Abstract
CLL patients (pts) with del(17p13.1) (17p-) karyotype are typically refractory to therapy. There are limited data on clinical outcomes of large groups of these pts treated at a single institution. We aimed to develop a risk score to classify pts with de novo 17p- CLL at high risk of early treatment or death.
We retrospectively reviewed records of 114 CLL pts with 17p- and no prior therapy seen at OSU from 2002-2012. Treatment free survival (TFS) was calculated from date of 1st visit until date of 1st treatment or death, censoring pts alive and treatment-free at last follow-up. Overall survival (OS) was calculated from date of 1st visit until date of death or last follow-up. TFS/OS estimates were calculated using the Kaplan-Meier method. Proportional hazards models were fit using backwards selection to identify variables significantly associated with TFS & OS. A risk score (RS) was calculated based on the variables and regression coefficients of the model. A simplified risk score (SRS) to be used in clinical practice was based on the strength of associations with clinical outcome when all variables had been categorized. To externally validate the SRS, a dataset of 129 de novo 17p- pts was obtained from MD Anderson Cancer Center (MDA). Consistency in model coefficients used to derive the SRS and predictive power of the SRS using Harrell’s c-index (c) were compared between the sets.
In the OSU set, median age was 62 yrs, 33% had Rai Stage 0, 61% had ECOG performance status (PS) 0 and 11% had ECOG PS >2. Around 35% and 10% of pts had white blood cell count (WBC) >50 x109/L and lactate dehydrogenase at least 2 x the upper limit of normal (LDH x2 ULN), respectively. Only 14% had concomitant 11q- and 36% had complex karyotype with >3 aberrations. None of these variables were significantly different between the OSU and MDA sets (p>0.15), nor were TFS and OS (p>0.10). Median TFS estimates were 16 mos (95%CI 6-27) and 6 mos (95%CI 3-12) for the OSU and MDA sets, respectively, while median OS estimates were 5.2 yrs (95%CI 3.4-7.8) and 6.4 yrs (95%CI 4.7-not reached).
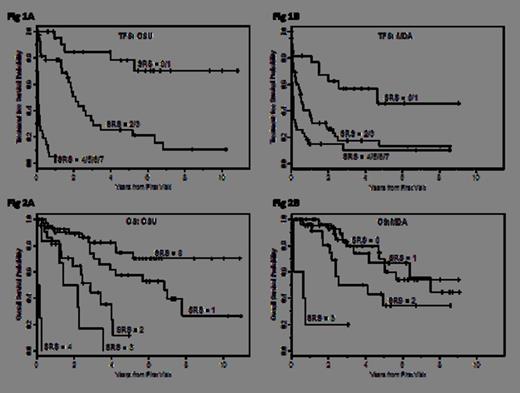
Using the OSU set, a multivariable model for TFS included ECOG PS, Rai Stage, WBC and 11q- (all p<0.017, c=0.84). A RS used the formula: 0.794 x (ECOG PS1, no=0,1=yes) + 1.686 x (ECOG PS≥2, no=0,1=yes) + 1.485 x (Rai I/II/III/IV, no=0,1=yes) + 0.053 x (age in yrs) + 0.0045 x (WBC) + 0.881 x (11q-, no=0,1=yes). A SRS used the formula: 1 x (ECOG PS1, no=0,1=yes) + 2 x (ECOG PS≥2, no=0,1=yes) + 2 x (Rai Stage I/II/III/IV, no=0,1=yes) + 1 x (age≥65yrs) + 1 x (WBC>50) + 1 x (11q-, no=0,1=yes), with possible scores ranging from 0 to 7. TFS estimates at 2 yrs for SRS=0/1, 2/3, and >4 were 85% (95%CI=0.60-0.95), 51% (95%CI=0.32-0.67), and 0%, respectively (Figure 1A). In the MDA set, Rai Stage and WBC contributed significantly to the SRS, followed by ECOG PS, with little consistency in the impact of age or 11q- compared with the OSU set, leading to a loss in predictive power (c=0.66). Still, the SRS was significantly associated with TFS (p<0.0001), with 2-yr estimates of 63% (95%CI=0.39-0.79), 26% (95%CI=0.15-0.39), and 16% (0.06-0.29) for SRS=0/1,2/3, and >4 (Figure 1B).
Using the OSU set, a multivariable model for OS included ECOG PS, age, and LDH (all p<0.025, c=0.76). A RS used the formula: 0.783 x (ECOG PS1, no=0,1=yes) + 1.637 x (ECOG PS≥2, no=0,1=yes) + 0.042 x (age in yrs) + 0.445 x (LDH relative to ULN). A SRS used the formula: 1 x (ECOG PS1, no=0,1=yes) + 2 x (ECOG PS≥2, no=0,1=yes) + 1 x (age≥65yrs) + 1 (LDH x2ULN, no=0,1=yes), with possible scores ranging from 0 to 4. The SRS was associated with OS (p<0.0001, c=0.73), with 2-yr estimates of 89% (95%CI=0.74-0.96), 64% (95%CI=0.39-0.81) and 0% for those with SRS=0, 2, and 4, respectively (Figure 2A). In the MDA set, with the exception of ECOG PS 1, the strength in association of all variables with OS was similar to what had been observed in the OSU set. The predictive ability of the SRS decreased in the MDA set (c=0.68), but remained associated with OS, with the highest score showing early, inferior OS (Figure 2B). Estimates at 2 yrs ranged from 95% (95%CI=0.83-0.99), to 80% (95%CI=0.55-0.92) to 20% (95%CI=0.01-0.58) with an SRS of 0, 2, and 3, respectively; no one had a SRS=4.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal