples were also obtained after cycle 3 or cycle 6 in some patients (n = 3). The level of acetylated histone 3 was measured using ELISA (Cell Signaling Technology) in these samples, as described previously.10
BM biopsies from 14 patients at pretreatment or after therapy were fixed in Zenker formalin, embedded in paraffin blocks, and sectioned. Sections were stained for CD20 and κ and λ light chains (Cell Signaling Technology).
Results
Patients and treatments
From July 2009 to March 2011, 39 patients were enrolled; 36 started on active therapy in 2 centers and 3 patients were found to be ineligible and were not initiated on therapy (Figure 1 CONSORT diagram). Table 1 shows selected characteristics of all 36 patients. The median age at enrollment was 61.6 years (range, 47-79.8). The median IgM level at enrollment was 3240 mg/dL (range, 804-10 300), and the median M spike by serum protein electrophoresis was 2.06 g/dL (range, 0.63-5.1). The median hemoglobin at enrollment was 10.7 g/dL (range, 8.2-14.5), with 58.3% (n = 21) of the patients having anemia (< 11 g/dL). The median beta-2 microglobulin at enrollment was 3.3 mg/dL (range, 1.5-7.4), with 47.2% (n = 17) of the patients having > 3.5 mg/dL. The median percentage of BM involvement was 70% (range, 5-100), with 10 patients (27.8%) having more than 70% involvement in the BM. Twenty-one (58%) of the patients were considered intermediate or high risk by the International Staging System for Waldenström Macroglobulinemia (ISS-WM) staging system at the time of enrollment. All patients had symptomatic disease requiring initiation of therapy based on consensus recommendations for WM.
Baseline characteristics (N = 36)
| Characteristic . | . |
|---|---|
| Median age, y (range) | 61.6 (47-80) |
| Male sex, n (%) | 22 (61%) |
| White race, n (%) | 35 (97%) |
| Median IgM at screening, mg/dL (range) | 3240 (804-10 300) |
| Median M spike at screening, g/dL (range) | 2.06 (0.63-5.1) |
| Median hemoglobin, g/dL, (range) | 10.7 (8.2-14.5) |
| Median platelet count, n (range) | 242 (74-388) |
| Median beta-2 microglobulin, mg/dL (range) | 3.3 (1.4-7.4) |
| BM involvement, % (range) | 70 (5-100) |
| Lymph nodes and HSM assessment by CT scan, n (%) | |
| Evidence of disease | 29 (81%) |
| ISS-WM at enrollment, n (%) | |
| High risk | 7 (19%) |
| Intermediate risk | 14 (39%) |
| Low risk | 15 (42%) |
| Characteristic . | . |
|---|---|
| Median age, y (range) | 61.6 (47-80) |
| Male sex, n (%) | 22 (61%) |
| White race, n (%) | 35 (97%) |
| Median IgM at screening, mg/dL (range) | 3240 (804-10 300) |
| Median M spike at screening, g/dL (range) | 2.06 (0.63-5.1) |
| Median hemoglobin, g/dL, (range) | 10.7 (8.2-14.5) |
| Median platelet count, n (range) | 242 (74-388) |
| Median beta-2 microglobulin, mg/dL (range) | 3.3 (1.4-7.4) |
| BM involvement, % (range) | 70 (5-100) |
| Lymph nodes and HSM assessment by CT scan, n (%) | |
| Evidence of disease | 29 (81%) |
| ISS-WM at enrollment, n (%) | |
| High risk | 7 (19%) |
| Intermediate risk | 14 (39%) |
| Low risk | 15 (42%) |
HSM indicates hepatosplenomegaly.
The median number of prior therapies was 3 (range, 1-8). Prior therapies included rituximab in all 36 patients (100%), nucleoside analogs including fludarabine or cladribine in 11 patients (31%), alkylating agents including chlorambucil and cyclophosphamide alone or in combination with other agents in 10 patients (28%), bortezomib-containing regimens in 20 patients (56%), and other therapies including thalidomide, imatinib mesylate, everolimus, and radiation therapy in 20 patients (56%).
Of the 36 patients, the median number of completed cycles of therapy was 5 (range, 0-32). There were 7 patients still on active therapy as of March 2012. Of these, 26 patients (72%) received at least 1 dose modification and the median number of treatment cycles without dose modifications was 1 (range, 0-11). The protocol was amended to allow a starting dose of 25 mg; 12 of 36 (36%) patients were enrolled in the 25 mg group.
Of the 12 patients who were treated with the 25-mg dose, 7 (58%) had dose reductions; of those who received 30 mg (n = 24), 19 (79%) had dose reductions. The median number of days that patients remained on the 30-mg dosing schedule was 61 days (range, 7-321); the median number of days that patients started on the 25-mg dose stayed on this dose was 38 (range, 11-97). The median number of dose reductions for those started on 30 mg was 2 (range, 0-3), whereas that of those started on 25 mg was 1 (range, 0-2). The median total amount of drug received for those who were started on the 30-mg dose was 1263 mg (range, 210-1185), whereas the median total amount of drug received by those who started at 25 mg was 740 mg (range, 175-3520).
At the time of this analysis (March 2012), 8 patients remained on study follow up (7 on active therapy), and the remaining 28 patients were off study for the following reasons: 3 due to PD (11%), 22 due to new systemic therapy (61%), 1 was lost to follow-up (3%), and 2 patients withdrew from the study (5%).
Efficacy
Using the uniform WM response criteria,13 which includes monoclonal M spike and CT scans for measuring organ and lymph node involvement, the following responses were observed. Of the 36 patients, 8 achieved a PR (22%), and 9 achieved MR (25%), with an overall response rate of 17 of 36 (47%; 90% CI, 33-62; Table 2). Stable disease (SD) was achieved in 18 (50%) of the patients and 1 (3%) patient was not evaluable because he did not complete the first cycle and did not have M spike measurements after the initiation of therapy. The median time to first response (n = 17) was 1.7 months (range, 0.9-1.8) and the time to best response (n = 17) was 1.8 months (range, 1.7-3.2). The duration of response (MR or better) was 18.9 months (range, 4.8-not reached).
Response measured by response assessment per protocol and by paraprotein (M spike) measurement based on the starting dose of 30 or 25 mg
| . | All patients, N = 36 (%) . | 30 mg, n = 24 (%) . | 25 mg, n = 12 (%) . |
|---|---|---|---|
| Best overall response, n (%) | |||
| CR | 0 (0) | 0 (0) | 0 (0) |
| VGPR | 0 (0) | 0 (0) | 0 (0) |
| PR | 8 (22) | 7 (29) | 1 (8) |
| MR | 9 (25) | 5 (21) | 4 (33) |
| SD | 18 (50) | 11 (46) | 8 (58) |
| PD | 0 (0) | 0 (0) | 0 (0) |
| Not evaluable | 1 (3) | 1 (4) | 0 (0) |
| Total | 36 | 24 | 12 |
| PR or better | 8 (22; 90% CI,12-37) | 7 (29; 90% CI, 15-48) | 1 (8; 90% CI, 0-34) |
| MR or better | 17 (47; 90% CI, 33-62) | 12 (50; 90% CI, 32-68) | 5 (41; 90% CI, 18-68) |
| Best paraprotein response, n (%) | |||
| CR | 0 (0) | 0 (0) | 0 (0) |
| VGPR | 1 (3) | 1 (4) | 0 (0) |
| PR | 10 (27) | 9 (38) | 1 (8) |
| MR | 9 (25) | 5 (21) | 4 (33) |
| SD | 14 (39) | 7 (29) | 7 (58) |
| PD | 1 (3) | 1 (4) | 0 (0) |
| Not evaluable | 1 (3) | 1 (4) | 0 (0) |
| Total | 36 | 24 | 12 |
| PR or better | 11 (30; 90% CI, 18-46) | 10 (42; 90% CI, 25-60) | 1 (8; 90% CI, 0-34) |
| MR or better | 20 (55; 90% CI, 41-70) | 15 (63; 90% CI, 44-79) | 5 (41; 90% CI, 18-68) |
| . | All patients, N = 36 (%) . | 30 mg, n = 24 (%) . | 25 mg, n = 12 (%) . |
|---|---|---|---|
| Best overall response, n (%) | |||
| CR | 0 (0) | 0 (0) | 0 (0) |
| VGPR | 0 (0) | 0 (0) | 0 (0) |
| PR | 8 (22) | 7 (29) | 1 (8) |
| MR | 9 (25) | 5 (21) | 4 (33) |
| SD | 18 (50) | 11 (46) | 8 (58) |
| PD | 0 (0) | 0 (0) | 0 (0) |
| Not evaluable | 1 (3) | 1 (4) | 0 (0) |
| Total | 36 | 24 | 12 |
| PR or better | 8 (22; 90% CI,12-37) | 7 (29; 90% CI, 15-48) | 1 (8; 90% CI, 0-34) |
| MR or better | 17 (47; 90% CI, 33-62) | 12 (50; 90% CI, 32-68) | 5 (41; 90% CI, 18-68) |
| Best paraprotein response, n (%) | |||
| CR | 0 (0) | 0 (0) | 0 (0) |
| VGPR | 1 (3) | 1 (4) | 0 (0) |
| PR | 10 (27) | 9 (38) | 1 (8) |
| MR | 9 (25) | 5 (21) | 4 (33) |
| SD | 14 (39) | 7 (29) | 7 (58) |
| PD | 1 (3) | 1 (4) | 0 (0) |
| Not evaluable | 1 (3) | 1 (4) | 0 (0) |
| Total | 36 | 24 | 12 |
| PR or better | 11 (30; 90% CI, 18-46) | 10 (42; 90% CI, 25-60) | 1 (8; 90% CI, 0-34) |
| MR or better | 20 (55; 90% CI, 41-70) | 15 (63; 90% CI, 44-79) | 5 (41; 90% CI, 18-68) |
Response using the monoclonal protein M spike level was as follows: 1 patient (3%) achieved a very good partial remission (VGPR), 10 (27%) patients achieved PR, 9 patients (25%) achieved MR, 1 patient (3%) showed PD, and 1 patient was not evaluable, thus yielding a response rate of MR or better of 20 of 36 (56%, 90% CI, 41-70) and of PR or better of 11 of 36 (31%, 90% CI, 18-46).
Using IgM response evaluated by nephelometry, 19 patients (53%) achieved at least MR or better (90% CI, 38%-67%), and 12 patients (33%) achieved PR or better (90% CI, 21-48), with 1 (4%) VGPR, 11 (31%) PR, and 7 (19%) MR. Figure 2 shows the maximum percent change from baseline in IgM over all cycles among all patients.
Waterfall of the maximum difference in IgM from baseline throughout the study (including follow-up; N = 36).
Waterfall of the maximum difference in IgM from baseline throughout the study (including follow-up; N = 36).
BM biopsies were performed, and results were available before and after therapy (after at least 6 cycles of therapy) in 20 (56%) patients. Of these, 12 patients (60%) showed a reduction in the percentage involvement of BM after therapy, with a median decrease of 63% (range, 20%-94%). The response was MR or better in 17 of 20 (85%) patients, and 3 patients showed SD by response criteria. Among the other 8 patients with no change in the BM involvement or increase in BM involvement, the median increase was 11% (range, 0%-300%). The increase in 300% was in a patient with a percent increase from 5%-20% in his pre- and posttreatment samples, respectively. The responses in these 8 patients included 2 PRs, 3MRs, and 3 SDs by response criteria.
Given that 23 patients were initiated on therapy at the 30-mg dose, which was then reduced because of toxicity, and another 12 patients were initiated on therapy at the 25-mg starting dose, we reported on the response rates of the patients initiated on both the 30- and the 25-mg dose (Table 2). The overall response rate and response rate by best paraprotein in all 36 patients and in those patients treated with 30 or 25 mg dosing of panobinostat is reported in Table 2.
TTP and PFS
After a median follow-up of 7.7 months (90% CI, 6.8-9.5), 24 patients had progressed; of these, 1 subsequently died and 14 were alive at the time of this analysis. Among the other 12, 4 started a new therapy and 1 patient died without documented disease assessment of progression, measured as 25% progression in the paraprotein.
The 2 deaths occurred off therapy and after receiving subsequent therapy. Both patients died with large-cell transformation and PD. One patient received 16 cycles of therapy and then showed progression and went on to another therapy. The patient then developed infections and large-cell transformation and died 6 months after being started on panobinostat. The second patient received 2 cycles of therapy and then withdrew consent. The patient had another therapy and also showed large-cell transformation and died 7 months after being entered into the clinical trial.
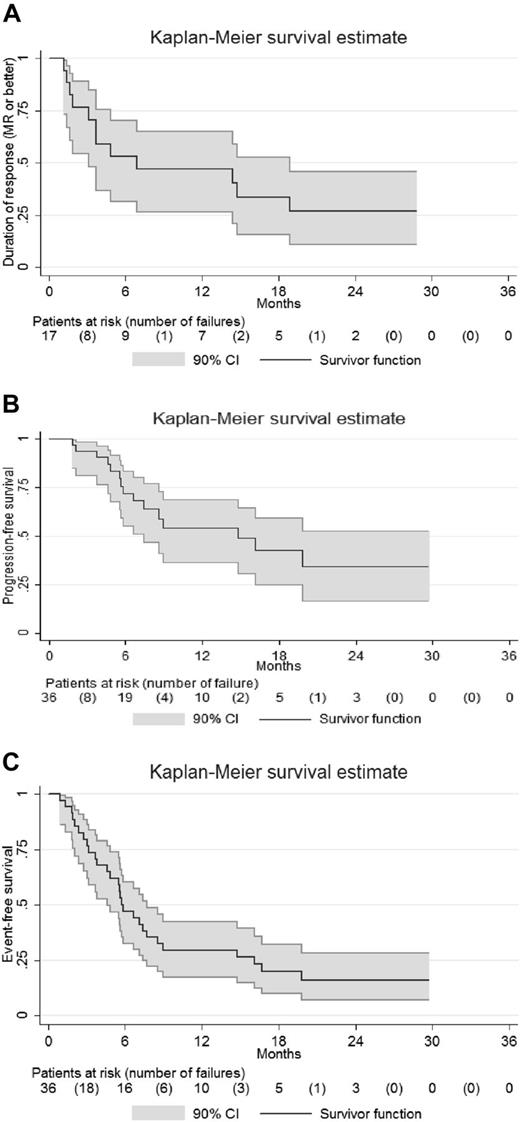
The median duration of response (MR or better, n = 17) was 6.9 months (90% CI, 3.1-18.9; Figure 3A). The TTP and PFS were similar in the 36 patients who were followed up: 6.6 months (90% CI, 5.5-14.8; Figure 3B). In the TTP and PFS analysis, patients who started nonprotocol therapy before progression (n = 4) were censored at the initiation of nonprotocol treatment. For the EFS analysis, in which the initiation of nonprotocol therapy is counted as an event, the median EFS time was 5.8 months (90% CI, 4.6-7.7; Figure 3C). The estimated 1-year EFS was 31% (90% CI, 19%-44%). The estimated EFS at 2 years was 17% (90% CI, 7%-29%).
Duration of response, progression-free, and event-free survival in patients treated with panobinostat. (A) Kaplan-Meier estimation of the duration of response (MR or better) end point (n = 17). (B) Kaplan-Meier estimation of the PFS end point (n = 36): PFS was similar to TTP. (C) Kaplan-Meier estimation of the EFS end point (n = 36).
Duration of response, progression-free, and event-free survival in patients treated with panobinostat. (A) Kaplan-Meier estimation of the duration of response (MR or better) end point (n = 17). (B) Kaplan-Meier estimation of the PFS end point (n = 36): PFS was similar to TTP. (C) Kaplan-Meier estimation of the EFS end point (n = 36).
Safety
A summary of all toxicities related to therapy is shown in Table 3. The most common grade 3 and 4 therapy-related adverse events included thrombocytopenia in 67%, neutropenia in 36%, anemia in 28%, leukopenia in 22%, fatigue in 11%, and syncope in 6%. Grade 1 and 2 diarrhea occurred in 58%, nausea and anorexia in 44%, taste disturbance in 28%, lower extremity edema in 22%, weight loss in 22%, dizziness in 19%, dyspnea in 19%, and alopecia in 17%. Pneumonitis occurred in 5 patients, 4 grade 1 and 1 grade 2 toxicity. All of these events were observed incidentally with CT scans performed during staging studies in follow-up during therapy. Pneumonitis was treated with tapering doses of steroids and by withholding therapy and reinitiating it at a dose reduction.
Summary of all adverse events > 10% of patients with at least possible attribution (N = 36)
| Toxicity type, n . | Maximum grade . | Total . | All grades, % . | Grade 1 and 2, % . | Grade 3 and 4, % . | |||
|---|---|---|---|---|---|---|---|---|
| 1 . | 2 . | 3 . | 4 . | |||||
| Fatigue | 4 | 22 | 4 | 0 | 30 | 83 | 72 | 11 |
| Platelets | 0 | 4 | 15 | 9 | 28 | 78 | 11 | 67 |
| Neutrophils | 0 | 12 | 9 | 4 | 25 | 69 | 33 | 36 |
| Diarrhea | 10 | 11 | 0 | 0 | 21 | 58 | 58 | 0 |
| Leukocytes | 0 | 12 | 6 | 2 | 20 | 56 | 33 | 22 |
| Hemoglobin | 0 | 8 | 8 | 2 | 18 | 50 | 22 | 28 |
| Nausea | 11 | 4 | 1 | 0 | 16 | 44 | 42 | 3 |
| Anorexia | 7 | 8 | 0 | 0 | 15 | 42 | 42 | 0 |
| Taste disturbance | 7 | 3 | 0 | 0 | 10 | 28 | 28 | 0 |
| Dizziness | 7 | 0 | 0 | 0 | 7 | 19 | 19 | 0 |
| Dyspnea | 5 | 2 | 0 | 0 | 7 | 19 | 19 | 0 |
| Edema limb | 6 | 1 | 0 | 0 | 7 | 19 | 19 | 0 |
| Weight loss | 6 | 1 | 0 | 0 | 7 | 19 | 19 | 0 |
| Abdominal pain | 4 | 2 | 0 | 0 | 6 | 17 | 17 | 0 |
| Headache | 3 | 3 | 0 | 0 | 6 | 17 | 17 | 0 |
| Vomiting | 5 | 1 | 0 | 0 | 6 | 17 | 17 | 0 |
| Alopecia | 5 | 0 | 0 | 0 | 5 | 14 | 14 | 0 |
| Creatinine | 0 | 5 | 0 | 0 | 5 | 14 | 14 | 0 |
| Pneumonitis | 4 | 1 | 0 | 0 | 5 | 14 | 14 | 0 |
| Constipation | 4 | 0 | 0 | 0 | 4 | 11 | 11 | 0 |
| Dry mouth | 4 | 0 | 0 | 0 | 4 | 11 | 11 | 0 |
| Dyspepsia | 2 | 2 | 0 | 0 | 4 | 11 | 11 | 0 |
| Toxicity type, n . | Maximum grade . | Total . | All grades, % . | Grade 1 and 2, % . | Grade 3 and 4, % . | |||
|---|---|---|---|---|---|---|---|---|
| 1 . | 2 . | 3 . | 4 . | |||||
| Fatigue | 4 | 22 | 4 | 0 | 30 | 83 | 72 | 11 |
| Platelets | 0 | 4 | 15 | 9 | 28 | 78 | 11 | 67 |
| Neutrophils | 0 | 12 | 9 | 4 | 25 | 69 | 33 | 36 |
| Diarrhea | 10 | 11 | 0 | 0 | 21 | 58 | 58 | 0 |
| Leukocytes | 0 | 12 | 6 | 2 | 20 | 56 | 33 | 22 |
| Hemoglobin | 0 | 8 | 8 | 2 | 18 | 50 | 22 | 28 |
| Nausea | 11 | 4 | 1 | 0 | 16 | 44 | 42 | 3 |
| Anorexia | 7 | 8 | 0 | 0 | 15 | 42 | 42 | 0 |
| Taste disturbance | 7 | 3 | 0 | 0 | 10 | 28 | 28 | 0 |
| Dizziness | 7 | 0 | 0 | 0 | 7 | 19 | 19 | 0 |
| Dyspnea | 5 | 2 | 0 | 0 | 7 | 19 | 19 | 0 |
| Edema limb | 6 | 1 | 0 | 0 | 7 | 19 | 19 | 0 |
| Weight loss | 6 | 1 | 0 | 0 | 7 | 19 | 19 | 0 |
| Abdominal pain | 4 | 2 | 0 | 0 | 6 | 17 | 17 | 0 |
| Headache | 3 | 3 | 0 | 0 | 6 | 17 | 17 | 0 |
| Vomiting | 5 | 1 | 0 | 0 | 6 | 17 | 17 | 0 |
| Alopecia | 5 | 0 | 0 | 0 | 5 | 14 | 14 | 0 |
| Creatinine | 0 | 5 | 0 | 0 | 5 | 14 | 14 | 0 |
| Pneumonitis | 4 | 1 | 0 | 0 | 5 | 14 | 14 | 0 |
| Constipation | 4 | 0 | 0 | 0 | 4 | 11 | 11 | 0 |
| Dry mouth | 4 | 0 | 0 | 0 | 4 | 11 | 11 | 0 |
| Dyspepsia | 2 | 2 | 0 | 0 | 4 | 11 | 11 | 0 |
Grade 3 and 4 toxicities observed in patients who were initiated at 30 mg (n = 23) or in those initiated at the 25-mg dose (n = 13) are shown in Table 4. There was no difference in the rate of grade 3 and 4 toxicities observed in these 2 groups.
All grade 3 or higher adverse events at least possibly treatment related based on the starting dose of 30 or 25 mg
| Toxicity type, n . | 30 mg (n = 24) . | 25 mg (n = 12) . | ||||
|---|---|---|---|---|---|---|
| Grade 3 . | Grade 4 . | Total (%) . | Grade 3 . | Grade 4 . | Total (%) . | |
| Platelets | 10 | 6 | 16 (67) | 5 | 3 | 8 (67) |
| Hemoglobin | 5 | 2 | 7 (29) | 3 | 0 | 3 (25) |
| Neutrophils | 5 | 2 | 7 (29) | 4 | 2 | 6 (50) |
| Leukocytes | 3 | 1 | 4 (17) | 3 | 1 | 4 (33) |
| Fatigue | 2 | 0 | 2 (8) | 2 | 0 | 2 (17) |
| Syncope | 2 | 0 | 2 (8) | 0 | 0 | 0 |
| Hypophosphatemia | 1 | 0 | 1 (4) | 0 | 0 | 0 |
| Lower GI/hemorrhage NOS | 1 | 0 | 1 (4) | 0 | 0 | 0 |
| Nonneuropathic generalized weakness | 1 | 0 | 1 (4) | 0 | 0 | 0 |
| Bilirubin | 0 | 0 | 0 | 1 | 0 | 1 (8) |
| Total | 32 | 12 | 44 | 18 | 0 | 24 |
| Toxicity type, n . | 30 mg (n = 24) . | 25 mg (n = 12) . | ||||
|---|---|---|---|---|---|---|
| Grade 3 . | Grade 4 . | Total (%) . | Grade 3 . | Grade 4 . | Total (%) . | |
| Platelets | 10 | 6 | 16 (67) | 5 | 3 | 8 (67) |
| Hemoglobin | 5 | 2 | 7 (29) | 3 | 0 | 3 (25) |
| Neutrophils | 5 | 2 | 7 (29) | 4 | 2 | 6 (50) |
| Leukocytes | 3 | 1 | 4 (17) | 3 | 1 | 4 (33) |
| Fatigue | 2 | 0 | 2 (8) | 2 | 0 | 2 (17) |
| Syncope | 2 | 0 | 2 (8) | 0 | 0 | 0 |
| Hypophosphatemia | 1 | 0 | 1 (4) | 0 | 0 | 0 |
| Lower GI/hemorrhage NOS | 1 | 0 | 1 (4) | 0 | 0 | 0 |
| Nonneuropathic generalized weakness | 1 | 0 | 1 (4) | 0 | 0 | 0 |
| Bilirubin | 0 | 0 | 0 | 1 | 0 | 1 (8) |
| Total | 32 | 12 | 44 | 18 | 0 | 24 |
NOS indicates not otherwise specified.
Translational studies
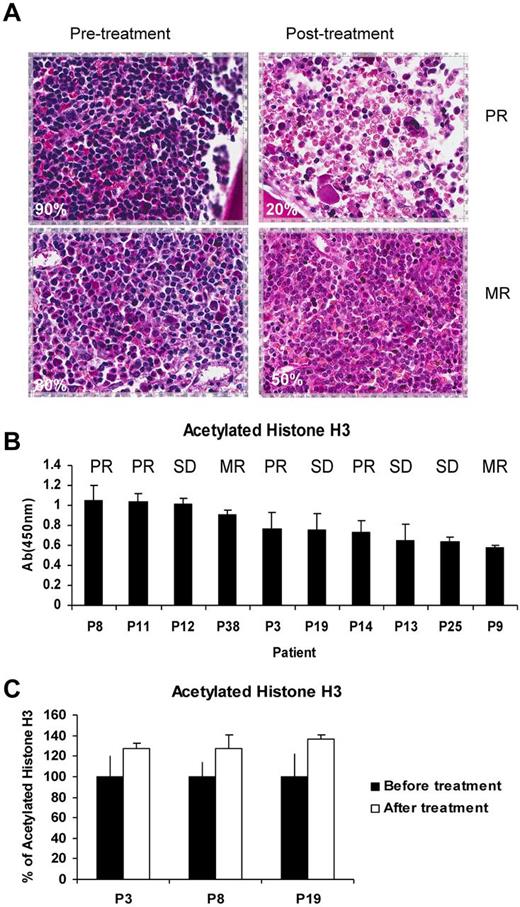
The degree of involvement (ie, the percentage involvement) observed in BM biopsies before and after treatment in patients who achieved MR or better to therapy is shown in Figure 4A. The level of acetylated H3 in the PBMCs is shown in Figure 4B. The numbers were too small to perform correlative studies with response to therapy. Interestingly, we observed an increase in the level of acetylated H3 after therapy in posttreatment samples (Figure 4C).
Correlative studies on samples obtained from patients treated with panobinostat. (A) Immunohistochemistry for CD20 and percentage BM involvement in pre- and posttreatment samples. (B) ELISA for acetylated histone 3 (H3) in PBMCs of samples before therapy in 10 patients with the clinical responses that were obtained in these patients. (C) ELISA for acetylated H3 in PBMCs of samples before and after therapy in 3 patients. Although the levels before and after therapy were not statistically different, there was a trend of increases in the level of acetylated H3 after therapy that is consistent with the activity of HDAC inhibitors.
Correlative studies on samples obtained from patients treated with panobinostat. (A) Immunohistochemistry for CD20 and percentage BM involvement in pre- and posttreatment samples. (B) ELISA for acetylated histone 3 (H3) in PBMCs of samples before therapy in 10 patients with the clinical responses that were obtained in these patients. (C) ELISA for acetylated H3 in PBMCs of samples before and after therapy in 3 patients. Although the levels before and after therapy were not statistically different, there was a trend of increases in the level of acetylated H3 after therapy that is consistent with the activity of HDAC inhibitors.
Discussion
Current recommendations for relapsed or refractory WM include the use of nucleoside analogs, alkylating agents including bendamustine, and novel agents such as bortezomib, everolimus, and immunomodulators.14-17 Despite these advances, most patients relapse or have significant side effects from current therapeutic agents. Therefore, there is a critical need for the development of novel therapeutic agents that have fewer long-term toxicities.
Preclinical studies have shown that epigenetic regulators, including histone acetylation, regulate tumor progression.10,11 Our prior studies have shown significant deregulation in HDAC activity in primary tumor cells, as well as in vitro and in vivo activity of panobinostat in WM.2,4 Based on these data, we initiated this phase 2 trial of single-agent panobinostat as a new class of novel therapeutic agent in WM.
The results of the present study show a response rate of MR or better in 47% of patients with 22% PRs. Response as assessed by paraprotein M spike level included a response rate of MR or better of 55% and PR or better of 30%, including 1 VGPR, 10 PR, 9 MR, and 1 not evaluable. Other studies using novel agents in a similar population of relapsed or refractory WM patients have shown responses of MR or better of 30%-50% using rituximab, 35% using perifosine, 70% using everolimus, and 26%-80% using bortezomib. Therefore, the response rate of 47% of single-agent panobinostat indicates that, indeed, this class of agents is highly active in patients with this low-grade lymphoma.
The response rate of panobinostat in other lymphomas and plasma cell dyscrasias varies.18-21 It is significantly high in Hodgkin lymphoma, with 30%-60% responses, but minimal to absent in multiple myeloma.22 However, significant responses were observed in combinations of panobinostat and bortezomib in multiple myeloma.23,24 Therefore, future studies using panobinostat and bortezomib or other proteasome inhibitors can lead to high responses in patients with WM. The PFS in the present study was 6.6 months. The median PFS for bortezomib was 6.6 months in the Waldenstrom Macroglobulinemia Clinical Trials Group study in a similar patient population.25
This study is relatively small and was performed in only 2 centers, 1 academic and 1 community based. The younger median age of 62 years compared with the median age of 63-65 years in other reported studies and the relatively lower high-risk ISS of 19% compared with 35% in newly diagnosed patients may be because of referral bias of these patients to clinical trials. Larger studies in community practices are needed to confirm the responses observed in this study.
The most common grade 3 and 4 therapy related adverse events included thrombocytopenia, neutropenia, and anemia. Fatigue and diarrhea were also common side effects that have also been seen commonly in other clinical trials using HDAC inhibitors.20,21 Interestingly, we observed pneumonitis in 5 patients in the present study, indicating that this toxicity may also occur with panobinostat. Pneumonitis has also been observed with everolimus and bortezomib in prior studies.26 Dose reductions were required in 72% of patients. In addition, the protocol was modified to allow a starting dose of 25 mg in 12 of 36 (33%) of patients. Despite the dose reduction to 25 mg, most hematologic toxicities remained high, with 67% of patients having grade 3-4 thrombocytopenia. However, responses appeared to be slightly lower in patients who were initiated at the lower dose of 25 mg, although the numbers are too small to make recommendations. Lower initial doses may possibly have lower toxicities, but may also have lower responses. An initial high dose followed by dose reduction may also be beneficial for some patients who require an urgent response in the paraprotein level. Future studies are required to examine different starting dose levels in patients with WM and other low-grade lymphomas, as well as combinations of therapy using lower doses. In addition, newer, more targeted HDAC inhibitors may provide similar responses with fewer off-target toxicities.
In summary, based on the results of the present study, we recommend the use of panobinostat as an effective and safe regimen for therapy in relapsed WM. This clinical trial establishes a role for HDAC inhibitors as a new class of therapeutic agents in the treatment of WM.
Presented in part at the 53rd ASH Annual Meeting and Exposition, December 12, 2011, San Diego, CA.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 USC section 1734.
Acknowledgments
This study was supported in part by a research grant from Novartis (1R01F0003743), the International Waldenstrom Macroglobulinemia Foundation, the Michelle and Steven Kirsch Laboratory for Waldenstrom Macroglobulinemia, and the Heje Fellowship for Waldenstrom.
National Institutes of Health
Authorship
Contribution: I.M.G. designed and performed research, analyzed and interpreted data, and wrote the manuscript; F.C. collected, analyzed, and interpreted data, performed statistical analysis, and wrote the manuscript; T.M. and J.M. performed research and collected and analyzed data; E.B., A.D., F.M., and D.W. collected and analyzed data; R.B., F.A., S.C., and J.K. collected and analyzed data and performed research; S.R. performed research and analyzed data; K.C.A. and P.G.R. designed research and analyzed and interpreted data; and E.W. collected, analyzed, and interpreted data, performed statistical analysis, and wrote the manuscript.
Conflict-of-interest disclosure: I.M.G. received research support for this trial from Novartis and is on the advisory boards of Millennium, Onyx, BMS, and Novartis. K.C.A. is a stockholder of Acetylon and is on the advisory boards of Novartis, Millennium, Onyx, Celgene, and BMS. P.G.R. is on the advisory boards of Millennium, Celgene, and Novartis. The remaining authors declare no competing financial interests.
Correspondence: Irene M. Ghobrial, MD, Medical Oncology, Dana-Farber Cancer Institute, 450 Brookline Ave, Boston, MA, 02215; e-mail: irene_ghobrial@dfci.harvard.edu.


This feature is available to Subscribers Only
Sign In or Create an Account Close Modal