High dose chemotherapy followed by an autologous stem cell transplant (auto-HCT) is considered standard of care in patients with newly diagnosed multiple myeloma (MM). In a recent randomized trial, median progression free survival (PFS) after auto-HCT, with or without maintenance therapy was 46 and 27 months, respectively (McCarthy P et al. NEJM 2012). However, about 15% of patients are reported to have much longer PFS (Pineda-Roman M et al. Cancer 2008). Here we tried to identify the factors that may predict a long PFS after auto-HCT.
We performed a retrospective chart review of patients who received an auto-HCT for MM between January 2000 and March 2007. A total of 1135 patients underwent an auto-HCT during this period, and 194 patients (17%) had a minimum PFS of 72 months or longer after a single auto-HCT. The primary objective was to determine the variables associated with a long PFS and overall survival (OS).
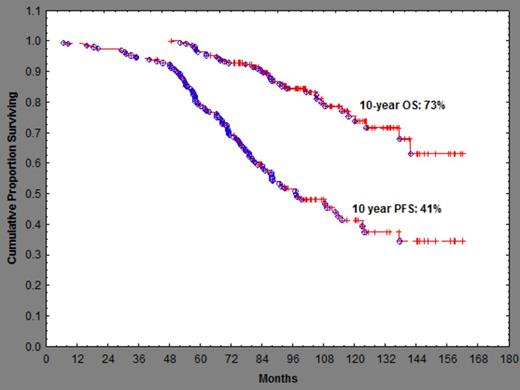
Patient characteristics and outcomes are shown in the attached Table. The median age at auto-HCT was 56 years, and the median time from diagnosis to auto-HCT was 7.5 months. Twenty-three (13%) patients had ≥ 10% plasma cells in the bone marrow at auto-HCT and only 9 patients (4.8%) had high-risk cytogenetic abnormalities. One-hundred and fifty (77%) patients received induction therapy containing either an immunomodulatory (IMiD) agent or a proteasome inhibitor (PI). At the time of the auto-HSCT, only 13 (6.7%) patients were in CR and 38 (19.6%) were CR or VGPR after induction therapy (Table). One-hundred and sixty three (84%) patients received mephalan alone as conditioning regimen. Eighty-one (42%) patients received post auto-HCT maintenance. Eighty (41%) patients achieved a CR, while 104 (54%) achieved CR + VGPR after auto-HCT. Six patients (3.1%) developed a second primary malignancy post- autologous transplant. After a median follow-up of 95.4 months, median PFS was 97.3 months and median OS has not been reached. The 10-year PFS and OS were 41% and 73% respectively. Use of melphalan alone as preparative regimen was associated with a longer PFS and OS (p=0.004 and 0.004, respectively). Achievement of CR after auto-HCT was associated with a longer PFS only (p=0.001), and the use of IMiD or a PI as induction was associated with a longer OS (p=0.01).
Table. Patient Characteristics and Outcome
| Male | 122 (63%) |
| Median Age | 56 (29-77) |
| Age >65 at auto-HCT | 22 (11.3%) |
| Induction with novel agents | 152 (78%) |
| Maintenance Rx | 81 (42%) |
| PC >10% at auto-HCT | 23 (13.5%) |
| LDH > 618 | 70 (37.6%) |
| b2m >3.5 | 34 (18.3%) |
| High-risk cytogenetic abnormalities | 9 (4.8%) |
| Disease status at auto-HCT · CR · VGPR · PR · <PR | 13 (6.7%) 25 (12.9%) 132 (68.0%) 24 (12.3%) |
| Median Interval DX to auto-HCT (months) | 7.5 (2.8-140) |
| IMiD or PI for induction | 150 (77%) |
| Melphalan alone as preparative regimen | 163 (84%) |
| Median CD34 dose x 10e6 | 4.5 (2.1-11.6) |
| Median time to ANC 500 | 10 days |
| Median time to PLT 20 | 10 days |
| Response after auto-HCT CR + CR sCR + CR + VGPR | 18 + 62 = 80 (41%) 18 + 62+ 24= 104 (53.6%) |
| Median F/U (months) | 95.4 (48.7 – 162.1) |
| Median PFS | 97.3 months |
| 10-year PFS | 41% |
| Median OS | NR |
| 10-year OS | 73% |
| Male | 122 (63%) |
| Median Age | 56 (29-77) |
| Age >65 at auto-HCT | 22 (11.3%) |
| Induction with novel agents | 152 (78%) |
| Maintenance Rx | 81 (42%) |
| PC >10% at auto-HCT | 23 (13.5%) |
| LDH > 618 | 70 (37.6%) |
| b2m >3.5 | 34 (18.3%) |
| High-risk cytogenetic abnormalities | 9 (4.8%) |
| Disease status at auto-HCT · CR · VGPR · PR · <PR | 13 (6.7%) 25 (12.9%) 132 (68.0%) 24 (12.3%) |
| Median Interval DX to auto-HCT (months) | 7.5 (2.8-140) |
| IMiD or PI for induction | 150 (77%) |
| Melphalan alone as preparative regimen | 163 (84%) |
| Median CD34 dose x 10e6 | 4.5 (2.1-11.6) |
| Median time to ANC 500 | 10 days |
| Median time to PLT 20 | 10 days |
| Response after auto-HCT CR + CR sCR + CR + VGPR | 18 + 62 = 80 (41%) 18 + 62+ 24= 104 (53.6%) |
| Median F/U (months) | 95.4 (48.7 – 162.1) |
| Median PFS | 97.3 months |
| 10-year PFS | 41% |
| Median OS | NR |
| 10-year OS | 73% |
PC – plasma cell, LDH- lactate dehydrogenase, b2m- beta-2- microglobulin, CR- complete remission, sCR- stringent CR, VGPR- very good partial remission, PR – partial remission, PFS – progression free survival, OS – overall survival, F/U- follow-up, ANC- absolute neutrophil count, PLT- platelet, IMiD- immunomodulatory, PI- proteasome inhibitor, NR- not reached
Approximately 17% patients achieved a median PFS of 6 years or longer after a single auto-HCT. The long PFS in this cohort may be associated with younger age, low incidence of HR cytogenetics, use of an IMiD or PI as induction therapy, relatively low disease burden at auto-HCT, transplant from the year 2000 onwards, achievement of CR in >40% and the use of melphalan alone as preparative regimen.
Shah:Celgene: Membership on an entity’s Board of Directors or advisory committees, Research Funding. Qazilbash:Celgene: Membership on an entity’s Board of Directors or advisory committees.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal