In this issue of Blood, Gutsaeva and colleagues demonstrate the role of nitric oxide (NO) to suppress and hypoxia to promote adhesion of sickle erythrocytes to blood vessels in the bone marrow of mice, visualized by intravital microscopy.1
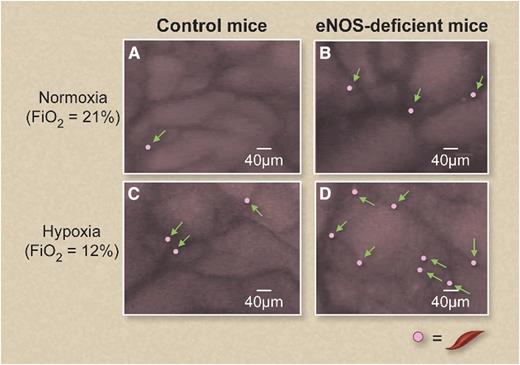
Sickle erythrocytes become adherent (arrows) to bone marrow venules in eNOS-deficient mice infused with labeled sickle cell blood compared with control mice. The number of adherent sickle erythrocytes increases in both control (A,C) and eNOS-deficient (B,D) mice under experimental hypoxia (C-D). This figure has been adapted with color enhancement from Figure 3B in the article by Gutsaeva et al that begins on page 1917. Professional illustration by Debra T. Dartez.
Sickle erythrocytes become adherent (arrows) to bone marrow venules in eNOS-deficient mice infused with labeled sickle cell blood compared with control mice. The number of adherent sickle erythrocytes increases in both control (A,C) and eNOS-deficient (B,D) mice under experimental hypoxia (C-D). This figure has been adapted with color enhancement from Figure 3B in the article by Gutsaeva et al that begins on page 1917. Professional illustration by Debra T. Dartez.
Circulating blood cells are recruited to sites of inflammation by vascular endothelium cell surface selectins and cell adhesion molecules (CAMs), which are excessively activated in sickle cell disease and some other disorders. Under normal conditions, P-selectin, E-selectin, vascular cell adhesion molecule 1, and intercellular adhesion molecule 1 and other family members are expressed at low levels. During infection, activated inflammatory cells in flowing blood “roll” in the postcapillary venules from one selectin to another until they anchor on the high-affinity, low-density CAMs. These mechanisms direct an appropriate inflammatory response to sites of infection to eliminate bacteria and other infectious pathogens. However, these adhesion pathways can become activated inappropriately in some disease states.
There remains little doubt that the primary pathophysiology in sickle cell disease involves red cell rigidity caused by polymerization of sickle hemoglobin, but evidence has mounted in the past 2 decades indicating an important role in sickle cell disease for excessive cell adhesion, first reported by Hoover et al2 and independently by Hebbel et al.3 Embury’s group first showed the importance of P-selectin in adherence of sickle erythrocytes to cultured endothelial cells and in sickle cell mice.4 Much additional evidence has supported the role of selectins and several other cell surface adhesion and bridging proteins that are expressed at high levels in sickle cell mice and humans.5 In adults with sickle cell disease, plasma soluble adhesion molecules serve as a biomarker of organ dysfunction and risk of mortality.6
What causes adhesion mechanisms to become activated in sickle cell disease? Several different pathways are dysregulated in sickle cell disease that activate cell adhesion. For example, interleukin 1 and tumor necrosis factor α are variably reported to be highly expressed in sickle cell disease, and these are known to activate expression of selectins and other adhesion components. The normal repression of endothelial activation by NO is impaired in sickle cell disease. NO bioavailability is reduced in sickle cell disease through both NO consumption and synthetic limitations. Intravascular hemolysis in sickle cell disease releases into plasma cell-free hemoglobin, which scavenges NO; arginase-1, which depletes arginine, the substrate for NO synthase; and asymmetric dimethylarginine, which inhibits NO synthase.7 In addition, NO is also consumed in reactions with oxygen radicals deriving from increased activity of xanthine oxidase and NADPH oxidase, from tissue ischemia-reperfusion injury, and from Fenton reactions involving heme-derived iron.7 There are also some signs of NO synthase uncoupling because of depletion of its cofactor tetrahydrobiopterin and its substrate l-arginine.
In the work published in this issue, Gutsaeva et al experimentally isolate the effects of NO deficiency upon vascular adhesion by infusing sickle blood into mice deficient in endothelial NO synthase (eNOS). In bone marrow blood vessels observed under intravital microscopy, more sickle erythrocytes became immobilized in the eNOS-deficient mice than in the wild-type mice (see figure). Sickle cell adhesion to blood vessels increased even further under experimental hypoxia, replicating tissue conditions relevant to sickle cell patients and mice.1
Endothelial P-selectin played a significant role in this model of cell adhesion regulated by hypoxia and NO. Gutsaeva et al observed that hypoxia induced P-selectin cell surface expression on cultured endothelial cells and promoted adhesion to sickle erythrocytes. A blocking antibody directed against P-selectin prevented sickle erythrocyte adhesion in the eNOS-deficient mice.
Can NO replacement therapy reverse adhesion and vaso-occlusion? Gutsaeva et al found that NO treatment inhibited P-selectin expression on cultured endothelial cells and reduced sickle cell adhesion. Administration of NO gas at 4 ppm also reduced sickle cell adhesion in the eNOS-deficient mice. This apparent benefit of inhaled NO in mice might spark an idea for a clinical trial of inhaled NO in patients with sickle cell disease during sickle cell vaso-occlusive pain crisis; however, exactly such a prospective, multicenter, randomized, double-blind trial was recently conducted, with no evidence of benefit.8 One possible explanation for this discrepancy is that NO deficiency might be more readily corrected in the eNOS null mice that have an isolated deficit in NO production, compared with patients with sickle cell disease who have NO resistance because of accelerated consumption of NO by free hemoglobin and oxygen radicals.
The current findings call attention in the sickle cell field to the intersection of NO, hypoxia, and P-selectin pathways on vaso-occlusion. Several P-selectin antagonists have entered early phase clinical trials for vaso-occlusion in patients with sickle cell disease. An oral P-selectin blocker showed signs of improved microcirculation and endothelial activation.9 Numerous publications have reported activity of the pan-selectin inhibitor GMI-1070 in sickle cell model systems, and preliminary results of a prospective, randomized, multicenter, double-blind phase 2 study in sickle cell vaso-occlusive pain crisis suggest that GMI-1070 significantly reduced opioid usage, with a trend toward shorter duration of pain.10 Results from animal models and early phase clinical trials must always be interpreted very cautiously, but several researchers and pharmaceutical companies are “selectin” this pathway for future clinical studies in sickle cell disease.
Conflict-of-interest disclosure: The author declares no competing financial interests.