Key Points
In contrast to their suppressive effects on T cells, src-kinase inhibitors strongly enhance IL-12 production in human myeloid cells.
This effect is synergistic to TLR2 or TLR4 signaling, whereas inhibition of src-kinases alone does not trigger DC activation.
Abstract
Src-kinase inhibitors hold great potential as targeted therapy against malignant cells. However, such inhibitors may also affect nonmalignant cells and cause pronounced off-target effects. We investigated the role of the dual kinase inhibitor dasatinib on human myeloid cells. Dasatinib is clinically used for the treatment of bcr/abl+ leukemias because it blocks the mutated tyrosine kinase abl. To understand its effect on the development of antigen-specific T-cell responses, we assessed antigen-specific priming of human, naïve T cells. In surprising contrast to the direct inhibition of T-cell activation by dasatinib, pretreatment of maturing dendritic cells (DCs) with dasatinib strongly enhanced their stimulatory activity. This effect strictly depended on the activating DC stimulus and led to enhanced interleukin 12 (IL-12) production and T-cell responses of higher functional avidity. Src-kinase inhibitors, and not conventional tyrosine kinase inhibitors, increased IL-12 production in several cell types of myeloid origin, such as monocytes and classical or nonclassical DCs. Interestingly, only human cells, but not mouse or macaques DCs, were affected. These data highlight the potential immunostimulatory capacity of a group of novel drugs, src-kinase inhibitors, thereby opening new opportunities for chemoimmunotherapy. These data also provide evidence for a regulatory role of src kinases in the activation of myeloid cells.
Introduction
The dual kinase inhibitor dasatinib is used widely for the treatment of bcr/abl+ leukemias. It also inhibits src kinases, which are suitable targets in solid tumors.1,2 However, src kinases are also expressed in nonmalignant cells, and their regulatory functions are diverse and not fully understood.3 Dasatinib is known for a number of clinically relevant off-target effects, owing in part to strong and paradoxical effects of the immune system.4 Hyperproliferative T-cell and natural killer (NK)-cell responses are seen frequently and are associated with severe adverse effects such as colitis, pleuritis, and pulmonary hypertension.5-7 However, the occurrence of such hyperinflammatory effects is associated with a better prognosis regarding the underlying leukemia.8 Somewhat paradoxically, the patients may experience severe functional impairment of their T cells9 because of blockade of T-cell receptor (TCR) triggering via inhibition of Lck.10-13 Chemical profiling of the drug, however, has revealed several potential binding sites to a variety of kinases, such as c-KIT, PDGFR, c-FMS, and DDR1.14-16 Therefore, despite its targeted design, this small molecule may interfere with multiple signaling pathways, leading to differential dose- and cell-dependent effects.
We recently described a young patient with bcr/abl+ acute lymphoblastic leukemia, who experienced triviral disease (cytomegalovirus, Epstein-Barr virus, and adenovirus) after haploidentical stem cell transplantation while taking dasatinib for imminent relapse.17 Despite high CD8+ counts, the infection could only be cleared once dasatinib treatment was halted. This case led us to ask whether the stimulatory and inhibitory effects of dasatinib could be the result of opposing effects on different cellular components of the immune system. Specifically, we wanted to understand the interaction of dasatinib with antigen-presenting cells, as they are essential for priming and boosting of T-cell responses. To our knowledge, there are only few studies on the effect of tyrosine kinase inhibitors on DCs.18 Appel et al demonstrated inhibition of differentiation and function of human DCs if imatinib was added to the culture.19 In contrast, Wang et al showed enhanced DC function in vitro and T-cell stimulation in vivo using a murine antigen-specific model.20 For dasatinib, only 1 study addressed its effects on monocyte-derived DCs, showing suppression of DC differentiation, when added early to the culture, leading to upregulation of the inhibitory receptor osteoactivin.21 Data on effects of other src kinase inhibitors (eg, saracatinib or bosutinib) on DCs are not available. Therefore, we analyzed the immunomodulatory capacity of clinically approved src-kinase inhibitors on myeloid antigen-presenting cells.
Methods
Cells
Peripheral blood mononuclear cells were obtained from leukapheresis products from healthy donors (consent and collection guidelines were in accordance with the Declaration of Helsinki and institutional regulations). The HLA-A0201+, Melan-A+ melanoma cell line FM55 was a gift from Dr Jürgen Becker, University of Würzburg.
Reagents and media
Cells were cultured in Cellgenix DC medium (Cellgenix, Freiburg, Germany). Human AB serum was obtained from PAA (PAA, Cölbe, Germany); 1 batch was used for all experiments.
Interleukin (IL)-4, IL-7, IL-15, and IL-21 were purchased from Peprotech (Hamburg, Germany). Granulocyte-macrophage colony-stimulating factor was purchased from Gentaur (Kampenhout, Belgium). Lipopolysaccharide (LPS) (Escherichia coli O15) was purchased from Sigma-Aldrich (Munich, Germany). Peptides were supplied by JPT Peptide Technologies (Berlin, Germany).
Dasatinib, saracatinib, bosutinib, and ENMD2076 were purchased from Selleck (Munich, Germany). For comparison, dasatinib from LC Laboratories (New York, NY) was tested with similar results (data not shown), as well as nilotinib and imatinib. Src-inhibitor 1 was purchased from Sigma-Aldrich. LPS derived from Porphyromonas gingivalis, R848, and Poly(I:C) was purchased from InvivoGen (Toulouse, France).
Cell isolation
Isolation of slan+ DCs, CD1c+ DCs, CD14+ monocytes, and CD8+ naïve T cells was performed using isolation kits from Miltenyi according to the manufacturer’s instructions (Bergisch Gladbach, Germany). Anti-APC beads were also purchased from Miltenyi. When testing different monocytes/DC fractions after direct isolation, we incubated these cells overnight in Cellgenix DC medium in the presence of granulocyte-macrophage colony-stimulating factor and IL-4 plus 5% human serum (PAA, Cölbe, Germany) and tested them the next day.
T-cell culture
The priming protocol is described in detail elsewhere.22 T-cell responses were evaluated by automated cell counting (Countess; Invitrogen, Darmstadt, Germany; trypan blue exclusion) and major histocompatibility complex (MHC) multimer staining.
Flow cytometry/intracellular cytokine staining
MHC multimers were obtained from Proimmune (Oxford, United Kingdom) and Immudex (Copenhagen, Denmark); staining with the Melan-A-multimer from both companies was comparable (data not shown). MHC multimer staining was performed at room temperature (20 minutes, 1:50 dilution), with 100 nM of dasatinib added for stabilized staining.23
Intracellular cytokine staining using standard staining conditions was performed after an incubation period under stimulating conditions of 16 hours (DCs) or 5 hours (T cells). The following antibodies were used: IL-12p40, clone C8.6 (eBioscience, San Diego, CA); IL-8, clone E8N1 (BioLegend, San Diego, CA); tumor necrosis factor α (TNFα), clone Mab11 (BioLegend); and interferon γ (IFNγ), clone 4S.B3 (BioLegend).
Multiplex assay/enzyme-linked immunosorbent assay (ELISA).
The multiplex assay (FlowCytomix; eBioscience) was performed following the instructions of the manufacturer. ELISA for IL-23, IL-12, and IL-10 was performed using commercial kits from eBioscience.
Phosphorylation-specific western blot
Cell lysate preparation and dual-color western blotting was carried out following standard protocols (as detailed in the supplemental Methods, available on the Blood Web site). Primary antibodies were as follows: phosphorylated ERK1/2 (137F5), p-p38 (3D7), p-JNK (81E11), p-IκB kinase complex α/β (IκBα/β) (16A6), IκBα, IRAK1 (D51G7), and p-IFN regulatory factor 3 (p-IRF3) (4D4G) from Cell Signaling; and β-actin from Sigma-Aldrich. Secondary antibodies conjugated with IRDye 800CW anti-rabbit or IRDye 680LT anti-mouse were purchased from LI-COR Biosciences (Bad Homburg, Germany).
The intensity of bands was quantified by ImageJ software (version 1.47g). The relative densities for the samples as well as the β-actin bands were calculated separately by normalizing relative to immature DCs. The adjusted density for each sample was calculated by dividing the relative density of each sample by that of the respective β-actin band.
Statistics.
Graph Pad Prism 5 software was used for statistical analysis. Columns generally show mean values; error bars indicate standard deviation.
Studies with animal cells
Studies outlining experiments with mouse and rhesus macaque cells are described in detail in the supplemental Methods.
Results
Dasatinib has suppressive effects on T cells but enhances the stimulatory capacity of DCs
To better understand the effects of dasatinib on T-cell priming, we implemented a robust in vitro system to assess the quantity and quality of the human naïve T-cell response against a single peptide antigen.22 Before coincubation with naïve CD8+ T cells, autologous DCs were matured for 16 hours with LPS and IFNγ and pulsed with the HLA-A0201–restricted model peptide antigen Melan-A(26-35(27L)). Melan-A, also known as MART1, is a prototypic melanosomal antigen overexpressed in melanoma. It has been targeted in many clinical studies exploring cancer immunotherapy.24 Because of altered thymic selection,25 naïve Melan-A-specific T cells can be detected in the blood at a slightly increased precursor frequency (10−4 of the naïve CD8 T cells).26 We recently validated a priming protocol that allows us to reproducibly expand these cells to an average range of 20% to 50% MHC multimer+ T cells with a single stimulation within a short expansion period of 10 to 12 days. Thus, variations from extensive restimulation procedures are eliminated, allowing the qualitative and quantitative characterization of antigen-specific T-cell responses as a result of a single, initial priming event (Figure 1A).22 The addition of dasatinib in a physiologically relevant dose (50 nM)27 on day 0 of culture completely blocked priming of Melan-A-specific T cells. Only the initial priming event (involving the TCR trigger) was blocked, whereas cytokine-driven proliferation following the TCR trigger was only slightly impaired (Figure 1B). Thus, dasatinib not only blocks effector memory T-cell function but also directly prevents antigen-specific priming of naïve T cells.12
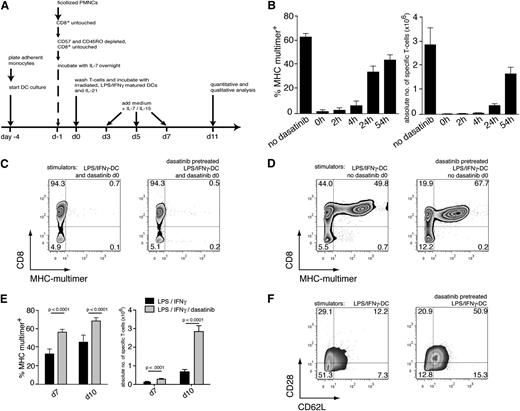
Differential effects of dasatinib on T cells and DCs. (A) A robust in vitro priming system for assessment of dasatinib-mediated effects. The protocol has been validated previously22 and is described in the “Methods” section. (B) The direct effects of dasatinib were assessed by adding a single dose of dasatinib (50 nM) at various time points after the initial coincubation of T cells and DCs. On day 10, individual wells were evaluated for MHC-multimer+ CD8+ T cells (left); this fraction was multiplied by the total number of cells per well to obtain the absolute number of antigen-specific T cells per well (right; 7 parallel wells per group, bars represent the mean with standard deviation). (C) T-cell priming with dasatinib-treated (50 nM) DCs (day −1) and addition of dasatinib (50 nM) at the time of priming resulted in complete blockade of antigen-specific T-cell proliferation. (D) T-cell priming with dasatinib-treated (50 nM) DCs (day −1), without addition to the T-cell culture, increased the percentage of MHC-multimer+ cells compared with matured DCs without dasatinib pretreatment. Before coincubation with T cells, the DCs were extensively washed to remove residual dasatinib. (E) Comparison of dasatinib-treated DCs and DCs matured with LPS/IFNγ only. Differences in the percentage of MHC-multimer+ cells and the absolute yield of antigen-specific T cells were highly significant (Student t test) on days 7 and 10 of culture (evaluation of 7 parallel wells, technical replicates). (F) Primed T cells (gated on viable CD8+ MHC-multimer+ cells) expressed higher levels of CD28 and CD62L on day 10 of culture, when naïve T cells had been primed with dasatinib-pretreated DCs as opposed to DC matured without dasatinib. Each of the results is representative of at least 3 separate experiments.
Differential effects of dasatinib on T cells and DCs. (A) A robust in vitro priming system for assessment of dasatinib-mediated effects. The protocol has been validated previously22 and is described in the “Methods” section. (B) The direct effects of dasatinib were assessed by adding a single dose of dasatinib (50 nM) at various time points after the initial coincubation of T cells and DCs. On day 10, individual wells were evaluated for MHC-multimer+ CD8+ T cells (left); this fraction was multiplied by the total number of cells per well to obtain the absolute number of antigen-specific T cells per well (right; 7 parallel wells per group, bars represent the mean with standard deviation). (C) T-cell priming with dasatinib-treated (50 nM) DCs (day −1) and addition of dasatinib (50 nM) at the time of priming resulted in complete blockade of antigen-specific T-cell proliferation. (D) T-cell priming with dasatinib-treated (50 nM) DCs (day −1), without addition to the T-cell culture, increased the percentage of MHC-multimer+ cells compared with matured DCs without dasatinib pretreatment. Before coincubation with T cells, the DCs were extensively washed to remove residual dasatinib. (E) Comparison of dasatinib-treated DCs and DCs matured with LPS/IFNγ only. Differences in the percentage of MHC-multimer+ cells and the absolute yield of antigen-specific T cells were highly significant (Student t test) on days 7 and 10 of culture (evaluation of 7 parallel wells, technical replicates). (F) Primed T cells (gated on viable CD8+ MHC-multimer+ cells) expressed higher levels of CD28 and CD62L on day 10 of culture, when naïve T cells had been primed with dasatinib-pretreated DCs as opposed to DC matured without dasatinib. Each of the results is representative of at least 3 separate experiments.
Next, we analyzed the direct influence of dasatinib on maturing DCs in the context of T-cell priming. When dasatinib was added to the DCs at the time of their maturation and again at the time of DC- or T-cell coincubation, antigen-specific T cells did not expand (Figure 1C). By incubating DCs with dasatinib during maturation only (ie, before the initial T-cell contact), we dissected the effects of dasatinib on DCs from the strong, direct inhibitory effect on T cells. Unexpectedly, antigen-specific T-cell proliferation in response to dasatinib-treated DCs was significantly higher than the responses to DCs matured with LPS/IFNγ alone (Figure 1D-E). Despite extensive proliferation, the T cells primed with dasatinib-treated DCs maintained a central memory phenotype with increased levels of CD28 and CD62L (Figure 1F). Therefore, dasatinib enhanced DC function, leading to increased antigen-specific T-cell proliferation.
Dasatinib enhances IL-12 production in DCs stimulated via Toll-like receptor (TLR) 2 and TLR4 agonists
MHC expression, expression of costimulatory molecules, and a proinflammatory cytokine signature (particularly IL-12 production) are key components of effective antigen presentation and CD8+ T-cell priming.28 Therefore, we evaluated the expression of six DC surface markers relevant to antigen presentation (CD80, CD86, CD83, CD40, CD54, and HLA-DR). No differences were observed in maturing or immature DCs after dasatinib treatment (supplemental Figure 1).
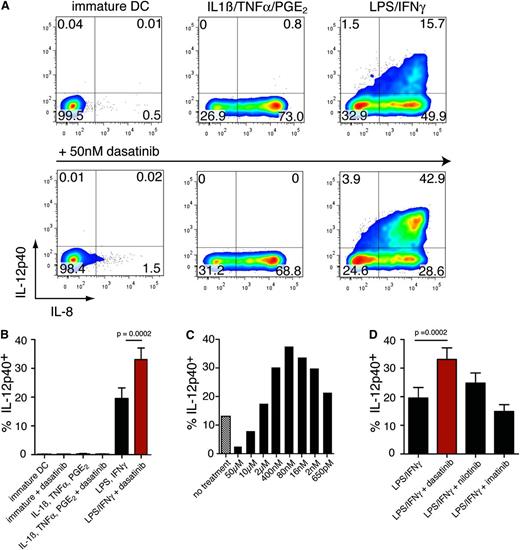
Next, we assessed IL-12 production by DCs matured with or without dasatinib using various maturation cocktails. In 10 of 10 donors, dasatinib coincubation with LPS (in combination with IFNγ) induced IL-12p40 production in a significantly higher fraction of DCs compared with DCs matured in the absence of dasatinib (P < .0001); dasatinib alone had no effect on immature DCs or on DCs matured with IL-1β, TNFα, and prostaglandin E2 (PgE2) (Figure 2A-B). We then asked whether the observed effects of dasatinib were dose dependent. As shown in Figure 2C, dasatinib enhanced IL-12 production at a dose range of 2 to 400 nM, whereas higher doses were suppressive (Figure 2C). This dose range corresponds to dasatinib serum levels in patients taking dasatinib twice daily at 70 mg, where the maximal serum level (Cmax) has been determined to be 90 nM.27 Nilotinib, another tyrosine kinase inhibitor slightly enhanced IL-12p40 production, whereas imatinib had no effect (Figure 2D).
Effects of dasatinib on DC function. (A) Effect of dasatinib on IL-12 production. DCs were matured with various maturation cocktails alone (upper row) or in the presence of dasatinib (lower panel). Intracellular IL-12p40 and IL-8 were stained after 16 hours of stimulation. (B) Analysis of 10 different donors for production of IL-12p40 assessed by intracellular cytokine staining. DCs were matured with the respective stimuli and were coincubated with dasatinib (50 nM, red bars) for 16 hours. Indicated is the mean percentage of IL-12p40+ DCs and the standard deviation. (C) Dose titration of dasatinib on maturing DCs. DCs were matured with LPS/IFNγ in combination with the indicated amounts of dasatinib (1 of 2 experiments with comparable results). (D) Effects of other tyrosine kinase inhibitors on 10 different donors. DCs were matured with LPS/IFNγ and were coincubated with 50 nM of dasatinib, 10 µM of imatinib, or 1 µM of nilotinib for 16 hours, followed by intracellular cytokine staining for IL-12p40 and TNFα.
Effects of dasatinib on DC function. (A) Effect of dasatinib on IL-12 production. DCs were matured with various maturation cocktails alone (upper row) or in the presence of dasatinib (lower panel). Intracellular IL-12p40 and IL-8 were stained after 16 hours of stimulation. (B) Analysis of 10 different donors for production of IL-12p40 assessed by intracellular cytokine staining. DCs were matured with the respective stimuli and were coincubated with dasatinib (50 nM, red bars) for 16 hours. Indicated is the mean percentage of IL-12p40+ DCs and the standard deviation. (C) Dose titration of dasatinib on maturing DCs. DCs were matured with LPS/IFNγ in combination with the indicated amounts of dasatinib (1 of 2 experiments with comparable results). (D) Effects of other tyrosine kinase inhibitors on 10 different donors. DCs were matured with LPS/IFNγ and were coincubated with 50 nM of dasatinib, 10 µM of imatinib, or 1 µM of nilotinib for 16 hours, followed by intracellular cytokine staining for IL-12p40 and TNFα.
To better understand the regulation of cytokine production in response to various inflammatory stimuli, we analyzed secretion of several cytokines relevant in DC activation. IL-12 secretion in general was strongly enhanced by combining the activating trigger with IFNγ, as the latter is known to efficiently prime the IL-12p40 promotor.29,30
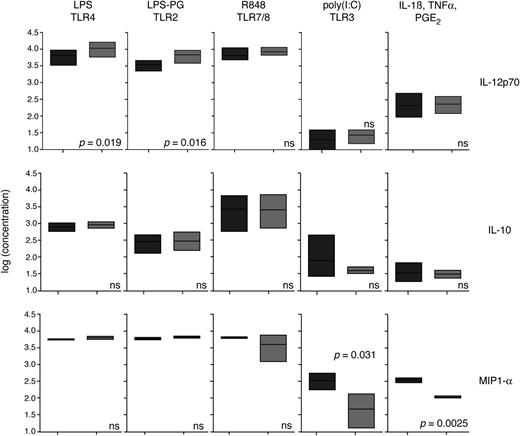
When adding dasatinib along with IFNγ to the stimulation cocktail, significantly more IL-12p70 was produced when E coli LPS (triggering via TLR4) and LPS derived from P gingivalis (triggering via TLR2) were used. No differences were observed after stimulation with R848 (TLR7/8), Poly I:C (TLR3) (regardless of additional IFNγ coincubation), or a cocktail of proinflammatory cytokines (IL1β, TNFα, and PgE2). (Figure 3 and supplemental Figure 2). Additional analysis by ELISA for IL-12, IL-10, and IL-23 in an independent set of experiments confirmed these findings (supplemental Figure 3). IFNα and IL-27 were not secreted under the chosen conditions. To summarize, we conclude that dasatinib specifically enhances TLR2 and TLR4 agonist–mediated IL-12 production but exerts no stimulatory activity by itself.
Production of cytokines by DCs matured with different TLR agonists with or without dasatinib. Immature DCs were stimulated with the respective TLR agonist: LPS (10 ng/mL), LPS derived from P gingivalis (1 µg/mL), Poly(I:C) (1 µg/mL) or R848 (2 µg/mL) combined with IFNγ (100 U/mL), or a cytokine cocktail consisting of IL1β (20 ng/mL), TNFα (20 ng/mL), and PgE2 (20 μg/mL). Either no dasatinib (dark gray) was added or dasatinib (50 nM) was added (light gray). At 16 hours later, supernatant was collected and was frozen for subsequent analysis. Analysis was performed using the FlowCytomix Bead Array (eBiosciences), following the instructions of the manufacturer. Data from 3 different experiments were analyzed. Values were transformed using the log of each measurement and were statistically evaluated by a paired t test. Data on cytokine production with similar stimulation conditions, but without IFNγ, are provided in supplemental Figure 2.
Production of cytokines by DCs matured with different TLR agonists with or without dasatinib. Immature DCs were stimulated with the respective TLR agonist: LPS (10 ng/mL), LPS derived from P gingivalis (1 µg/mL), Poly(I:C) (1 µg/mL) or R848 (2 µg/mL) combined with IFNγ (100 U/mL), or a cytokine cocktail consisting of IL1β (20 ng/mL), TNFα (20 ng/mL), and PgE2 (20 μg/mL). Either no dasatinib (dark gray) was added or dasatinib (50 nM) was added (light gray). At 16 hours later, supernatant was collected and was frozen for subsequent analysis. Analysis was performed using the FlowCytomix Bead Array (eBiosciences), following the instructions of the manufacturer. Data from 3 different experiments were analyzed. Values were transformed using the log of each measurement and were statistically evaluated by a paired t test. Data on cytokine production with similar stimulation conditions, but without IFNγ, are provided in supplemental Figure 2.
Priming with dasatinib-pretreated mature DCs leads to enhanced Tc1-skewed immune responses
Our original observation was based on the quantitative assessment of the CD8+ T-cell response when using dasatinib-pretreated DCs. We next sought to investigate the quality of the resulting T-cell response in more detail. Dasatinib alone had no effect on immature DCs, and when testing such DCs, the resulting T-cell responses remained low (Figure 4A). This finding rules out potential artifacts (eg, by accidental contamination of the dasatinib preparation with LPS). Furthermore, different batches of dasatinib from 2 different vendors led to similar results regarding DC activation and T-cell responses (data not shown). Next, we wanted to exclude the possibility that, instead of a direct effect on DCs, the observed effect was indirectly mediated by mechanisms related to contaminating NK cells or regulatory T cells within the initial DC preparation. Therefore, we purified 4-day cultured, immature DCs with CD11c-targeting magnetic beads to obtain a highly purified DC population (>95%) and only then induced maturation using LPS/INFγ with or without dasatinib. Again, dasatinib-treated mature DCs were better stimulators than DCs matured with LPS/INFγ alone (Figure 4B), arguing for a direct effect on the maturing DCs.
Qualitative effects of dasatinib-treated DCs on T-cell priming (day 10 of culture). (A) Dasatinib does not improve the priming capacity of immature DCs. Shown are T-cell responses with differentially treated immature DCs. (B) Effects after dasatinib treatment are not the result of contaminating bystander cells. Immature DCs were harvested, stained with APC-labeled anti-CD11c-antibodies, and purified with anti-APC-beads (>95% purity) and only then matured. (C) Dasatinib-associated effects are mediated in trans. Melan-A peptide–pulsed DCs were either matured with LPS/IFNγ alone or coincubated with dasatinib. Melan-A-pulsed, LPS/IFNγ–matured DCs were mixed with LPS/IFNγ–matured DCs pulsed with a mock peptide (STEAP1(292.2L)) or with dasatinib/LPS/IFNγ–matured DCs pulsed with the mock peptide at a 1:1 ratio. (D) T cells primed with dasatinib-pretreated DCs have higher functional avidity. Responses to titrated peptide onto CD14+ monocytes (IFNγ+ response normalized for MHC-multimer+ cells). (E) Avidity testing using Melan-A+ melanoma cells (FM55, HLA-A2+, Melan-A+) at a 2:1 Effector:Target ratio (5-hour stimulation). Zebra plots show the MHC-multimer staining of the unstimulated cell lines. Pseudocolor plots show the stimulated cells gated on live, CD8+ T cells (in brackets: IFNγ+TNFα+ T cells normalized for the MHC-multimer+cells). First row: T cells primed with DCs matured with LPS/IFNγ (left) vs DCs matured with dasatinib/LPS/IFNγ. Middle row: Identical maturation conditions plus 5 μg/mL of neutralizing IL-12 antibody at the time of priming. Last row: DCs matured with IL1β, TNFα, and PgE2 in the absence or presence of dasatinib were used for priming. Results are representative for at least 3 independent experiments.
Qualitative effects of dasatinib-treated DCs on T-cell priming (day 10 of culture). (A) Dasatinib does not improve the priming capacity of immature DCs. Shown are T-cell responses with differentially treated immature DCs. (B) Effects after dasatinib treatment are not the result of contaminating bystander cells. Immature DCs were harvested, stained with APC-labeled anti-CD11c-antibodies, and purified with anti-APC-beads (>95% purity) and only then matured. (C) Dasatinib-associated effects are mediated in trans. Melan-A peptide–pulsed DCs were either matured with LPS/IFNγ alone or coincubated with dasatinib. Melan-A-pulsed, LPS/IFNγ–matured DCs were mixed with LPS/IFNγ–matured DCs pulsed with a mock peptide (STEAP1(292.2L)) or with dasatinib/LPS/IFNγ–matured DCs pulsed with the mock peptide at a 1:1 ratio. (D) T cells primed with dasatinib-pretreated DCs have higher functional avidity. Responses to titrated peptide onto CD14+ monocytes (IFNγ+ response normalized for MHC-multimer+ cells). (E) Avidity testing using Melan-A+ melanoma cells (FM55, HLA-A2+, Melan-A+) at a 2:1 Effector:Target ratio (5-hour stimulation). Zebra plots show the MHC-multimer staining of the unstimulated cell lines. Pseudocolor plots show the stimulated cells gated on live, CD8+ T cells (in brackets: IFNγ+TNFα+ T cells normalized for the MHC-multimer+cells). First row: T cells primed with DCs matured with LPS/IFNγ (left) vs DCs matured with dasatinib/LPS/IFNγ. Middle row: Identical maturation conditions plus 5 μg/mL of neutralizing IL-12 antibody at the time of priming. Last row: DCs matured with IL1β, TNFα, and PgE2 in the absence or presence of dasatinib were used for priming. Results are representative for at least 3 independent experiments.
Next, we determined whether improved priming only occurred when cognate peptide was presented by dasatinib-treated DCs themselves (in cis), or whether these DCs could “assist” DCs not previously treated with dasatinib (in trans). When dasatinib-pretreated DCs not presenting the relevant antigen were mixed with untreated Melan-A-pulsed DCs matured without dasatinib, the resulting T-cell response to the Melan-A peptide was significantly higher than in the groups, in which none of the DC populations had been pretreated with dasatinib, indicating “assistance” of dasatinib-pretreated DC (Figure 4C).
We then wanted to test the functional avidity of T-cell lines induced by differentially treated DCs. T cells primed with different DC preparations were tested for their cytokine response to titrated amounts of peptide pulsed onto autologous cytokine-activated monocytes. T cells that had been initially primed with dasatinib-pretreated LPS/IFNγ–matured DCs had a higher functional avidity than T cells primed with LPS/IFNγ–matured DCs (EC50 (LPS/IFNγ): 1.5e−10 M; EC50 (LPS/IFNγ/dasatinib: 4.7e−11 M; Figure 4D).
We next asked whether the resulting T cells differed in their ability to recognize tumor cells that express the relevant antigen endogenously. Therefore, we coincubated the T cells with the Melan-A+, HLA-A0201+ melanoma cell line FM55 at an effector-to-target ratio of 4:1 and assessed intracellular cytokine production in the antigen-specific T cells. T cells that had been primed with dasatinib-pretreated DC 11 days earlier responded better to the tumor cells than T cells primed with standard LPS/INFγ–matured DC (Figure 4E, upper row). Because increased IL-12 production was a potential reason for this improved functionality, we blocked IL-12 at the time of priming by adding neutralizing IL-12 antibody. In fact, although expansion of MHC multimer+ cells was still good, the functionality of the T cells was reduced (Figure 4E, middle row).
However, T cells stimulated with DCs matured without dasatinib were more sensitive to the effects of the blocking IL-12 antibody than T cells stimulated with dasatinib-coincubated DCs. This finding is a good argument for incomplete blockade of excess IL-12 by the antibody, especially at the immunologic synapse, but may also indicate additional factors to be relevant for optimal priming. We conclude that enhanced IL-12 production was at least partly responsible for improved T-cell priming. For comparison, DCs matured with proinflammatory cytokines produced no detectable IL-12 (Figure 2C-D) and, in consequence, were poor stimulators. Dasatinib pretreatment of these DCs did not restore stimulatory function; therefore, synergistic activity of dasatinib is restricted to TLR-mediated DC activation (Figure 4E, lower row).
Dasatinib enhances nuclear factor κB (NF-κB) signaling in maturing DCs
Imatinib, the first-generation tyrosine kinase inhibitor, has been shown to inhibit DC differentiation and function.31 In line with these findings, we did not observe any stimulatory activity when using imatinib (Figure 2D). In contrast to imatinib, dasatinib is designed as a dual kinase inhibitor not only targeting bcr/abl but also targeting src kinases. In addition, more than 30 potential targets have been described.4,14 To better understand phosphorylation patterns of receptor tyrosine kinases in DCs in response to inflammatory stimuli, we evaluated differentially treated DCs for receptor tyrosine kinase phosphorylation using a phosphoarray approach. In this screening experiment, however, no differential effect of dasatinib vs treatment with nilotinib or maturation with proinflammatory cytokines was observed (supplemental Table 1).
Next, we screened a library of tyrosine kinase inhibitors focusing on groups of inhibitors with an overlapping functional profile compared with dasatinib. Src kinase inhibitors as a group uniformly enhanced TLR4-mediated IL-12p40 production in DCs even exceeding the dasatinib-mediated effects. Other groups of compounds had a far more diverse effect, with some compounds enhancing and some suppressing IL-12 production, or having no effect at all (Figure 5A; supplemental Table 2). This finding is a good argument for involvement of src-kinases in the regulation of IL-12 synthesis in TLR2/4-triggered DC activation.
Biochemical effects of dasatinib and other src inhibitors. (A) Src inhibitors enhance IL-12p40 production in LPS/IFNγ–matured DCs. Different src kinase family inhibitors were tested in combination with LPS/IFNγ maturation. DCs were matured with LPS/IFNγ in the presence of the respective inhibitor (1.25 μM) and brefeldin A for 16 hours. Subsequently, Intracellular cytokine staining was performed. Data were pooled from 3 independent experiments. (B) Dasatinib added at the time of the activation stimulus leads to the highest synergistic activity. Dasatinib was added to DCs matured with LPS/IFNγ at the indicated time points, followed by IL-12p40 staining 16 hours after stimulation. Pooled data from 3 experiments. (C) Effects of dasatinib on mitogen-activated protein kinase phosphorylation. Dasatinib was added together with the maturation stimulus LPS/IFNγ. Six hours later, cell lysates were obtained and phosphorylation-specific western blots were carried out. Std.: standard maturation conditions with LPS/IFNγ. Mix: use of IL1β, TNFα, and PgE2 for stimulation. β-Actin served as a loading control (for quantitative evaluation, see supplemental Figure 4A). (D) Dasatinib enhances NF-κB signaling. Dasatinib was added together with the maturation stimulus LPS/IFNγ. Six hours later, cell lysates were obtained and phosphorylation of IκBα/β as well as degradation of IkBα was assessed. β-Actin served as a loading control (for quantitative evaluation, see supplemental Figure 4B). (E) Dasatinib enhances phosphorylation of IRF3. Dasatinib was added together with the maturation stimulus LPS/IFNγ. At the indicated time points (minutes), cell lysates were obtained and phosphorylation of IRF3 as well as degradation of IRAK1 was assessed (for quantitative evaluation, see supplemental Figure 4B).
Biochemical effects of dasatinib and other src inhibitors. (A) Src inhibitors enhance IL-12p40 production in LPS/IFNγ–matured DCs. Different src kinase family inhibitors were tested in combination with LPS/IFNγ maturation. DCs were matured with LPS/IFNγ in the presence of the respective inhibitor (1.25 μM) and brefeldin A for 16 hours. Subsequently, Intracellular cytokine staining was performed. Data were pooled from 3 independent experiments. (B) Dasatinib added at the time of the activation stimulus leads to the highest synergistic activity. Dasatinib was added to DCs matured with LPS/IFNγ at the indicated time points, followed by IL-12p40 staining 16 hours after stimulation. Pooled data from 3 experiments. (C) Effects of dasatinib on mitogen-activated protein kinase phosphorylation. Dasatinib was added together with the maturation stimulus LPS/IFNγ. Six hours later, cell lysates were obtained and phosphorylation-specific western blots were carried out. Std.: standard maturation conditions with LPS/IFNγ. Mix: use of IL1β, TNFα, and PgE2 for stimulation. β-Actin served as a loading control (for quantitative evaluation, see supplemental Figure 4A). (D) Dasatinib enhances NF-κB signaling. Dasatinib was added together with the maturation stimulus LPS/IFNγ. Six hours later, cell lysates were obtained and phosphorylation of IκBα/β as well as degradation of IkBα was assessed. β-Actin served as a loading control (for quantitative evaluation, see supplemental Figure 4B). (E) Dasatinib enhances phosphorylation of IRF3. Dasatinib was added together with the maturation stimulus LPS/IFNγ. At the indicated time points (minutes), cell lysates were obtained and phosphorylation of IRF3 as well as degradation of IRAK1 was assessed (for quantitative evaluation, see supplemental Figure 4B).
We then asked whether timing of dasatinib coincubation with the TLR trigger was relevant for synergistic enhancement. Indeed, dasatinib-mediated effects were most pronounced when added at the time of DC stimulation, whereas the addition of dasatinib at later time points (eg, 3-6 hours after LPS stimulation) led to a gradually lower response (Figure 5B). Therefore, the synergistic effect is closely connected to the activating trigger.
IL-12 production in DCs can be modulated either by modification of mitogen-activated protein kinases erk, jnk, or p38, or by modified NF-κB signaling. Phosphorylation-specific western blots revealed only a slight increase of erk1/2 and jnk phosphorylation and reduced phosphorylation of p38 in response to dasatinib cotreatment. However, IκBα/β phosphorylation was strongly increased after dasatinib treatment, whereas IκBα protein expression was reduced, indicating enhanced NF-κB signaling by dasatinib (Figure 5C-D; supplemental Figure 4).
Because enhanced IL-12 production was restricted to TLR2 or TLR4 agonists (Figures 2 and 3), we asked whether dasatinib regulates the classical MyD88-associated pathway or the alternative TIR-domain-containing adapter inducing IFN-β (TRIF)–associated pathway. To answer this question, we performed western blots on IRAK1 to assess the extent of MyD88 activation and also determined phosphorylation of IRF3, which qualifies as an upstream checkpoint of the TRIF pathway.32 On LPS/IFNγ stimulation, IRAK1 was degraded within 15 minutes regardless of dasatinib coincubation. However, TRIF-associated IRF3 phosphorylation was increased in the presence of dasatinib within 60 to 90 minutes after stimulation (Figure 5E; supplemental Figure 3). In conclusion, enhanced IL-12 production following src-kinase inhibition in combination with the appropriate activation stimulus is predominantly regulated via enhanced TRIF signaling, which, when combined with MyD88 signaling, leads to rapid and enhanced activation of the NF-κB pathway.
Synergistic enhancement of IL-12 production by dasatinib is observed in various myeloid cell types
Next, we asked whether the effects of dasatinib on in vitro–activated, monocyte-derived DCs differed from the effects on myeloid cell subsets isolated directly from the peripheral blood. CD14+ monocytes, slan+CD14low DCs,33,34 and CD1c+ myeloid DCs represent a significant pool of antigen-presenting cells within the peripheral blood. We purified these cell subsets and stimulated the cells with LPS/INFγ with or without dasatinib. Similar to our results with in vitro–generated DCs, dasatinib clearly increased IL-12p40 production in these myeloid cell subsets. In particular, slan+ DCs strongly increased their IL-12 production, which is in line with the notion that this cell type may represent an important inflammatory DC subset33 (Figure 6A).
Effects of dasatinib on various myeloid cell subsets. (A) CD14+ monocytes, CD1c+ myeloid DCs, and slan+ DCs were purified from peripheral blood mononuclear cells. After overnight culture, the cells were stimulated with LPS/IFNγ with or without 50 nM of dasatinib and were tested for cytokine production after 16 hours. (B) Dasatinib sensitizes different cells of myeloid origin for suboptimal LPS triggering. CD14+ monocytes were subjected to maturation with titrated amounts of LPS in the absence or presence of dasatinib (50 nM). IL-12p40 production was detected after 16 hours of maturation. Results are representative for at least 3 experiments.
Effects of dasatinib on various myeloid cell subsets. (A) CD14+ monocytes, CD1c+ myeloid DCs, and slan+ DCs were purified from peripheral blood mononuclear cells. After overnight culture, the cells were stimulated with LPS/IFNγ with or without 50 nM of dasatinib and were tested for cytokine production after 16 hours. (B) Dasatinib sensitizes different cells of myeloid origin for suboptimal LPS triggering. CD14+ monocytes were subjected to maturation with titrated amounts of LPS in the absence or presence of dasatinib (50 nM). IL-12p40 production was detected after 16 hours of maturation. Results are representative for at least 3 experiments.
Physiologically, antigen-presenting cells are required to sense ultralow doses of endotoxin to mount a sufficient immune response. We wanted to know whether dasatinib renders monocytes more sensitive to LPS by dasatinib. As demonstrated in Figure 6B, in combination with IFNγ, significantly less LPS was required for dasatinib-incubated monocytes to stimulate equal numbers of IL-12p40-producing cells (Figure 6B). Thus, dasatinib is capable of sensitizing myeloid antigen-presenting cells to LPS-mediated activation.
Mouse and rhesus macaque DCs respond differently to dasatinib than human DCs
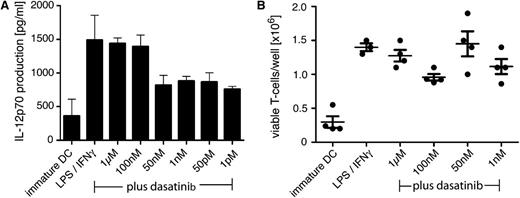
We then wanted to analyze the effects of dasatinib in an animal model. However, before proceeding with in vivo experiments, we first evaluated the effects of dasatinib on murine DCs in vitro. DCs derived from the C57Bl/6 mice and TCR transgenic T cells, specific for the pmel epitope/mgp(25-33), obtained from B6.pmel-1 mice were used.35 In vitro differentiated, bone marrow–derived mouse DCs were tested for synergistic activity of dasatinib combined with LPS/INFγ as a maturation stimulus. Figure 7A shows no enhancement of IL-12p70 production in murine DCs when adding varying concentrations of dasatinib (Figure 7A). In consequence, when testing murine DCs for their stimulatory activity of T cells, we observed no difference in the proliferation rate of murine antigen-specific T cells in response to differentially matured DCs regardless of dasatinib treatment (Figure 7B). We then decided to address this question in nonhuman primates. Again, when probing DCs from rhesus macaques for IL-12, we detected no significant effect of dasatinib treatment (supplemental Figure 5). These data suggest that human DCs are particularly sensitive to src-kinase inhibitors and that significant species-specific differences in the regulation of DC activation by src-kinases may exist.
Dasatinib has no stimulatory effect on mouse DCs. (A) Immature DCs were generated from C57Bl/6.CD45.1 bone marrow cells and matured overnight with 100 ng/mL of LPS and 100 IU/mL of INFγ with or without titrated doses of dasatinib. After 16 hours, supernatant was collected and the IL-12p70 concentration was evaluated by ELISA (pooled data from 3 experiments). (B) Splenic T cells from C57Bl/6.pmel-1 mice, engineered to all express a TCR specific for the mgp100-peptide, were isolated and cocultured with gp100-loaded, differentially treated DCs for 96 hours. Then viable T cells were counted using an automated cell counter (data represent technical replicates, representative for 3 independent experiments).
Dasatinib has no stimulatory effect on mouse DCs. (A) Immature DCs were generated from C57Bl/6.CD45.1 bone marrow cells and matured overnight with 100 ng/mL of LPS and 100 IU/mL of INFγ with or without titrated doses of dasatinib. After 16 hours, supernatant was collected and the IL-12p70 concentration was evaluated by ELISA (pooled data from 3 experiments). (B) Splenic T cells from C57Bl/6.pmel-1 mice, engineered to all express a TCR specific for the mgp100-peptide, were isolated and cocultured with gp100-loaded, differentially treated DCs for 96 hours. Then viable T cells were counted using an automated cell counter (data represent technical replicates, representative for 3 independent experiments).
Discussion
The interplay between chemotherapy and immune effector mechanisms, called chemoimmunotherapy, holds promise to amplify current treatment strategies against cancer.36,37 Although so-called targeted therapies claim high specificity, interference with other pathways often leads to significant adverse effects. Our study reveals a dual effect of src-kinase inhibitors on 2 essential subsets of the immune system: T cells and antigen-presenting cells. Dasatinib inhibits TCR triggering in T cells by blocking the src-kinase Lck.38 However, studies addressing the effects of tyrosine kinase inhibitors on DCs are controversial.18 Our data now clearly demonstrate a stimulatory mechanism for dasatinib and other src-kinase inhibitors, which is strictly dependent on the mode of DC activation, suggesting interference with specific regulatory pathways.
Our data provide an explanation for the observed paradoxical role of dasatinib during therapy for patients with bcr/abl+ leukemia. Enhanced activation of the large pool of myelomonocytic cells, responding to the drug, may account for the effects. Increased IL-12 secretion from myeloid cells may start a cytokine cascade, leading to an increase in CD8+ T cells and NK cells. Inflammatory conditions and elevated cytokine levels are also common in the pathologic patterns of pulmonary arterial hypertension39,40 ; therefore, it will be interesting to analyze patient samples of dasatinib-induced pulmonary hypertension to determine the underlying mechanism for this severe condition.
Although the inhibitory effect on T cells is profound, our recent data indicated a short-lived direct effect in vivo.17 Plasma half-life is reported to be only 3 to 4 hours.27 Moreover, data presented in our current study show that cytokine-driven proliferation was barely affected when dasatinib was added 24 hours after TCR triggering (Figure 1). Therefore, it is conceivable that once the suppressive effect on T cells wears off, secreted IL-12 may be the driving factor. Bacterial infection or viral reactivation such as cytomegalovirus, which has been reported to be associated with dasatinib-induced hyperleukocytosis,6 would qualify as the inflammatory trigger. In concert with the described inhibition of regulatory T cells by dasatinib, as reported in vitro41 and in vivo,42 these mechanisms may lead to unrestricted CD8 proliferation in the clinical setting, along with a better clinical response against the underlying leukemic disease.5,43
The exact regulation of IL-12 synthesis on TLR-mediated activation in DCs is still not fully understood.44 The NF-κB pathway is one of the critical signaling pathways for the synthesis of IL-12. Our data provide mechanistic evidence that src-kinases are involved in the regulation of TRIF/MyD88–dependant NF-κB activation. Because dasatinib alone has no direct stimulatory activity on DCs, we expect that 1 or several pathways regulating NF-κB activation are induced by src kinases as a negative regulatory feedback mechanism. Src-kinase inhibitors in consequence would block these negative immune regulators, thus leading to excess TLR triggering. Which of the 4 src kinases, known to be expressed in DCs, Fgr, Hck, Src, and Lyn,3 are involved in this process and how such a putative negative feedback loop is initiated by TLR triggering is currently being investigated in our laboratory. That mouse and rhesus macaques DCs respond differently to the drug highlights potential interspecies differences, which need to be carefully taken into account during preclinical testing.
In summary, our data provide a reasonable explanation for the paradoxical role of dasatinib on the immune system. The synergistic effects with TLR triggers add to the complexity of this drug in the clinical setting. These data also point toward a regulatory role of src kinases in specific activation pathways in human myeloid cells. On the basis of these data, we hypothesize that the development of a new class of a molecularly designed vaccine might be appealing. Local application of src-inhibitors in combination with TLR agonists would not compromise the systemic T-cell function but would improve the activation of resident antigen-presenting cells. Moreover, targeted delivery of antigen and src-inhibitors (eg, using DEC-205-constructs combined with PLGA nanoparticles45 ) may greatly reduce the inhibitory activity on T cells. For cancer therapy, rational inclusion of such immunostimulatory drugs will allow the design of treatment regimens that use both chemotherapeutic and immunologic strategies in a combined approach.
The online version of this article contains a data supplement.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked ‘‘advertisement’’ in accordance with 18 USC section 1734.
Acknowledgments
The authors thank the patients and their families, who inspired this work.
This work was largely supported and funded by the parent’s initiative “Aktion Regenbogen für leukämie- und tumorkranke Kinder Main-Tauber e.V.” This work was also funded by a program project grant from BayImmuNet (F2-F5121.7.1.1/13/1/2009) (M.W. and P.G.S.) and an unrestricted educational grant from the parent’s Initiative “Elterninitiative Leukämie- und tumorkranker Kinder Würzburg e.V.” Additional grant support includes Deutsche Forschungsgemeinschaft (SFB TR52 Z2) and Interdisciplinary Center for Clinical Research Würzburg (A.B.); and the National Cancer Institute, National Institutes of Health (HHSN261200800001E) (V.A. and C.O.). M.B. is a fellow of the Else-Kröner-Forschungskolleg Würzburg for Translational Immunology. M.W. was supported by an American Society of Hematology/European Hematology Translational Research Training Award 2011.
The content of this publication does not necessarily reflect the views or policies of the Department of Health and Human Services, nor does mention of trade names, commercial products, or organizations imply endorsement by the US Government.
Authorship
Contribution: M.W. designed, performed, and analyzed the experiments and wrote the paper; S.S., Y.-E.Y., M.L.R., M.B., and S.C.S. performed and analyzed the experiments; M.C., A.B., V.I.A., and C.O. performed and analyzed the experiments with mouse and monkey cells; and M.E. and P.G.S. analyzed the experiments and assisted with writing the manuscript.
Conflict-of-interest disclosure: The authors declare no competing financial interests.
Correspondence: Matthias Wölfl, Children’s Hospital, University of Würzburg, Josef-Schneider-Strasse 2, 97080 Würzburg, Germany; e-mail:woelfl_m@klinik.uni-wuerzburg.de.