Abstract
More active high-dose (HD) regimens are needed for refractory myeloma, where single-agent melphalan offers poor outcomes. Registry data suggest that busulfan/melphalan might be superior to melphalan in 1st-line treatment of chemosensitive patients. While gemcitabine has potent activity in vitro against resistant myeloma cell lines, this drug has shown little activity in patients with resistant myeloma when tested in short 30-min infusions. Gemcitabine cytotoxicity correlates with the intracellular accumulation of its active triphosphate metabolite, which is optimized when infused at a fixed dose rate (FDR) of 10 mg/m2/min. We previously developed a HD regimen of Gem/Bu/Mel, infusing gemcitabine at FDR and exploiting its inhibition of DNA damage repair, with a manageable toxicity profile. In its phase 1 trial (Nieto, BBMT 2012) Gem/Bu/Mel showed some encouraging signs of activity in patients with refractory myeloma. Thus, we wished to study Gem/Bu/Mel in refractory myeloma patients who either had an estimated CR likelihood <15% with high-dose melphalan or had disease that previously failed HD Mel, whose median PFS after a 2nd ASCT is typically ≤1 year (Qazilbash, Cancer 2006; Michaelis, BBMT 2013).
Patients ages 18-70, with myeloma treated in 1st-line therapy with lenalidomide, bortezomib or thalidomide, plus ≥1 of the following 3 criteria: no response to 1st-line therapy, relapse after 1st-line therapy, or relapse after prior ASCT, along with adequate end-organ function, were eligible for this phase 2 study. Gemcitabine was given on days -8 and -3 as a loading dose of 75 mg/m2 followed by FDR infusion of 1,800 mg/m2. Busulfan was given on days -8 to -5 targeting AUC 4,000/day x 4. Melphalan was given at 60 mg/m2/day x 2 (days -3 and -2). The primary study endpoint was CR rate (determined by day 100 before starting maintenance treatment); secondary endpoints were CR+VGPR, RR, PFS and OS. This trial was sized with >85% power to detect a CR rate ≥20%, which was considered clinically significant.
Between 11/10 and 6/13, 60 patients were enrolled, all of whom had failed at least 1 line of therapy (Table).
| Age | 57 (39-65) | |
| ISS stage at diagnosis | 1 | 24 (40%) |
| 2 | 18 (30%) | |
| 3 | 18 (30%) | |
| Median # prior lines of treatment (range) | 3 (2-10) | |
| Primary refractory (IMWG criteria: never achieved a minimal response or better with any therapy) | 9 (15%) | |
| Relapsed and refractory (IMWG criteria: nonresponsive while on salvage therapy or progressive within 60 days of last therapy) | 24 (40%) | |
| High-risk cytogenetics | Overall | 20 (33%) |
| 17p- | 9 (15%) | |
| t(4;14) or t(14;16) | 4 (7%) | |
| 1q+ | 6 (10%) | |
| Cytogenetic 13q- | 6 (10%) | |
| Extramedullary disease | 5 (8%) | |
| Renal failure at diagnosis | 15 (25%) | |
| Hypercalcemia at diagnosis | 10 (17%) | |
| Prior ASCT | 25 (42%) | |
| Status at HDC (CR / PR / no response) | 9 / 30 / 21 | |
| PD at HDC | 14 (23%) | |
| Age | 57 (39-65) | |
| ISS stage at diagnosis | 1 | 24 (40%) |
| 2 | 18 (30%) | |
| 3 | 18 (30%) | |
| Median # prior lines of treatment (range) | 3 (2-10) | |
| Primary refractory (IMWG criteria: never achieved a minimal response or better with any therapy) | 9 (15%) | |
| Relapsed and refractory (IMWG criteria: nonresponsive while on salvage therapy or progressive within 60 days of last therapy) | 24 (40%) | |
| High-risk cytogenetics | Overall | 20 (33%) |
| 17p- | 9 (15%) | |
| t(4;14) or t(14;16) | 4 (7%) | |
| 1q+ | 6 (10%) | |
| Cytogenetic 13q- | 6 (10%) | |
| Extramedullary disease | 5 (8%) | |
| Renal failure at diagnosis | 15 (25%) | |
| Hypercalcemia at diagnosis | 10 (17%) | |
| Prior ASCT | 25 (42%) | |
| Status at HDC (CR / PR / no response) | 9 / 30 / 21 | |
| PD at HDC | 14 (23%) | |
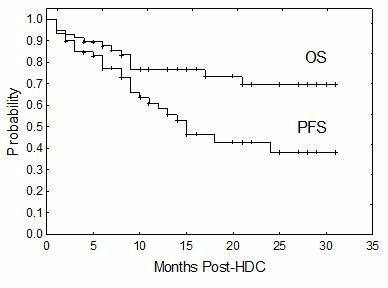
Neutrophils and platelets engrafted on d+10 (8-13) and d+11 (9-16), respectively. There were 3 treatment-related deaths (4.9% TRM: 1 pneumonia, 1 cardiac arrest with unrevealing autopsy, 1 E coli sepsis). Toxicities: mucositis (50% G2, 18% G3), rash (20% G2, 6% G3), asymptomatic transaminase elevation (17% G2, 8% G3) and bilirubin elevation (3% G2, 10% G3) (no cases of VOD), with no renal, cardiac, neurological or pulmonary toxicity. Among 49 patients with measurable disease at transplant and evaluable for response, the CR rate was 24.5% (95% CI, 16-32.5%), 42% CR/VGPR rate (36-50%), and 77.5% RR (71-83%). Posttransplant maintenance was given to 38 patients, using lenalidomide (N=23), bortezomib (N=11), thalidomide (N=3) and bendamustine (N=1). At median f/u of 16 months (range, 2-31), the PFS and OS rates are 55% (median 15 months) and 77% (median not reached), respectively (Figure). In the subset of 25 patients receiving Gem/Bu/Mel as a 2nd salvage ASCT, there were 1 CR, 2 VGPR and 7 PR for a CR+VGPR of 19%, RR 62.5%, with 52% PFS (median 15 months) and 68% OS (median NR). In the subset of 20 patients with high-risk cytogenetics (N=20), there were 28% CR, 56% CR+VGPR and 83% RR, with 55% PFS (median 14 months) and 80% OS (median NR).
Gem/Bu/Mel is a safe and highly active HD regimen in refractory myeloma and warrants its further study in earlier stages of this disease.
Nieto:Otsuka Pharmaceuticals: Research Funding. Off Label Use: Gemcitabine not approved for myeloma. Qazilbash:Otsuka Pharmaceuticals: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal