Abstract

Elderly multiple myeloma (MM) patients are an heterogeneous population. Aging is associated with an increased frequency of co-morbidities, frailty and disability, with negative impact on treatment tolerance and outcome. A simple and reliable scoring system, based on geriatric assessment, has been developed to predict survival and used also to predict the risk of severe toxicities or treatment discontinuation in elderly newly diagnosed MM patients treated with lenalidomide-, bortezomib- or carfilzomib-based induction regimens.
Patients with newly diagnosed MM, ineligible for high-dose therapy and autologous stem cell transplantation due to age (≥65 years) or coexisting co-morbidities, enrolled in 3 prospective multicenter trials, were included in the analysis. Up-front dose reductions were performed according to patients age (full doses for patients ≤75 years and reduced for patients >75 years). Details on treatment regimens and results of these studies have previously been reported (Gay F et al EHA 2013, Larocca A et al EHA 2013, Bringhen S et al EHA 2013). At diagnosis, a geriatric assessment had been performed, to assess co-morbidities, cognitive and physical conditions.
869 patients were included in the analysis: 659 enrolled in the lenalidomide-based, 152 in the bortezomib-based and 58 in the carfilzomib-based trial. Median age was 74 years, and 44% of patients were older than 75 years. Median follow-up was 18 months.
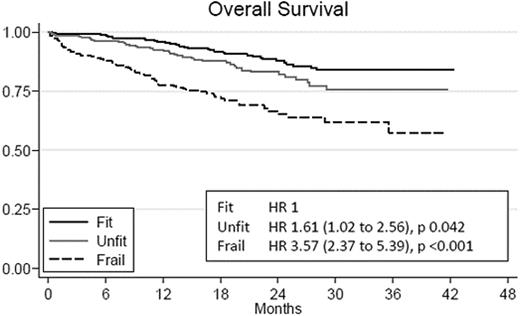
In univariable analysis, the risk of death was higher in patients aged 75-80 (Hazard Ratio, HR 1.37, p=0.11), and in patients older than 80 years (HR 2.75, p<0.001), compared to patients younger than 75 years. Performance status and gender did not significantly impact overall survival (OS). In a multivariable Cox model, an additive scoring system (range 0-5), based on age, co-morbidities, cognitive and physical conditions, was categorized to identify 3 groups: fit (score=0, 39%); unfit (score=1, 31%), and frail (score≥2, 30%). The 18-month OS was 92%, 88% and 73% in the three categories (fit, unfit and frail), respectively.
In a Cox's model, including ISS, gender and performance status, the HR compared to the fit category was 1.4 (p=0.18) and 2.9 (p<0.001) in unfit and frail patients. The cumulative 6-month risk of serious adverse events or treatment discontinuation was 44%, 47% and 55% in fit, unfit and frail patients, respectively. The higher mortality rate in unfit and frail patients seems mainly due to higher cumulative incidence of grade ≥3 adverse events (in particular extra hematologic toxicities) causing subsequent treatment discontinuation.
The use of a simple scoring system, based on geriatric assessment, allows the identification of groups of patients with different survival and risk of severe toxicities.
Overall survival and crude Hazard Ratio for fit, unfit and frail patients.
Larocca:Celgene: Honoraria; Janssen-Cilag: Honoraria. Bringhen:Celgene: Honoraria; Janssen-Cilag: Honoraria; Novartis: Honoraria; Merck Sharpe & Dohme: Membership on an entity’s Board of Directors or advisory committees; Onyx: Consultancy. Gay:Celgene: Honoraria; Janssen-Cilag: Honoraria; Celgene: Membership on an entity’s Board of Directors or advisory committees; Byotest: Membership on an entity’s Board of Directors or advisory committees. Boccadoro:Celgene: Research Funding; Janssen-Cilag: Research Funding; Celgene: Consultancy; Janssen-Cilag: Consultancy; Celgene: Membership on an entity’s Board of Directors or advisory committees; Janssen-Cilag: Membership on an entity’s Board of Directors or advisory committees. Palumbo:Amgen: Consultancy, Honoraria; Bristol-Myers Squibb: Consultancy, Honoraria; Celgene: Consultancy, Honoraria; Janssen Pharmaceuticals: Consultancy, Honoraria; Millenium: Consultancy, Honoraria; Onyx: Consultancy, Honoraria.
Author notes
Asterisk with author names denotes non-ASH members.

This icon denotes a clinically relevant abstract

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal