Abstract
Core-binding factor (CBF)-positive acute myeloid leukemia (AML) is regarded as a favorable group with good complete remission (CR) rate after induction chemotherapy and is generally treated by repeated high-dose cytarabine consolidation or autologous hematopoietic stem cell transplantation (auto-HSCT). However, emerging molecular studies have recently identified the unfavorable CBF-AML subgroup which should be treated by further intensified treatments.
This single center retrospective study enrolled 264 adult CBF-AML patients from 2002 to 2011. Except 15 patients, 217 patients were treated by intensive induction chemotherapy and 32 were treated by reduced intensity treatment. After CR achievement, patients with available donor were treated by allogeneic (allo)-HSCT and the rest were treated by auto-HSCT or chemotherapy alone. We evaluated 206 patients who achieved CR after intensive chemotherapy regarding survival outcomes according to post-remission therapies and prognostic factors which affected the outcomes. The factors included cytogenetic study and subgroup analysis with additional chromosomes and normal karyotype (NK) mosaicism, c-kit mutation, minimal residual disease (MRD) qPCR level, BAALC and WT1 expression.
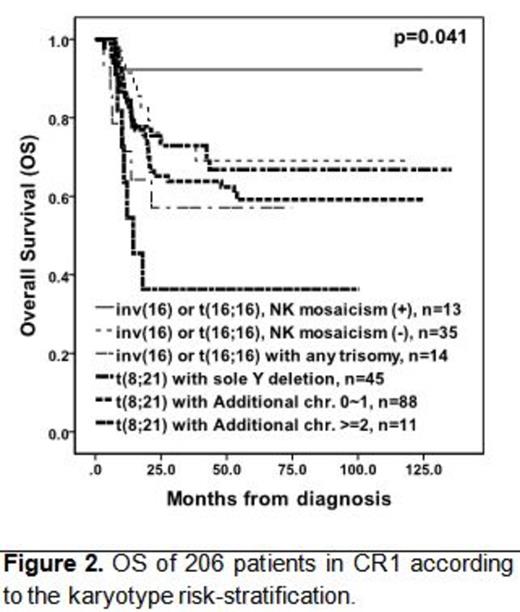
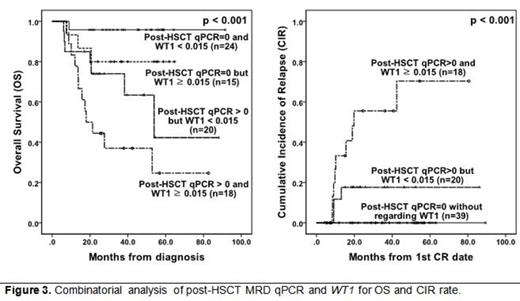
We achieved CR in 94.9% with intensive chemotherapy and 115 patients went on allo-HSCT and 72 were treated by auto-HSCT. There were no significant OS differences between CBF¥â/MYH11 and RUNX1/RUNX1T1 (p=0.173), and auto-HSCT showed favorable EFS (p=0.038) compared to allo-HSCT and chemotherapy alone. For cytogenetic analysis, inv(16) or t(16;16) with NK mosaicism showed the most favorable OS compared to t(8;21) with additional chromosome (¡Ã2) which showed the worst OS. c-kit mutation was a poor prognostic factor with lower reduction rate of post-induction MRD qPCR, however the effect was not definite after HSCT. For HSCT patients, we analyzed post-HSCT MRD qPCR and WT1 expression level. We found that undetected level of post-HSCT MRD qPCR and lower level of WT1 expression (<0.015) showed the most favorable OS with no relapse cases.
For CBF-AML, the role of auto-HSCT and allo-HSCT for selected patients should be re-evaluated by large prospective studies and the values like post-treatment MRD qPCR and WT1 expression level can be used for prediction of patients who might relapse with higher probability.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal