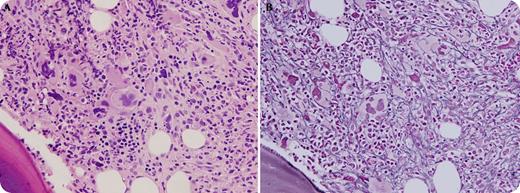
A 55-year-old woman with chronic refractory idiopathic thrombocytopenic purpura (ITP) presented with gum bleeding for 1 day. Over the course of several years, she had failed, or became resistant to, multiple treatments including glucocorticoids, intravenous immunoglobulin, splenectomy, rituximab, and, recently, a 9-month course of weekly romiplostim with moderate compliance. A complete blood count showed mild leukocytosis (white blood cells, 16.2 × 109/L), severe anemia (hemoglobin, 6.7 g/dL), and severe thrombocytopenia (platelet count, 12 × 109/L). Examination of a bone marrow specimen obtained to evaluate her unxplained worsening cytopenias revealed hypercellular marrow with a cellularity of 80%, trilineage hematopoiesis, and increased numbers of pleomorphic megakaryocytes (panel A). A reticulin stain demonstrated diffuse moderate to severe reticulin fibrosis (MF2-MF3; panel B). A diagnosis of romiplostim-induced myelofibrosis was established, and the medication was discontinued. Thrombocytopenia responded to danazol and an increase in the dose of glucocorticoids, and bleeding resolved.
Secondary myelofibrosis occurs in ∼3% of patients treated with thrombopoietin receptor agonists such as romiplostim and is usually reversible and dose dependent. Amplified megakaryocyte-fibroblast interactions and increased levels of cytokines such as transforming growth factor-β in the bone marrow due to chronic thrombopoietin stimulation have been implicated in romiplostim-induced reticulin myelofibrosis.
A 55-year-old woman with chronic refractory idiopathic thrombocytopenic purpura (ITP) presented with gum bleeding for 1 day. Over the course of several years, she had failed, or became resistant to, multiple treatments including glucocorticoids, intravenous immunoglobulin, splenectomy, rituximab, and, recently, a 9-month course of weekly romiplostim with moderate compliance. A complete blood count showed mild leukocytosis (white blood cells, 16.2 × 109/L), severe anemia (hemoglobin, 6.7 g/dL), and severe thrombocytopenia (platelet count, 12 × 109/L). Examination of a bone marrow specimen obtained to evaluate her unxplained worsening cytopenias revealed hypercellular marrow with a cellularity of 80%, trilineage hematopoiesis, and increased numbers of pleomorphic megakaryocytes (panel A). A reticulin stain demonstrated diffuse moderate to severe reticulin fibrosis (MF2-MF3; panel B). A diagnosis of romiplostim-induced myelofibrosis was established, and the medication was discontinued. Thrombocytopenia responded to danazol and an increase in the dose of glucocorticoids, and bleeding resolved.
Secondary myelofibrosis occurs in ∼3% of patients treated with thrombopoietin receptor agonists such as romiplostim and is usually reversible and dose dependent. Amplified megakaryocyte-fibroblast interactions and increased levels of cytokines such as transforming growth factor-β in the bone marrow due to chronic thrombopoietin stimulation have been implicated in romiplostim-induced reticulin myelofibrosis.
For additional images, visit the ASH IMAGE BANK, a reference and teaching tool that is continually updated with new atlas and case study images. For more information visit http://imagebank.hematology.org.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal