Abstract
Despite recent advances in care, central nervous system (CNS) lymphoma remains a disease with very poor long-term outcomes. We reviewed outcomes at our centre following the adoption of autologous stem cell transplant (ASCT) for patients achieving remission.
Records for 78 consecutive unselected patients diagnosed with cerebral diffuse large B-cell lymphoma (DLBCL) between 2003-2014 were analyzed. 62 of these patients did not undergo ASCT. The median age for the non-ASCT group was 60 years (range 26-80, 32 males, 30 females). Of these 50 had primary CNS lymphoma (PCNSL) and 12 cases had isolated CNS relapse after systemic lymphoma. 5 patients were HIV positive, and 4 patients had post-transplant lymphoproliferative disease. 30 patients received HD-MTX alone and 3 patients received whole brain radiotherapy (WBRT) alone. 10 patients received HD-MTX with salvage WBRT on relapse and 1 patient with CNS relapse post BEAM autograft for systemic disease received HD-MTX & WBRT. 14 patients received palliative treatment and 2 unknown.
The remaining 16 DLBCL patients and an additional 3 with mantle cell (2) or ALK positive anaplastic lymphoma (median age 53, range 27-67, male: female 13:6) who were in remission (VGPR/CR) by MRI with adequate performance status (PS) underwent ASCT after HD-MTX-based induction therapy, conditioned with 400mg/m2 BCNU & 10mg/kg Thiotepa. 4 received WBRT post-ASCT as adjuvant therapy. Of the 19 ASCT patients 16 presented with PCNSL, 2 late relapses confined to the CNS following prior systemic DLBCL, 1 mantle cell showed evidence of low-level disease on bone marrow biopsy and all were HIV negative.
Median CD34 cell dose was 4.48 x 106. Median times to neutrophil and platelet engraftment were 12 (range 10-57) and 15.5 (range 7-57) days respectively. No deaths occurred from transplant-related complications, including sepsis. 2 year PFS was 67% and OS was 73%. 4 patients relapsed post-transplant (21%), all within 4 months of transplant; 3 subsequently died. 1 patient developed systemic disease progression at time of ASCT and 1 had evidence of a mixed response on MRI pre-ASCT. No patients in CR pre-ASCT have relapsed and 1/11 PR patients has relapsed. The longest remission is now 64 months without use of WBRT, providing evidence for durable long-term response and possible cure in an unselected group of patients.
For the non-ASCT patients, median OS post diagnosis was 2.5 months overall, and 7.5 months, excluding palliative patient. Of those receiving MTX therapy 7 achieved CR, 7 PR and 23 had PD. 3 patients failed to tolerate treatment. Of those who achieved CR/PR reasons for not proceeding to ASCT included inadequate PS or lack of willingness to receive further therapy. Outcomes for those who achieve CR are good, with median PFS & OS for patients achieving CR not reached at a median of 32 months follow-up. 5/7 remain in remission; 1 patient has died. Only 1 of these patients received WBRT. The median PFS & OS for patients achieving PR were 5.5 & 8 months respectively (p= 0.041 & 0.027 vs CR).
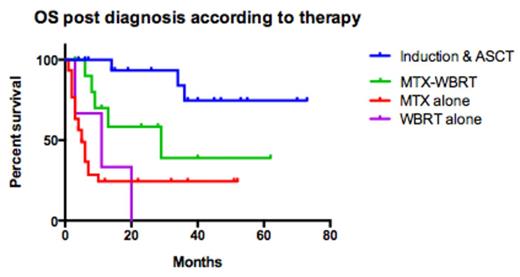
When comparing the two groups, median OS for patients receiving ASCT was not reached vs 5 months for MTX alone (p<0.001) and 29 months for MTX & WBRT (p=0.013).
Overall we conclude MTX therapy alone induces CR in only a small number of patients and outcomes for those not achieving CR are dismal. For patients who are able to proceed to ASCT long-term remissions can be obtained. New strategies are required to enable patients to achieve CR in order to receive ASCT and thus achieve a durable long-term survival from CNS lymphoma.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal