One of the complications of myeloablative conditioning regimen with busulfan (BU) and cyclophosphamide (CY) in children undergoing hematopoietic stem cell transplantation (HSCT) is the occurrence of hemorrhagic cystitis (HC). Pathophysiology of HC involves multiple factors, such as damage to the bladder's transitional epithelium and the endothelium of blood vessels by BU, CY and their metabolites, viruses, bacterial infections, or other disease processes. It is well established fact that damage to the urothelium is the initial step during pathogenesis of HC. Though it is known about acrolein (metabolite of CY) contribution to HC development, the role of BU or its metabolites is not yet known completely. We recently developed an analytical method for sulfolane (Su) quantification, a water soluble metabolite of BU. Using this method we explored the relation of Su levels in plasma with HC before day 30 post-transplant, in 39 children (20 females, 19 males) receiving BU-CY conditioning prior to HSCT.
Hospital ethics committee approved the study, and all patients or their parents have signed the informed consent. Out of 39 patients 16 were diagnosed with nonmalignant disease. BU was administered in 16 dose infusions, with each infusion lasting two hours for every six hours. Bone marrow and cord blood were graft sources in 18 and 21 patients, respectively. Twenty patients had HLA–matched donor. HC was defined as the presence of hematuria (both microscopic and macroscopic) for more than a week from the initiation of the conditioning regimen up to 30 days post-transplant. All patients received MESNA as prophylaxis for HC. Plasma from patients collected before dose 7 and after dose 9 infusions of BU was used for measuring Su levels using gas-chromatography. Plasma levels of Su adjusted to cumulative BU dose up to Su level measurements (upto dose 6 for before dose 7 levels, upto dose 9 for after dose 9 levels) in mg/kg were used in the analysis. Mann-Whitney U test was used to analyze the relation of Su levels (ng/mL//mg/kg) and HC. A receiver–operator characteristic curve (ROC) for Su levels was plotted to show the trade-off in sensitivity versus 1- specificity rates for HC, as the cut-off of the test was shifted from low to high. Two sided p values were represented and probability at 0.05 was considered as statistically significant. Cumulative incidences of HC were estimated using Kaplan-Meier curves and log-rank test was used to compare the difference between groups divided based on cutoff defined in ROC curves, in univariate analysis. Univariate cox-regression was used to estimate hazard ratios with 95% confidence intervals.
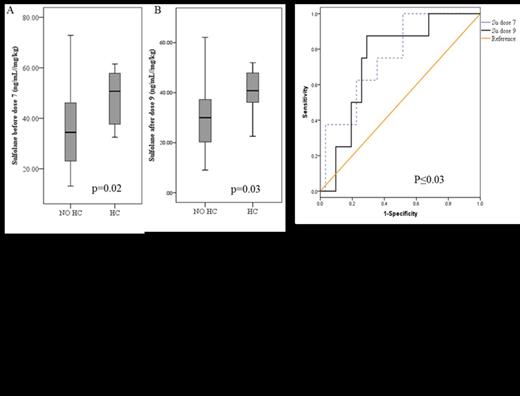
The overall cumulative incidence of HC was 20.5 %. We observed higher Su levels before dose 7 (mean±SD; 48.3±11.2 vs. 35.1±15.3 – p=0.02) and after dose 9 (40.5±9.6 vs. 30.9±14.4 – p=0.03) in patients diagnosed with early HC (n=8) compared to those with no HC (n=31-Figure 1A, Figure 1B), respectively. Cutoff values of 49.44 and 36.28 were chosen in ROC analysis for Su levels before dose 7 and after dose 9, respectively with better sensitivity and specificity to diagnose HC (Figure 1C). Patients with Su levels above the cutoff value defined (before dose 7, 41.7 %; after dose 9 42.9 %) had higher incidence of HC compared to those below the cutoff (before dose 7, 11.0 %; after dose 9, 8.0 %) at both dose levels (Figure 2A, Figure 2B). Age and Weight were also correlated with the incidence of HC, with higher incidence in patients older than 10 years, and weighed above 30 kg. Higher levels of Su correlated with the weight and age of the patients. Out of 8 individuals diagnosed with HC, 6 were detected positive for BK virus and one patient was positive for JC virus.
Higher plasma Su levels might also explain availability of Su and its hydroxyl metabolite in bladder to cause damaging effect similar to that of acrolein. We hypothesize that formation of Su is related to the volume of liver and enzyme activity which is usually correlated with weight and age of the patient. These levels might also predict the extent for acrolein formation, and might serve as surrogate marker to identify patients predisposed to HC. A functional study to elucidate the effect of Su on bladder urothelium is underway at our laboratory to understand its role in pathogenesis of HC.
No relevant conflicts of interest to declare.


This feature is available to Subscribers Only
Sign In or Create an Account Close Modal