Abstract
The plasmin(ogen) and complement systems are activated at sites of tissue injury and are involved in hemostasis, wound healing, inflammation and immune surveillance. Although the mechanisms are poorly understood, dysregulation of these systems underlie the pathogenesis and progression of inflammatory and vascular diseases. We aimed to characterize the relevant molecular interactions between the plasmin(ogen) and complement pathways.
The three complement pathways converge with formation of C3-convertases that cleave C3 into C3a and C3b. C3a is liberated as an anaphylatoxin while C3b participates in further formation of the C3 and C5 convertases, thereby amplifying complement activation. To dampen the system, negative regulatory mechanisms exist. C3b is degraded to iC3b by the factor I (FI)/FH complex, which in turn is degraded to C3dg by the FI/complement receptor 1 (CR1) complex. iC3b and C3dg induce cellular responses by binding to complement receptors CR3 / CR4 / CR2, and CR2, respectively. Interactions of iC3b with CR3 or CR4 induce phagocytosis by macrophages, and binding of iC3b or C3dg to CR2 promotes B-cell responses.
Recent studies show that plasmin proteolyses C3b and iC3b. We further characterized the plasmin cleavage sites in iC3b and evaluated the functional consequences in vitro.
Plasmin cleavage of iC3b was examined over a range of concentrations and times. Plasmin (50 nM) generated a 40 kDa iC3b cleavage fragment (946TLD – PSR1303) which was notable for containing both C3dg (1002HLI – PSR1303) and the C3 thioester domain, necessary for opsonic binding to surfaces.
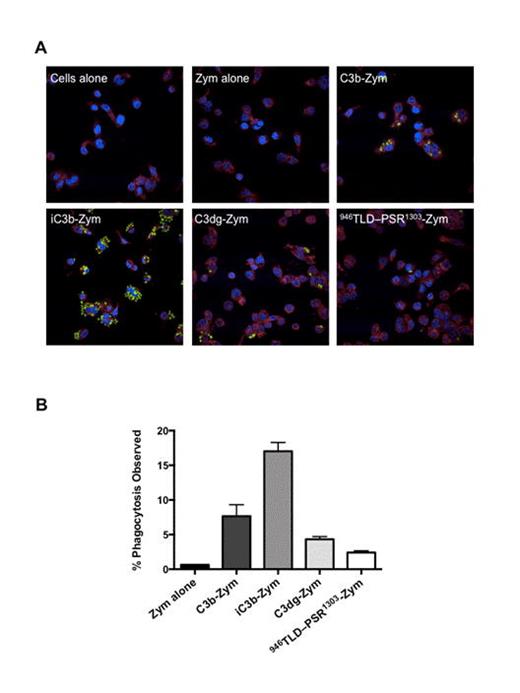
We tested the relevance of this cleavage in phagocytosis assays using immunofluorescence and flow cytometry (Figure 1). C3b bound to the surface of fluorescent (Alexa 488) zymosan particles (C3b-zym), was treated with FI/FH to generate iC3b-zym, and subsequently incubated with FI/CR1 or plasmin to yield C3dg-zym or 946TLD – PSR1303-zym, respectively. Western blots confirmed that plasmin generated 946TLD – PSR1303 from iC3b-zym. The C3 fragment-zymosan species (C3b-zym, iC3b-zym, C3dg-zym and 946TLD – PSR1303-zym) were each incubated with macrophages (PMA-differentiated THP-1 cells) for 90 minutes. Cells were washed, stained and fixed for immunofluorescence, or suspended for flow cytometry. Figure 1, panel A shows macrophages stained with CellMask (red, cell membrane) and DAPI (blue, nucleus). Fluorescent zymosan is seen in green. No phagocytosis was detected with zymosan lacking C3 (zym alone), but there was a small amount with C3b-zym. In contrast, iC3b-zym was highly effective in inducing phagocytosis by most macrophages. This effect of iC3b-zym was abolished with FI/CR1 or plasmin, i.e. little phagocytosis was detected with C3dg-zym or 946TLD – PSR1303-zym.
Flow cytometry-based quantitative analyses confirmed the preceding findings (Figure 1, panel B), with a similar pattern of phagocytosis induced by the zymosan-bound fragments. No phagocytosis was detected with zymosan lacking C3. Phagocytosis of C3b-zym and iC3b-zym was 7±2% and 17±1% of cells, respectively. C3dg-zym and 946TLD – PSR1303-zym induced phagocytosis was <5%.
We also evaluated the role of the complement receptors in mediating the effect of the C3b/iC3b fragments using CR3/4 and CR1 blocking antibodies. These confirmed that phagocytosis of iC3b-zym and C3b-zym is mediated by CR3/4 and CR1, respectively.
Plasmin cleaves iC3b to form a redundant complement regulatory pathway with the FI/CR1 complex, but which notably does not require a cellular cofactor. Further studies will delineate the role of this and other plasmin-generated complement fragments in modulating innate immune and inflammatory responses.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal