Abstract
Myelodysplastic/myeloproliferative neoplasm, Unclassifiable (MDS/MPN-U) is a distinct entity among the myeloid neoplasms, characterized by the simultaneous presence of both dysplastic and proliferative features. The natural history, clinical characteristics, response to treatment and patient outcome of patients with MDS/MPN-U has not been well described, apart from the MDS/MPN-U provisional entity of Refractory Anemia with Ringed Sideroblasts and Thrombocytosis (RARS-T).
Clinicopathologic features of 85 patients with MDS/MPN-U and without RARS-T were evaluated, along with clinical outcomes based on treatment strategy.
All patients with MDS/MPNs treated from July 1986 to February 2013 at MDACC were reviewed. Patients seen prior to 2006 with a recorded diagnosis of MDS/MPD or chronic MPD-U were reviewed by two hematopathologists and diagnoses were revised as appropriate according to the current WHO criteria. All RARS-T patients per WHO 2008 definition were excluded, and patients were excluded if the de novo presence of both myelodysplastic and proliferative features at diagnostic presentation per WHO criteria was unable to be confirmed.
MDS/MPN-U patients were predominantly over the age of sixty (92%), with a median age of 70 years (range 22 – 90), and 61 patients (72%) were male. 29 patients (35%) had splenomegaly at presentation. Median presenting white blood cell (WBC) count was 17 x 10⁹/L (1 – 141 x 10⁹/L), median hemoglobin was 10 g/dL (5 – 15 g/dL), and median platelet (PLT) count was 85 x 10⁹/L (6 – 1168 x 10⁹/L). Of 56 patients with known JAK2 status, 17 patients (30%) had the presence of the JAK2 V617 mutation. The majority of patients had either diploid cytogenetics (49%) or trisomy 8 as the sole abnormality (15%); 10 patients (12%) had a complex karyotype.
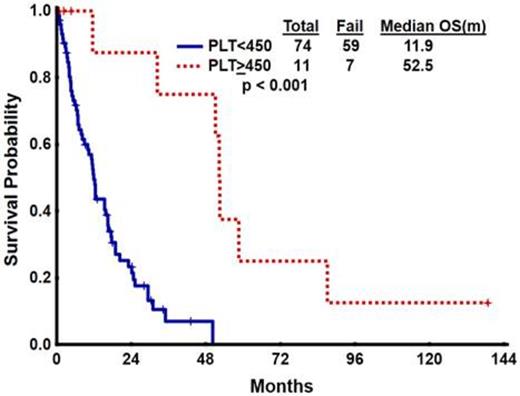
Median OS was 12.4 months (range 0.3 – 138.7). A uniquely favorable outcome was seen in the 11 patients presenting with a PLT count ≥ 450 x 10⁹/L, with median OS 52.5 vs 11.9 months (p<0.001) {Figure 1}. Other variables associated with favorable outcome included age <60 (p < 0.001), lack of circulating blasts (p = 0.023) and <5% bone marrow blasts (p = 0.017). Neither JAK2 V617F mutant status nor karyotype associated with outcome, and in multivariate analysis, only platelet count retained prognostic significance (p=0.001). Whereas the IWG-MF score was not prognostic, the MDS IPSS score imparted a statistically significant classification for the MDS/MPN-U cohort, with a median OS by IPSS score of 15.4, 17.7, 8.3 and 6.9 m, respectively (p = 0.039) {Figure 2}.
Overall, 36 patients (42%) received hypomethylating agent (HMA) therapy. 13 (15%) were treated with an immunomodulatory approach (e.g. lenalidomide, interferon-α), five (6%) underwent splenectomy and five (6%) received stem cell transplant (SCT). HMA-treated patients had an OS of 16.4 vs 11.5 months with other approaches (p=0.57); patients on immunotherapy had a non-significant trend towards worse OS of 11.4 vs 15.4 months (p=0.07). The five patients receiving splenectomy had OS 51.1 m vs 10.0 mo (p=0.12), and with SCT 12.4 vs 12.5 months (p=0.16).
Overall Survival by platelet count at diagnosis
Overall Survival based on MDS IPSS score
Overall, our analysis validates the diagnosis of MDS/MPN-U as a unique pathologic entity, with features and prognostic variables distinctive from either PMF or MDS. While no statistically significant differences in OS were identified based on therapy; in terms of the various diagnostic, prognostic and treatment strategies, MDS/MPN-U patients without RARS-T appear to have characteristics and outcome most analogous to MDS. The favorable outcome of surgical splenectomy among those MDS/MPN-U patients with splenomegaly suggests this may also be part of a a reasonable therapeutic approach.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.


This feature is available to Subscribers Only
Sign In or Create an Account Close Modal