Abstract
Germline mutations in the N-terminal of CCAAT/enhancer binding protein α (CEBPA) are a feature of autosomal dominant AML. Despite the strong penetrance of these mutations, the age of disease onset varies considerably and is usually precipitated by acquiring a C-terminal mutation. Although biallelic CEBPA-mutations in sporadic AML are associated with favorable clinical outcomes, little is known about long-term survival or the secondary molecular events linked with familial cases.
We sought to establish the long term clinical outcomes in familial CEBPA-mutated AML and to examine the patterns of secondary mutations associated with leukemic transformation.
Disease specific and follow up information was collected in 16 affected patients, from 7 pedigrees, published between 2004 and 2011. In 94% of patients (n=15), at least 3 years follow up was achieved. All pedigrees had a germline N-terminal CEBPA mutation and 17 of 18 documented disease episodes had an acquired C-terminal mutation.
The age at AML diagnosis varied from 2-39 years (median 24.5 yrs) with a single asymptomatic carrier detected (now 23 yrs). With the exception of 1 patient diagnosed in 1963, all cases received combination chemotherapy at diagnosis. Additional consolidation comprised autologous stem cell transplantation (SCT, n=3) and allogeneic SCT in 1 patient failing to achieve CR post induction therapy. Ten patients had at least 1 further disease episode, the first recurrence presenting after a median of 2.1 years (range 0.5-14 yrs), 5 continued in CR and 1 patient was lost to follow up. In 3 out of 4 patients, where CEBPA was screened at recurrence, the acquired C-terminal mutations differed from diagnosis, signifying new episodes of AML. The median overall survival (OS) for the entire cohort was 20 years (1.1-46 yrs, n=16) and 17.3 years for patients with multiple disease episodes, reflecting durable responses to second line therapies.
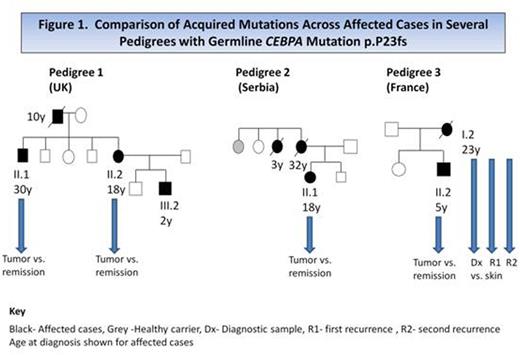
To identify potential co-operating mutations in CEBPA pedigrees, whole exome sequencing (WES) was performed in 7 tumor samples from 5 patients across 3 pedigrees, all with the germline mutation p.P23fs (Figure 1). All tumor DNA samples were sequenced with matched remission or skin DNA as a germline control. The number of acquired mutations in familial tumors was similar to sporadic disease, with 10-22 (median=14) non-synonymous tier 1 mutations per sample. In addition to the acquired C-terminal CEBPA mutation, these included established AML loci such as EZH2, TET2, WT1, GATA2, NRAS, CSF3R and the recently identified cohesin complex gene, SMC3. Of note, FLT3-ITD, NPM1 and DNMT3A mutations were absent in all tumors. A minimum of 2 established mutations were identified in each tumor and, at present, we can only speculate on which additional mutations are ‘driver' or ‘passenger' events.
Reflecting findings in sporadic AML, biallelic CEBPA and GATA2 mutations co-occurred in both siblings from Pedigree 1 and were subsequently identified by Sanger sequencing in the child III.2 (Figure 1). All 3 patients continue in long term remission following chemotherapy. We were able to trace the clonal evolution in patient I.2 (Pedigree 3) by WES of 3 consecutive tumor samples which arose over a 17 year period. At diagnosis (Dx) the patient received induction and consolidation chemotherapy and remained disease free for 14 years. The second disease episode (R1) was treated with chemotherapy followed by autologous SCT and the third presentation (R2) was chemo-refractory. Tumor DNA from R2 was clonally related to Dx, sharing 7 identical mutations, including the original C-terminal CEBPA deletion. In contrast, R1 appeared molecularly distinct from Dx and R2, most likely representing a new clone which was subsequently eradicated with treatment.
This is the first report of long term clinical outcomes in familial CEBPA-mutated AML. Although many patients experienced disease recurrence, our extended follow up showed that OS remained favorable despite multiple episodes of disease. Assessment of C-terminal CEBPA mutations provided a unique insight into the recurrence of AML, with some patients appearing to develop completely new leukemic episodes. Although the penetrance of germline mutations is high, healthy carriers and late onset disease are noted, emphasizing the need for clinical vigilance and screening of all related potential SCT donors.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal