Abstract
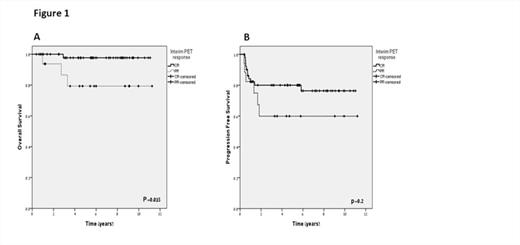
Patients with advanced stage Hodgkin Lymphoma (HL) and high international prognostic score (IPS≥3), treated with ABVD, have low freedom from progression, estimated as 60-65% at 5 years. Six cycles of escalated (esc) BEACOPP significantly improved the outcome of patients with advanced stage HL with progression free survival (PFS) of 90% and overall survival (OS) of 95% at 5 years. However, 6 cycles of escBEACOPP are associated with significant hematological toxicity and infections, as well as late adverse effects, such as increased incidence of myelodsysplastic syndrome (MDS), acute myeloid leukemia (AML) and infertility. In this retrospective study we analyzed the survival outcome of poor risk advanced stage HL patients who were treated with response- adapted therapy, tailored by the results of early interim FDG-PET/CT scans, after the initial 2 cycles of escBEACOPP. After complete or partial responses were obtained with this regimen, treatment was then de-escalated to 4 cycles ABVD. A total of sixty nine patients were evaluated, 45 of whom participated in the multicenter phase II prospective study which was conducted between 2001 and 2007 (Avigdor et al, Ann Oncol. 2010). The current study includes analyses of long term outcome of the former group, as well as the outcome of an additional 24 consecutive patients who were treated with the same protocol at Sheba Medical Center since the termination of the prospective study. The response and survival outcomes were defined according to the revised response criteria for malignant lymphoma. Scans were scored as positive or negative based only on visual assessment, according to guidelines adopted by the International Harmonization Committee. Survival was calculated with the Kaplan-Meier method and survival comparison was analyzed with the Log-Rank test. Forty five (65 %) were males and median age was 30 years (19-59). The most frequent subtype of HL was nodular sclerosis (78%). Four patients (6%) had unfavorable stage IIB, 12 (17%) had stage III and 53 (77%) had stage IV disease. Nine patients (13%) had an IPS <3, the remaining 60 patients (87%) had 3 or more IPS risk factors. Four patients received involved field radiotherapy with 30 Gy to the initial site of bulky mediastinum, after completion of chemotherapy. After a median follow-up of 5.6 years (0.4-11), 4 patients (6%) have died: 2 due to advanced HL, 1 from catastrophic APLA syndrome and 1 from lung carcinoma; the latter 2 patients were in complete response (CR). After the initial 2 cycles of escBEACOPP,52(75%) patients were in CR and 17 (25%) achieved partial response (PR). Five-year OS for the entire cohort was 93%. Importantly, OS was predicted by the results of the early-interim PET/CT scans: patients in CR had OS of 98% while those in PR had OS of 79% at 5 years (Figure 1A, p=0.015). Seventeen patients (25%) relapsed or progressed. Five-year PFS for the entire cohort was 76%, median PFS was not reached. Early-interim PET/CT results did not predict PFS at 5 years (80% for patients in CR and 60% for patients in PR, Figure 1B, p=0.2) most probably due to small sample size. The presence of extranodal disease or bulky mediastinal mass (≥10 cm on CT scan) did not predict treatment failure. As expected, grade 3-4 acute hematological toxicity was more frequent during the first 2 cycles of escBEACOPP than in the comparable ABVD phase. There was no treatment related mortality, and until now no cases of AML or MDS have been encountered. In conclusion, the current retrospective analysis indicates that combined escBEACOPP-ABVD therapy is well tolerated and certainly less toxic than 6 cycles of escBEACOPP. In patients receiving escBEACOPP-ABVD regimen, negative early-interim PET activity reliably predicted an excellent outcome, while a positive result partly identified patients with a worse prognosis. Based on relatively long follow-up data, it appears that high risk advanced HL patients, who achieve early metabolic CR (after 2 cycles of escBEACOPP), have a favorable outcome after de-escalating therapy to the less toxic ABVD regimen.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal