Abstract
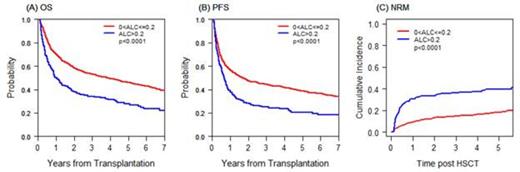
To determine the impact of absolute lymphocyte count (ALC) recovery on clinical outcome after allogeneic hematopoietic stem cell transplantation (HSCT) and to determine the threshold value of ALC, we conducted a retrospective study of 1109 adult patients who underwent a first allogeneic HSCT from 2003 through 2009, excluding patients who died or relapsed before D30. The median age was 51 years (range: 18-74) with 52% undergoing reduced intensity HSCT and 48% myeloablative intensity HSCT with T-replete PBSC (93.7%) or marrow (6.4%) grafts; 41% receiving HLA-matched related donors, 51% HLA-matched unrelated donors, and 8.5% HLA-mismatched transplantation. The median follow-up time was 6 years (range: 2.5 – 9.8 years). To determine the threshold value, we randomly split the entire cohort into a training set and a validation set in a 1:1 ratio stratified by conditioning intensity, and then applied a restricted cubic spline (RCS) smoothing method to obtain relative hazard estimates of the relationship between ALC at 1 month and log hazard of progression-free survival. Based on this approach, ALC was categorized as low (≤0.2x 109 cells/L) or normal (>0.2x109 cells/L). For patients with low ALC at 1, 2, or 3 months after HSCT, excluding relapse or death prior to each time point to rule out the direct influence of relapse on the ALC, the overall survival (OS) (p≤0.0001) and progression-free survival (PFS) (p≤0.0002) were significantly lower and non-relapse mortality (p≤0.002) was significantly higher compared to patients with ALC >0.2x109 cells/L at each timepoint, but there was no difference in relapse. Since patients with newly low ALC at 2 or 3 months post HSCT had equally poor outcome as those whose ALC was low at 1 month post HSCT, we combined patients who had low ALC at 1, 2 or 3 months post HSCT and compared their outcome to that of patients who had ALC>0.2x109 cells/L at 1, 2, and 3 months after HSCT. The 5-year OS for patients with low ALC was 28% vs 46% for patients without low ALC (p<0.0001); the corresponding 5-year PFS were 21% vs 39%, p<0.0001 and NRM 40% vs 18%, p<0.0001 (Figure A-C). This result was consistent when other prognostic factors, including occurrence of grade II-IV acute GVHD, were adjusted for in multivariable Cox models stratified by conditioning intensity: HR for OS was 1.52 , p≤0.0001; for PFS, 1.42, p=0.0008; and for NRM, 2.4 p<0.0001 for patients with low ALC within 3 months of HSCT. Low ALC was not significantly associated with relapse (HR 1.01, p=0.92) in the multivariable model. Low ALC early after HSCT is an independent risk factor for increased NRM and poor survival independent of grade II-IV acute GVHD. ALC assessment early after HSCT may be useful to identify high-risk patient cohorts that may benefit from additional therapeutic interventions.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal