Abstract
Background:
Molecular profiling has revolutionized the field of hematology, and in particular myeloid neoplasms. NPM1+/FLT3- mutational status has been shown to have a favorable prognostic impact in patients with acute myeloid leukemia (AML). However, little is known about its interaction with age.
Methods:
We retrospectively analyzed the overall survival (OS) in newly diagnosed AML patients, whose FLT3 and NPM1 data were available, and were treated with cytotoxic chemotherapy at our institution between 2003 and 2013. Patients 18 to 60 years of age were categorized as adult, and those above 60 years were classified as elderly. Each of the elderly or adult groups were further divided according to the presence or absence of combined NPM1+/FLT3- mutational status. Estimated probabilities of overall survival were calculated using the Kaplan-Meier method, with the log-rank test to compare groups. Demographics and continuous variables were compared using the Wilcoxon rank sum test. Appropriate IRB approval was obtained.
Results:
Out of 835 patients with AML, 86 patients with both known FLT3/NPM1 mutation status and receiving induction chemotherapy were found. NPM1+/FLT3- mutational status was present in 11 elderly (median age 68 yr, hemoglobin (Hb) 8.7 g/dL, white blood cells (WBC) 9.6 x109/L, platelets (PLT) 100 x109/L, peripheral blood blasts percentage (PB%) 31), and in 11 adult patients (median age 49 years, Hb 9.1 g/dL, WBC 14 x109/L, PLT 67 x109/L, and PB% 21). Twenty-eight elderly patients (median age 66 yr, Hb 9.4 g/dl, WBC 15.7 x109/L, PLT 66 x109/L, and PB% 33), and 36 adult patients (median age 49 years, Hb 9.1 g/dL, WBC 14 x109/L, PLT 67 x109/L, and PB% 21) were carrying genotypes other than NPM1+/FlT3-. There was no statistical significant difference in the median age, Hb, WBC, PLT, and PB% at the time of diagnosis. Out of 86 patients, 79 had intermediate, 6 had adverse, and 1 had favorable cytogenetic risk. All elderly and adult patients with NPM1+/FLT3- genotype had intermediate risk cytogenetics.
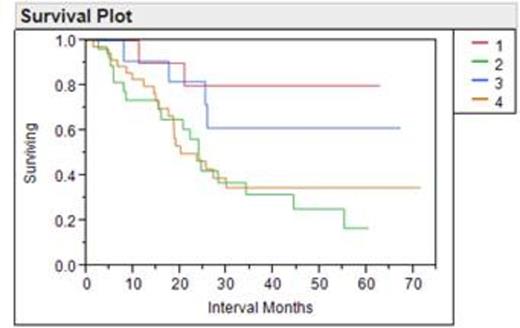
When treated with cytotoxic chemotherapy, elderly patients with NPM1+/FLT3- genotype demonstrated a significantly better overall survival compared to elderly patients without this genotypes (p=0.015), and interestingly also to adult AML carrying other genotypes (p=0.028). Surprisingly, there was not an improved survival in adults with NPM1+/FLT3- genotype compared to adults carrying other genotypes (p=0.14), but this may have been related to the small numbers in each group. No significant difference in the overall survival was observed between elderly and adult patients who were carrying NPM1+/FLT3- mutational status (p=0.4). The estimated 5-year survival rates for elderly with and without NPM1+/FLT3- status were 71% vs. 14%, and for adults with and without this genotype were 49% vs. 19%, respectively.
Conclusion:
Age does not have an impact on the OS in AML patients with NPM1+/FLT3- mutational status, arguing strongly for intense chemotherapy in this group. Elderly AML patients with NPM1+/FLT3- genotype have a superior OS compared to both adult and elderly patients carrying other genotypes, when treated with cytotoxic chemotherapy. Further validation in large prospective studies is warranted.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal