Abstract
Background: The Revised International Prognostic Scoring System (R-IPSS) stratifies MDS patients better than the original IPSS scoring system. Although RBC-transfusion dependency (RBC-TD) is associated with poor prognosis, it is not included in the R-IPSS. Another limitation of R-IPSS is that it is designed to assess the prognosis of patients only at the time of diagnosis; it does not provide prognostic guidance during the disease course. We hypothesise that the use of RBC-transfusion dependency status as a time-varying covariate improves R-IPSS.
Aim: To assess the impact of RBC-TD as a time-varying covariate in addition to R-IPSS in predicting survival outcome of MDS patients.
Materials and Methods: To match the patient selection criteria as in R-IPSS, primary MDS patients, AML (blast 20-30%) and CMML (WBC≤12x109/L) not treated with disease modifying agents or stem cell transplantation were included. RBC-TD was defined as RBC transfusion of at least 1 unit/8 weeks for at least 4 months (Malcovati et al; JCO 2007). For the statistical analysis of overall survival (OS) measured in months since diagnosis, the Akaike Information Criterion (AIC) was used to assess the goodness-of-fit of a model. Landmark analyses at 6, 12 and 24 months after the diagnosis were also conducted; individuals who experienced the event (i.e. death) before the landmark time point were excluded. The remaining patients were then classified into two groups – RBC-TD noted at or before the landmark time point and transfusion independent at the landmark time point. Results: In our study, 295 patients met the inclusion criteria for analysis, their median age was 75 years (21-97 years) and 66% patients were male. The majority of patients were RCMD, RAEB1 and RAEB2. R-IPSS improved the risk stratification of MDS patients, predominantly for the IPSS-intermediate group (Table I). The median OS in R-IPSS Very Low, Low, Intermediate, High and Very High risk group was 87, 62, 28, 13 and 12 months respectively (p<0.001). Median OS was significantly inferior in male patients (42.4 vs. 63.9 months; p<0.001) compared to females and elderly patients (129, 51 and 33 months in patients <60, 60-80 and >80 years respectively).
Of the 295 patients, 22 patients died and 1 lost-to-follow-up within four months of diagnosis; they did not complete the four months qualifying period for RBC-TD and hence were excluded from further analysis. Of the models tested, the four factor model which included R-IPSS, RBC-TD as a time-varying covariate, age and sex was best supported. RBC-TD (HR 5.5; P<0.001) was associated with poor survival, independent of the R-IPSS category, sex and age at diagnosis (Table 2).
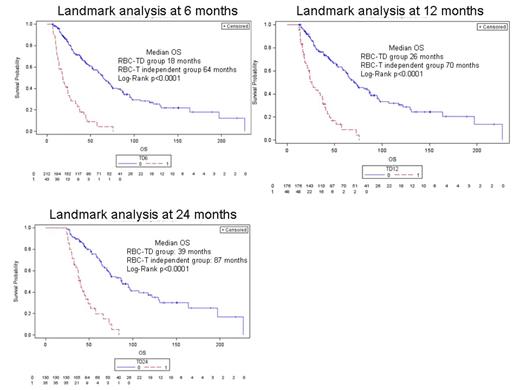
At each land mark analysis RBC-TD was associated with poor survival, independent of R-IPSS, age and gender. The median survival of patients who became RBC-TD by 6 months was significantly poorer than patients who remained RBC-transfusion independent (18 vs.64 months; p<0.001; Fig 1A). Similarly median OS was significantly poorer in patients who became RBC-TD by 12 months (26 vs.71 months; p<0.001; Fig 1B) and 24 months (40 vs. 87 months; Fig.1C)
Conclusions: Majority of MDS patients become progressively cytopaenic and require RBC transfusion during the disease course. RBC-transfusion dependency is always associated with poor prognosis irrespective of time to become RBC-TD. Assessing RBC-TD status along with R-IPSS provides more precise prognostic information during the disease course.
Refinement of IPSS patient risk categories by R-IPSS scoring system
| . | R-IPSS . | ||||
|---|---|---|---|---|---|
| IPSS | Very Low | Low | Intermediate | High | Very High |
| Low (n=126; 43%) | 60 | 64 | 2 | 0 | 0 |
| Intermediate1 (n=121; 41%) | 8 | 54 | 45 | 14 | 0 |
| Intermediate-2 (n=33; 11%) | 0 | 0 | 7 | 16 | 10 |
| High (n=15; 5%) | 0 | 0 | 0 | 4 | 11 |
| Total=295 | 68 23% | 118 40% | 54 18% | 34 11.5% | 21 7% |
| . | R-IPSS . | ||||
|---|---|---|---|---|---|
| IPSS | Very Low | Low | Intermediate | High | Very High |
| Low (n=126; 43%) | 60 | 64 | 2 | 0 | 0 |
| Intermediate1 (n=121; 41%) | 8 | 54 | 45 | 14 | 0 |
| Intermediate-2 (n=33; 11%) | 0 | 0 | 7 | 16 | 10 |
| High (n=15; 5%) | 0 | 0 | 0 | 4 | 11 |
| Total=295 | 68 23% | 118 40% | 54 18% | 34 11.5% | 21 7% |
Factors Predicting Survival of Primary Untreated MDS Patients
| Factor . | Hazard Ratio . | P value (Chi Sq) . |
|---|---|---|
| Age at diagnosis (Unit = 1 year) | 1.04 | <0.001 |
| Sex (Male) | 1.99 | <0.001 |
| R-IPSS Low (Ref Level = Very Low) | 1.46 | 0.106 |
| R-IPSS Int | 3.23 | <0.001 |
| R-IPSS High | 4.03 | <0.001 |
| R-IPSS Very High | 7.72 | <0.001 |
| Transfusion Dependency as a Time Varying Covariate | 5.50 | <0.001 |
| Factor . | Hazard Ratio . | P value (Chi Sq) . |
|---|---|---|
| Age at diagnosis (Unit = 1 year) | 1.04 | <0.001 |
| Sex (Male) | 1.99 | <0.001 |
| R-IPSS Low (Ref Level = Very Low) | 1.46 | 0.106 |
| R-IPSS Int | 3.23 | <0.001 |
| R-IPSS High | 4.03 | <0.001 |
| R-IPSS Very High | 7.72 | <0.001 |
| Transfusion Dependency as a Time Varying Covariate | 5.50 | <0.001 |
Landmark analysis for OS according to RBC-transfusion dependency (RBC-TD): Patients were classified according to transfusion dependency at 6, 12 and 24 months. At all three land mark analysis time-points median OS of RBC-TD patients was significantly inferior compared to patients who remained independent
Landmark analysis for OS according to RBC-transfusion dependency (RBC-TD): Patients were classified according to transfusion dependency at 6, 12 and 24 months. At all three land mark analysis time-points median OS of RBC-TD patients was significantly inferior compared to patients who remained independent
Hiwase:Novartis pharmaceutical Ltd , Australia: Research Funding. Ross:Novartis: Honoraria, Research Funding; BMS: Honoraria. Reynolds:Novartis AG: Former Novartis AG employee and holder of Novartis AG stock Other.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal