Abstract
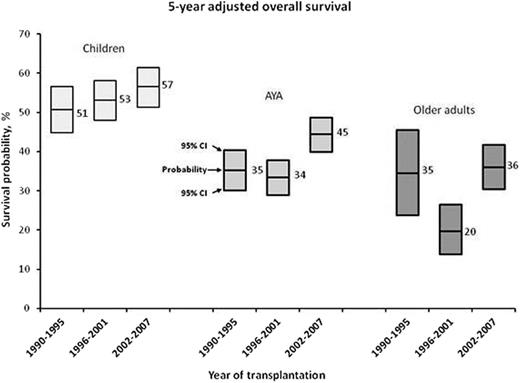
Adolescents and young adults (AYAs) with cancer have not experienced survival improvements over time to the same extent as younger and older patients. Studies in acute lymphoblastic leukemia (ALL) have identified differences in chemotherapy treatment approaches, adherence and possibly outcomes for AYAs treated in pediatric vs. adult settings. To determine if these same issues are operative in ALL patients treated with hematopoietic cell transplantation (HCT), we compared outcomes among 2730 patients including 1008 children (<15 years), 1244 AYAs (15-40 years) and 478 older adults (> 40 years) receiving myeloablative allogeneic HCT for ALL at US centers over three time periods (1990-1995, 1996-2001, and 2002-2007). All patients were in first or second complete remission at HCT; Ph+ patients were included; umbilical cord blood transplant recipients were excluded. The proportions of patients receiving peripheral blood transplants and receiving HCT using well-matched unrelated donors increased over time in all three age groups. From 1996-2001 to 2002-2007, transplant volume increased by 7% in children, 50% in AYAs, and 180% in older adults. Our analysis demonstrated that 5-year overall survival varied inversely with age group, but survival for AYAs over time improved at rates comparable to survival in children (Figure). Multivariate analyses adjusting for important patient and disease characteristics confirmed that older age was associated with poorer survival (hazard ratio 2.2 for older adults and 1.7 for AYA vs. children, P<0.001); however, no significant interactions were observed between age and time period confirming that changes in survival rates over time were similar between the groups even after statistical adjustment for other factors. Similar findings were observed for transplant-related mortality (TRM) and relapse. Transplantation techniques and outcomes were also explored for a subset of 131 AYAs (ages 15-25) transplanted at 46 pediatric or 92 adult centers. Although limited by small numbers, univariate analyses did not show differences in probabilities of overall survival, TRM, or relapse by center type. Patients transplanted at pediatric centers had a longer time from diagnosis to transplant than patients transplanted at adult centers (p=0.024), and were more likely to receive bone marrow vs. peripheral blood stem cell graft (p<0.001). Conditioning regimens (p=0.04) and GVHD prophylaxis (p<0.01) also differed. Taken together, these findings suggest that, in contrast to what has been observed for other cancers over time, survival following myeloablative allogeneic HCT for AYA’s has improved at a rate comparable to other age groups. There appear to be differences in transplant timing and techniques for AYAs depending on whether treatment occurs in a pediatric or adult center but transplant outcomes did not significantly differ, in contrast to survival differences reported in the non-transplant setting. In summary, AYAs are experiencing improvements comparable with younger children, and appear to have similar outcomes whether transplanted at pediatric or adult centers. Close modal
Figure
5-year adjusted overall survival probabilities for the three age-groups and time periods. Boxes represent estimates (center lines) and 95% confidence intervals.
Figure
5-year adjusted overall survival probabilities for the three age-groups and time periods. Boxes represent estimates (center lines) and 95% confidence intervals.
Disclosures:
No relevant conflicts of interest to declare.
Author notes
*
Asterisk with author names denotes non-ASH members.
© 2013 by The American Society of Hematology
2013

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal