Abstract

Introduction
Allogeneic stem cell transplantation for older individuals with hematologic malignancies has been performed with a reduced-intensity conditioning (RIC) regimen due to lower treatment-related mortality (TRM) associated with this approach; however, the optimal conditioning regimen for these individuals remains unclear.
Methods
We analyzed 163 patients, 55 years or older with hematologic malignancies (127 AML/MDS, 19 lymphoma, 11 ALL, 6 other) who underwent 1st allo-HSCT with fludarabine-melphalan-based conditioning between 01/2000-04/2014. All patients achieved complete remission (CR) at the time of transplant (13 patients were beyond 2nd CR). Donors were HLA matched related (MRD), matched unrelated (MUD), and mismatched (related and unrelated) (MMD) in 56 (34.3%), 65 (39.8%) and 42 (25.7%) patients respectively. Patients received fludarabine 120 mg/m2 plus either melphalan 100 mg/m2 (FM100; 61 patients) or melphalan 140 mg/m2 (FM140; 102 patients). Patients who received mismatched transplants received also thiotepa 5-10 mg/kg or 2 Gy TBI. There was no statistical difference between characteristics of the two groups except more patients in the FM100 group received marrow stem cells (62.3% vs 33.3%, p<0.001).
Results
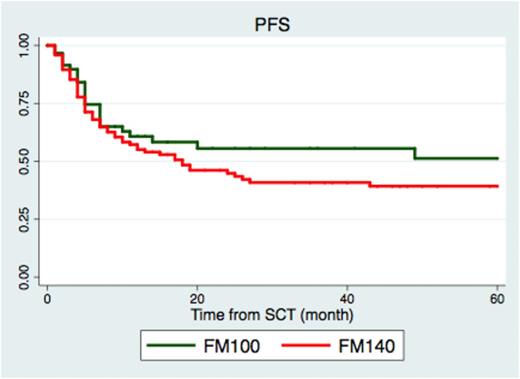
Median age was 62 years (range 55-76 years) (63 years in FM100 vs 62 years in FM140 group, p=0.458). Median follow-up for 82 survivors was 36.5 months. Of 163, 155 patients engrafted (98.4% in FM100, 93.1% in FM140, p=0.385) with median time to neutrophil and platelet engraftment of 12 days and 15 days, respectively. All of these 155 patients remained in continuous CR at 3 months post-transplant. Treatment-related mortality (TRM) at day 100 and 1 year of the entire cohort was 11.3% and 25.9%, respectively. Comparing the FM100 with the FM140 group, TRM at 1 year was 20.4% vs 26.9% (p=0.046); cumulative incidence (CI) of relapse at 3 years was 29.4% vs 35.4% (p=0.491); 3-year OS was 59.5% vs 42.3% (p=0.012); 3-year PFS was 54.6% vs 38.9% (p=0.024) (Figure1); CI of acute GVHD all grades was 23.2% vs 35.7% (p=0.039) while CI of acute GVHD grade2-4 was 15.3% vs 22.8% (p=0.024). There was no significant difference in chronic GVHD (40.1% vs 43.7%, p=0.745) or chronic extensive GVHD (20.5% vs 25.1%, p=0.356).
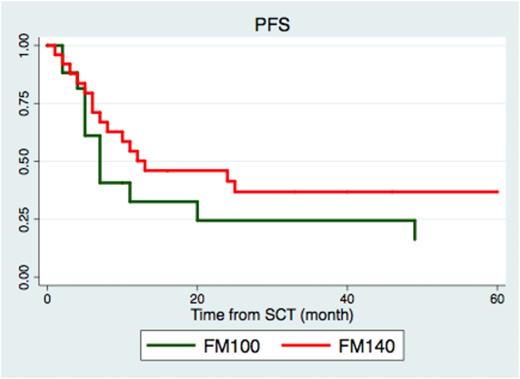
In subgroup analysis of 46 patients with high-risk cytogenetics AML/MDS, FM140 was associated with better PFS compared with FM100; 3-year PFS was 32.9% vs 16.3% (p=0.046) (Figure2). The better PFS resulted from lower relapse rate (3-year CI of relapse was 29.2% in FM140 vs 53.8% in FM100 group, p=0.039) while TRM was not different (1-year TRM 20.5% in FM140 vs 21.7% in FM140 group, p=0.876).
Factors associated with poor PFS in univariate analysis were high-risk cytogenetics, transplant in beyond 1st CR, and grade 2-4 acute GVHD while using FM100 and MRD associated with a better PFS. However, only high-risk cytogenetics (HR 1.69, 95%CI 1.04-2.74, p=0.031), FM100 (HR 0.74, 95%CI 0.53-0.91, p=0.048), and acute GVHD grade 2-4 (HR 1.57, 95%CI 1.01-2.46, p=0.048) retained their statistical significance in multivariate analysis.
Conclusions
Allo-HSCT with reduced doses of melphalan (FM100) is associated with improved survival in elderly patients with hematologic malignancies due to lower TRM in this group. Patients with high-risk cytogenetics AML/MDS appear to have better survival with more intense conditioning (FM140) due to lower relapse rate. These results suggest that a differential approach should be applied to transplant conditioning, not only based on age but also based on disease type, and provide the basis for a future personalized approach for transplant conditioning in hematopoietic stem cell transplantation.
Progression free survival of patients with high risk cytogenetics AML/MDS
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This icon denotes a clinically relevant abstract

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal