Abstract
Background: Previous studies have shown that the absolute lymphocyte count (ALC) in peripheral blood at diagnosis may be an independent prognostic factor of IPI for patients with diffuse large B-cell lymphoma (DLBCL). In the rituximab era, the U.S. National Comprehensive Cancer Network International Prognostic Index (NCCN-IPI) was developed to improve the risk stratification of DLBCL in comparison to the existing IPI. Therefore, the aim of this study was to clarify the impact of ALC at diagnosis on event free survival (EFS) and overall survival (OS) on analysis performed with factors included in NCCN-IPI.
Patients and methods: We retrospectively reviewed the ALC of 413 patients with newly diagnosed DLBCL treated with R-CHOP at our hospital between January 2005 and March 2013. Primary central nervous system lymphoma patients were excluded from this study. ALC was determined in all patients from complete blood count with differential white blood count at the time of diagnosis, and prior to therapy administration. EFS and OS were estimated according to the Kaplan-Meier method. Multivariate analysis was performed with the proportional hazard Cox model.
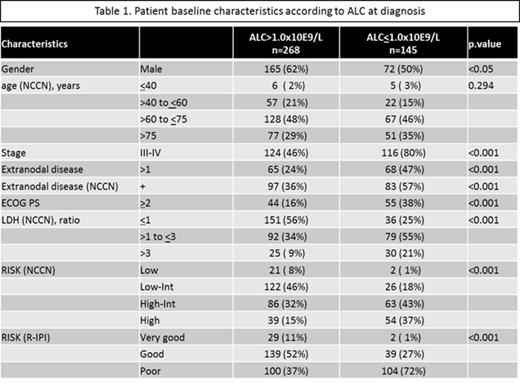
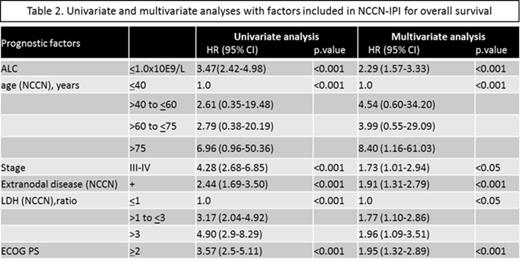
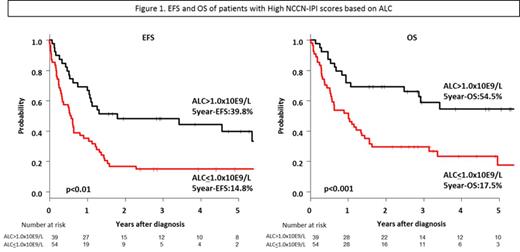
Results: The median ALC was 1.2x10E9/L (range, 0.06-9.0). We set an ALC cut-point at 1.0x10E9/L based on previous studies. The median follow-up duration was 40 months. Baseline characteristics according to ALC (<1.0x10E9/L[n=145] and >1.0x10E9/L[n=268]) are summarized in Table1. Patients with ALC<1.0x10E9/L had a significantly poorer EFS and OS than patients with ALC>1.0x10E9/L (5-year EFS, 37.0% versus 68.9%, p<0.001; 5-year OS, 46.3% versus 80.0%, p<0.001). On multivariate analysis performed with factors included in IPI and NCCN-IPI, ALC remained an independent predictor of EFS (IPI: hazard ratio [HR] 1.95; 95% confidence interval [CI] 1.43-2.68; p<0.001, NCCN-IPI: HR 1.94; 95%CI 1.42-2.65; p<0.001) and OS (IPI: HR 2.35; 95%CI 1.61-3.42; p<0.001, NCCN-IPI: HR 2.29; 95%CI 1.57-3.33; p<0.001) (Table2). Importantly, within the poor R-IPI group, ALC distinguished patients with different 5-year EFS (24.4% versus 50.4%, p<0.001) and OS (35.7% versus 65.7%, p<0.001). For the high NCCN-IPI group also, ALC distinguished patients with different 5-year EFS (14.8% versus 39.8%, p<0.01) and OS (17.5% versus 54.5%, p<0.001) (Figure1).
Conclusions: According to our results, ALC<1.0x10E9/L is an adverse prognostic factor and independent of IPI and NCCN-IPI. ALC might be more successful in identifying high-risk patients in which IPI and NCCN-IPI analysis was unrevealing. Our results suggest that other therapeutic strategies may be more effective in high-risk patients with DLBCL.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal