Abstract
Introduction:
The treatment strategy for diffuse large B-cell lymphoma (DLBCL) in elderly patients is problematic. Recently, the Comprehensive Geriatric Assessment (CGA) has been proposed as an objective tool to identify those who can safely tolerate curative treatment. Although several researchers have reported the effectiveness of CGA in patients with aggressive B-cell non-Hodgkin lymphoma and revealed that intensive treatment cannot improve the outcomes of patients identified by CGA as unfit, compared with palliative treatment, the effectiveness of CGA and the effects of treatment are not firmly established. In the present study of elderly patients, we evaluated clinical outcomes and the prognostic value of clinical and biological parameters, including CGA stratification and treatment.
Methods:
We conducted a retrospective analysis using a database at our hospital. Patients were eligible if aged 60 years or older and diagnosed with DLBCL between November 1, 2000 and August 31, 2013. CGA stratification was performed using medical records, including assessment of the following four parameters: 1) age >= 80 years; 2) ADL including bathing, dressing, toileting, transferring, feeding, and continence; 3) comorbidity score according to the Cumulative Illness Rating Score for Geriatrics (CIRS-G) and evaluated for all organs/systems as follows: no problem – 1, mild problem – 2, moderate disabilities or morbidities (requiring treatment) – 3, severe and significant chronic disabilities – 4, and extremely severe disabilities – 5 ; and 4) geriatric syndrome, defined as the occurrence of dementia, delirium, depression, incontinence, falls, osteoporosis, neglect and abuse, or failure to thrive. Patients were classified as "fit" if they were aged <80, had a normal ADL score, fewer than three grade 3 CIRS-G comorbidities and no grade 4 comorbidities (except hematological comorbidities), and absence of geriatric syndrome. All other patients were classified as "unfit".
We classified treatment as CHOP+-R, THP-COP+-R (THP-COP: pirarubicin 30 mg/m2, cyclophosphamide 500 mg/m2 and vincristine 1 mg/m2 on day 1 and predonisolone 30 mg/day on days 1–5), surgery alone, and palliative therapy (radiation, low-dose chemotherapy, rituximab alone, and corticosteroids). We compared overall survival (OS), progression free survival (PFS), complete response rate (CRR) and overall response rate (ORR) with each CGA stratification and treatment.
Results:
87 patients were identified, with a median age of 72 years (range 60–84), 59% >= 70 years, and 16% >= 80 years; 53% male; 67% Stage III/IV; 62% IPI high–int/high, 20% loss of ADL and 13% geriatric syndrome. 70% were CGA fit and 30% unfit. 39% were treated with CHOP+-R, 53% THP-COP+-R, 2% surgery alone, 6% palliative therapy and 84% received rituximab. Median observation time was 859 days (range 40–4955).
Univariate analysis showed the parameters negatively affecting OS were: loss of ADL (p<0.01), albumin < 3.5 mg/dl (p=0.03), CGA unfit (p=0.04), IPI high–int/high (p<0.01), PS 2–4 (p=0.02). On multivariate analysis, loss of ADL (HR 3.60, 95% CI [1.37, 9.42], p<0.01) and IPI high–int/high (HR3.30, 95% CI [1.06, 10.31], p=0.04) were independent baseline factors affecting OS.
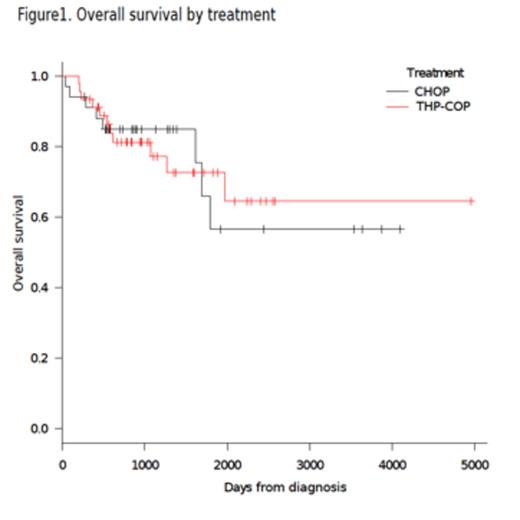
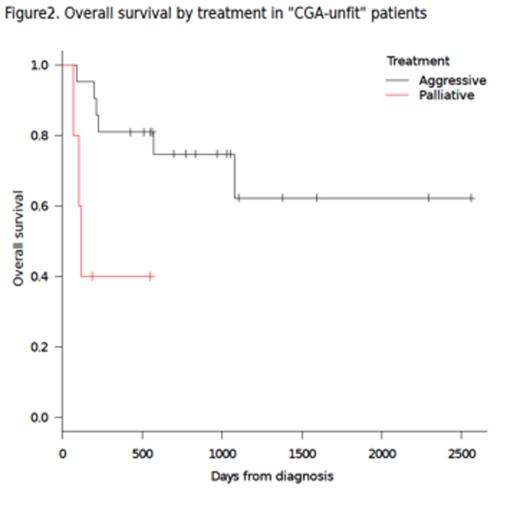
At five years, the outcomes of the patients treated with CHOP+-R and THP-COP+-R were similar in terms of OS (85.0% vs 77.2%; p=0.95), see figure 1, PFS (56.4% vs 66.9%; p=0.96), CRR and ORR. The patients treated aggressively (CHOP or THP-COP +- R) had significantly better OS, PFS, CRR and ORR compared with those receiving palliation. We also observed better outcomes in terms of OS (p<0.01), see figure 2, PFS (p<0.01), CRR (p=0.04) and ORR (p<0.01) among unfit patients treated aggressively, when compared to those receiving palliation. Although fit patients showed significantly better OS (p=0.04), PFS (p<0.01), CRR (p<0.01) and ORR (p<0.01) compared with unfit patients, both groups of patients were similar regarding OS (p=0.23), PFS (p=0.07) and ORR (p=0.23), excepting CRR (p=0.01) among patients treated aggressively.
Conclusions:
In this study, we observed similar outcomes regarding OS and PFS between two aggressive treatments (CHOP or THP-COP +- R). The patients treated aggressively had significantly better outcomes compared to those receiving palliation, irrespective of CGA stratification. Intensive treatment should be considered even for unfit patients.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal